Key takeaways:
- Borderline personality disorder (BPD) results from a combination of genetic susceptibility (40-60% heritability) and environmental triggers like childhood trauma. The genetic variants alone don’t cause BPD, but they increase vulnerability when combined with adverse experiences.
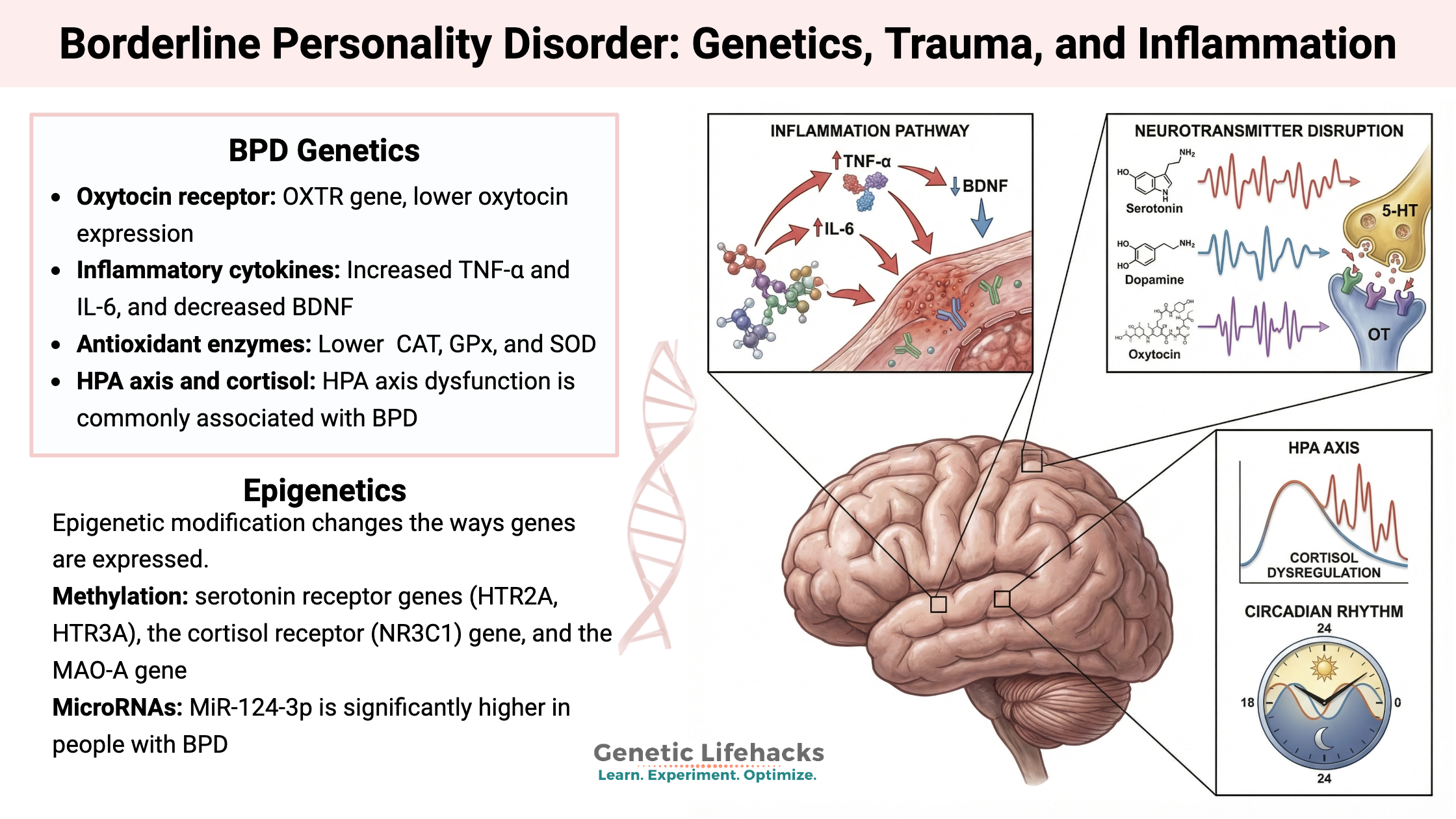
- People with BPD show increased inflammation and oxidative stress, with elevated cytokines like TNF-α and IL-6, plus lower antioxidant enzymes. This neuroinflammation disrupts serotonin synthesis and BDNF production, contributing to mood instability.
- Specific genetic variants in the serotonin, dopamine, oxytocin, and cortisol pathways affect BPD risk. These include variants in HTR2C, TPH2, ANKK1/DRD2, OXTR, and FKBP5 genes that alter neurotransmitter function and stress response.
- Circadian rhythm dysfunction plays a major role in BPD symptoms. Studies show that circadian phase delays, sleep-onset insomnia, and desynchronization correlate with impulsivity and mood instability.
What is Borderline Personality Disorder (BPD)?
Borderline personality disorder (BPD) is a mental illness that involves the inability to regulate emotions. There is a variety of symptoms, including:[ref][ref]
- Fear of abandonment
- Pattern of unstable and violent relationships
- Splitting, or seeing things/people as all good or all bad
- Emotional lability
- Impulsivity
- Frequent self-destructive and suicidal behavior
- Short-lived stress-related paranoid thoughts
- Identity issues
Studies estimate that just under 3% of the U.S. population meets the criteria for BPD. [ref]
Historical name:
The name borderline personality disorder dates back to the 1970s and referred to people who didn’t really fit into the diagnoses of psychosis or neurosis. It sits on the border between several conditions. Individuals were described as having a more primitive psychological defense mechanism to avoid anxiety.[ref]
Comorbidities:
BPD very often occurs along with other psychiatric disorders, such as anxiety disorders, depressive disorder, bipolar disorder, sleep disorders, or substance use disorders.[ref]
Genetics + Environment:
Genetics plays a role in BPD, but genes alone do not cause it. Instead, it is a combination of genetic susceptibility, epigenetic changes, and an environmental trigger such as childhood trauma, physical/sexual abuse, or a traumatic event such as a divorce.[ref]
Twin and family studies estimate the heritability of borderline personality disorder to be around 40-60% (genetics, epigenetics), with the rest being environmental.[ref][ref][ref]
Childhood trauma is often listed as an environmental factor. Traumatic events, adversity, or abuse during times when the brain is developing can cause long-term effects on the HPA axis and neurotransmitter production.[ref]
Genetic pathways involved in BPD:
The following genetic susceptibility pathways have been identified in studies as increasing the relative risk of borderline personality disorder.
Oxytocin receptor (OXTR gene):
Oxytocin is a hormone involved in mother-child bonding as well as social bonding and empathy. People with BPD, on average, show lower oxytocin expression. Studies on patients with BPD show that changes in the oxytocin receptor gene that reduce expression are likely to cause someone with BPD to feel more psychological pain and be more affected by childhood maltreatment.[ref] [ref]
Inflammatory cytokines:
Multiple studies show that people with BPD have increased oxidative stress, increased inflammatory cytokines (TNF-α and IL-6), and decreased BDNF.[ref][ref]
Inflammatory cytokines interfere with the synthesis and reuptake of key neurotransmitters, especially serotonin. Serotonin disruption may contribute to the severe mood swings and emotional instability characteristic of BPD. Cytokines also decrease the production of brain-derived neurotrophic factor (BDNF), which is important for neuroplasticity.
Antioxidant enzymes:
Two recent studies looked at the levels of antioxidant enzymes, including CAT, GPx, and SOD, and found that they were lower in people with BPD than in a healthy age-matched control group.[ref][ref]
Oxidative stress can trigger a cycle of inflammation through the activation of pathways like nuclear factor-kappa B (NFκB), causing neuroinflammation. This affects brain areas implicated in BPD symptoms, such as those involved in stress response, emotional processing, and behavioral control.
HPA (hypothalamus-pituitary-adrenal) axis and cortisol:
HPA axis dysfunction is commonly associated with BPD, but not everyone with BPD has altered cortisol levels. Studies link BPD to heightened vulnerability to stress — often with a blunted cortisol response to acute stress, but overall elevated cortisol output. This is especially true in those with a history of childhood trauma. This HPA axis dysregulation, characterized by a hypersensitive stress system, contributes to emotional instability, impulsivity, and difficulties with social cognition.[ref]
So what is the HPA axis? The hypothalamus is a region in the brain that controls the initial signal to the pituitary that then signals the adrenals to release cortisol. Researchers think that childhood trauma causes some people to have altered cortisol levels or altered timing of cortisol release, which persists through adulthood. This leads to changes in the response to stress in some people with BPD.
Note that not everyone with BPD has altered cortisol levels. Here’s what the studies show:
- In women with BPD, those with depression tended to have higher overnight cortisol, while those with comorbid PTSD did not.[ref]
- Another study that looked at both men and women with BPD found that only women had elevated waking cortisol levels. Women with BPD also had higher-than-normal testosterone levels in multiple studies.[ref][ref]
Thyroid:
Studies show that low thyroid levels may play a role in several types of mood disorders, including BPD. Interestingly, a recent Mendelian randomization study pointed to a genetic link between BPD and thyroid problems.[ref]
Epigenetics – Changes in Gene Expression:
A number of epigenetic changes have been identified in people with borderline personality disorder. Epigenetic modifications are thought to cause the sustained abnormalities of most mental disorders.[ref]
Epigenetic modification changes the ways genes are expressed, which is often explained as a gene being turned on or off, but is more akin to being turned up or down.
Two well-studied ways that epigenetic changes can occur are the methylation of genes and microRNAs acting on mRNA.
Methylation:
One way that gene expression can be changed is through a methyl group being added to the DNA in a place that prevents the gene from being translated into its protein. Multiple studies have shown methylation changes in the serotonin receptor genes (HTR2A, HTR3A), the cortisol receptor (NR3C1) gene, and the MAO-A gene. One study showed reduced methylation for an opioid receptor in people with BPD. Some studies indicate that these changes are attributed to traumatic events experienced during childhood.[ref][ref]
What does this mean? It means that changes in the serotonin, cortisol, or dopaminergic pathways that happen in response to an environmental factor, such as a traumatic event, can persist through adulthood.
Importantly, not all studies show epigenetic changes or methylation of these genes in borderline personality disorder. This is just one possible factor involved.
MicroRNAs:
MicroRNAs are short strands of RNA that can bind to an mRNA strand and prevent the translation into its protein. MiRNAs thus affect gene expression. Each miRNA can bind to hundreds of different mRNA strands and affect the gene expression of hundreds of genes, depending on the tissue.
For borderline personality disorder, specific microRNA changes have been identified. MiR-124-3p is significantly higher in people with BPD compared to a control group of psychiatric patients with other diagnoses. “miRNA miR-124-3p was implicated in the path from early life adverse events to BPD in adulthood through methylation analysis” [ref].
MiR-124-3p is highly abundant in the central nervous system and plays a role in schizophrenia and bipolar disorder, as well. It acts to downregulate GRIA2, a glutamate receptor, and ADRAB1, the beta-1 adrenergic receptor. GRIA2 may be key here. The AMPA glutamate receptors that lack the GRIA2 subunit have increased postsynaptic conductance, and downregulation of GRIA2 by miR-124-3p, therefore, may cause an increase in glutamatergic (excitatory) signaling in the brain.[ref]
Circadian rhythm:
The 24-hour circadian rhythm controls the expression of about 40% of genes. An altered or disrupted circadian rhythm can dramatically affect mood and cognitive function. In BPD, a circadian phase delay is often found, and sleep-onset insomnia is likely to be a problem. For example, impulsivity correlates with a lower circadian amplitude and lower stability between days. Mood instability is associated with delayed activity onset and decreased circadian amplitude.[ref]
Studies on body temperature patterns and heart rate changes indicate that individuals with BPD exhibit a desynchronization with their circadian rhythm.[ref]
Genotype report: Borderline Personality Disorder
Access this content:
An active subscription is required to access this content.
Lifehacks:
Various types of therapy are used to treat borderline personality disorder, such as cognitive behavioral therapy, metacognitive therapy, or dialectical behavioral therapy. A clinical trial also showed efficacy for ketamine.[ref][ref][ref]
Circadian rhythm optimization:
There’s a strong connection between circadian rhythm dysfunction and mood instability in borderline personality disorder. Studies using circadian optimization for BPD or depression patients show significant efficacy, especially when combined with other treatments:[ref][ref]
- Bright morning light (10,000 lux or more) reduces symptom severity
- Exposure to light in the blue wavelengths at night delays melatonin production, which is found in people with BPD. One way to optimize this is to shut off electronics (TV, phones, tablets) an hour before bedtime. Also, turn down bright overhead lights. An alternative is to wear amber-colored glasses that block all blue light.
- Exercise and consistent meal timing
Natural supplements for BPD:
The following supplements have been shown in studies to help some people with borderline personality disorder, but always talk with your health care provider before making changes or adding supplements, especially if you are on medications.
DHA and EPA:
A meta-analysis of studies showed that DHA and EPA (fish oil, krill oil) decreased the severity of BPD symptoms significantly. Studies used 1.2g to 2g per day.[ref][ref][ref] DHA and EPA are used by cells to synthesize the pro-resolving lipid mediators needed for the resolution of neuroinflammation.
Oxytocin:
A study found that multiple types of therapy helped to increase oxytocin levels, and the increase in oxytocin correlated with improved symptoms.[ref]
Intranasal oxytocin was shown in a small clinical trial to attenuate stress reactivity in people with BPD.[ref] Oxytocin in nasal spray form should be available from your doctor, or it may be available online in some places without a prescription.
L-tryptophan:
Case studies report that supplemental L-tryptophan improved depression symptoms in people with BPD.[ref] Tryptophan as an amino acid supplement is better absorbed and transported when consumed with carbohydrates. Foods high in tryptophan include cheese, poultry, egg whites, fish, milk, sunflower seeds, and pumpkin seeds.[ref]
Magnesium:
A 2015 study showed that RBC magnesium (magnesium in the cells) was low in people with BPD. Restoring adequate magnesium levels with supplementation reduced anxiety, depression, and sleep symptoms.[ref] Magnesium l-threonate is a form that may work better for crossing the blood-brain barrier.
Hormonal connections:
Multiple studies point to neuroendocrine disruptions in BPD. It may be worth testing (or talking to your doctor about testing) the following:
- 24-hour cortisol test to see if it is rising and falling at the right levels, right time of the day
- testosterone (tends to be high in women with BPD)
- thyroid hormone levels (connection to low thyroid in BPD)
Related articles
MAO-A and MAO-B: Neurotransmitter levels, genetics, and warrior gene studies
Glutamate: Synthesis, transport, and supplement interactions
Is Inflammation Causing Your Depression and Anxiety? The Science Behind the Link
References: