Key takeaways:
~ The low FODMAPs diet works for many people with IBS, but it doesn’t work for everyone.
~ Instead of a FODMAPs problem, some people diagnosed with IBS have genetic variants that reduce the activity of the sucrase-isomaltase (SI) enzyme. This causes impaired digestion of sugars and starch.
~ Check your genetic data to see if your root cause could be SI enzyme deficiency.
What if a low FODMAPs diet doesn’t work?
The low FODMAPs diet is often recommended as a starting point for anyone with gas, bloating, diarrhea, constipation, and other symptoms of IBS. Often, people describe the diet in such a way that you think it’s THE solution for everyone — people absolutely swear by it, there are Facebook groups for support, and many doctors recommend it as a place to start for IBS symptoms.
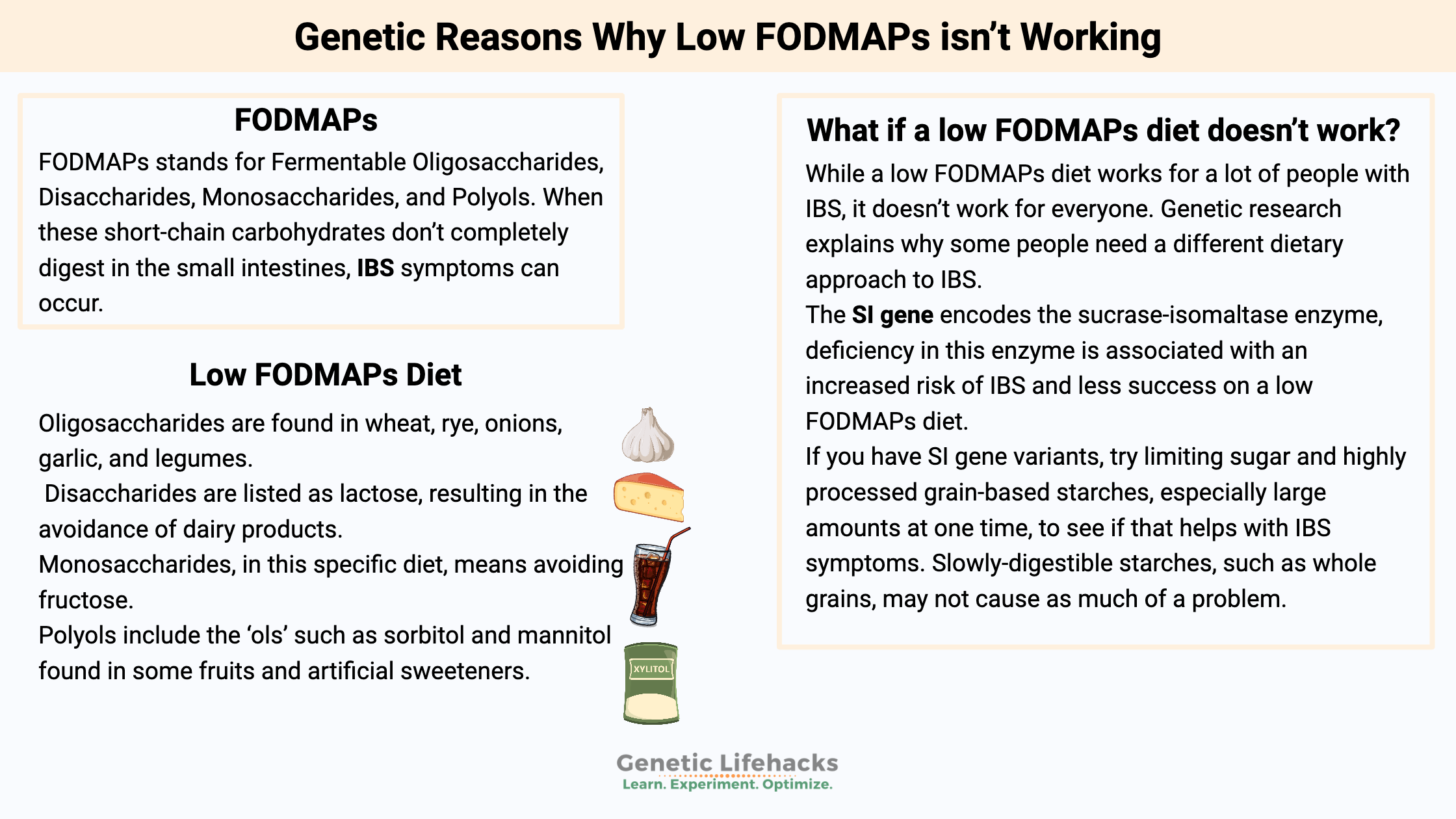
While a low FODMAPs diet works for a lot of people with IBS, it doesn’t work for everyone. Genetic research explains why some people need a different dietary approach to IBS.
Irritable bowel syndrome (IBS) has multiple causes, and a one-size-fits-all dietary solution is unlikely to work for everyone.
What are FODMAPs?
FODMAPs stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. When these short-chain carbohydrates don’t completely digest in the small intestines, IBS symptoms can occur. Bacteria in the large intestines can ferment undigested carbohydrates, causing bloating and other problems.
Let’s break down the low FODMAPs diet with some examples:
Oligosaccharides are fructans and GOS (galactooligosaccharides). They are found in wheat, rye, onions, garlic, and legumes. Disaccharides are listed as lactose, resulting in the avoidance of dairy products. Avoiding monosaccharides, in this specific diet, means avoiding fructose, while polyols include the ‘ols’ such as sorbitol and mannitol found in some fruits and artificial sweeteners.[ref]
| FODMAP Type | Example Foods | Avoid On Diet? |
|---|---|---|
| Oligosaccharides | Wheat, rye, onions, garlic, legumes | Yes |
| Disaccharides | Dairy (lactose) | Yes |
| Monosaccharides | Fruits with fructose (apples, pears, honey) | Yes |
| Polyols | Certain fruits (apples, plums), artificial sweeteners | Yes |
The low FODMAPs diet cuts out many of the IBS problem foods, such as those including lactose or fructose, so it works for a lot of people.
But what if the specific FODMAPs carbohydrates aren’t your problem? It turns out that there are multiple causes of not being able to break down foods. You could be a champ at digesting lactose, and fructose could be fine for you…
Another cause of IBS is decreased sucrase-isomaltase
Researchers have found that SI insufficiency is one cause of irritable bowel syndrome.
SI stands for the sucrase-isomaltase enzyme produced in the small intestines to break down sugar and starches. Sucrase is the enzyme for breaking down sucrose (e.g., table sugar). Isomaltase breaks down maltose, which is a disaccharide from grains and starches.
Congenital sucrase-isomaltase deficiency (CSID) is an uncommon genetic disease caused by severe mutations in the SI gene. Usually diagnosed in infants when they start eating solid foods or drinking fruit juices, the severe deficiency of sucrase-isomaltase is a serious issue that causes babies to have bloating, pain, and watery diarrhea.
CSID, an autosomal recessive genetic disease, means two copies of a non-functioning mutation in the gene are required. It’s the worst-case scenario, and kids diagnosed with it are on a sugar and starch-restricted diet throughout childhood. CSID can improve somewhat as kids get older and their small intestine grows.
The prevalence of CSID varies by population group, with up to 1 in 500 Caucasians affected. Rates are lower in people of African descent, but indigenous populations of Alaska, Canada, and Greenland have higher rates of up to 1 in 10 with CSID.[ref]
Breaking down starches:
Sucrase-isomaltase is a dual-function enzyme, breaking down sucrose into glucose and fructose, as well as breaking down certain starches into glucose.
It’s fairly easy to figure out which foods have sucrase in them — sweet fruits and anything with added sugar.
But the ‘isomaltase’ component of SI is slightly more complicated.
When you eat foods that contain starch, digestion begins in the mouth with salivary amylase (an enzyme for breaking down starch). Not all starch breaks down in the mouth, of course. Also, the pancreas secretes amylase into the small intestines to break apart starch molecules there. The broken-down starch molecules then need to undergo one more enzymatic reaction to turn them into simple sugars for absorption. The sucrase-isomaltase enzyme handles about 60-80% of starch digestion in the small intestines. The other 20-40% breaks down by another enzyme called maltase-glucoamylase.[ref]
What happens with partial sucrase-isomaltase deficiency?
It turns out that people with genetic variants or single mutations that decrease the sucrase-isomaltase enzyme are quite a bit more likely to be diagnosed with IBS.[ref][ref] A decreased production of the sucrase-isomaltase enzyme can combine with a diet high in starch or sugar to cause gas, bloating, diarrhea, and/or constipation.
Thus, for someone whose IBS is caused by low SI enzyme function, going on a low FODMAP diet may not be the whole solution.
Yes, a low FODMAP diet cuts down on some foods with starches and may give some relief, but a more tailored diet that slows the influx of sugar and starch may be a better option.
Research shows this to be true. A recent study in the British Medical Journal showed that IBS patients who carry SI gene variants are less likely to achieve IBS remission on the FODMAPs diet.[ref]
FODMAPs Diet Genotype Report:
Access this content:
An active subscription is required to access this content.
Lifehacks:
While there are multiple causes of IBS, if you have reduced SI enzyme, the best strategy is to limit sucrose and starch intake. Avoid overwhelming your digestion with large amounts of sugar or processed starches at once. Tracking your food intake and symptoms can help you find your optimal diet.
Here’s how:
Access this content:
An active subscription is required to access this content.
Related Articles and Topics:
Irritable Bowel Syndrome (IBS): Targeted Solutions Based on Your Genes
References: