Key takeaways:
~ For some people, acetaminophen can cause liver damage when used at higher doses or with chronic use.
~ Genetic variants interact with acetaminophen in the risk of liver damage. Variants in CD44, CYP3A5, UGT1A9, UGT1A1, UGT2B15 impact risk.
~ Factors such as alcohol use, chronic illness, low glutathione, infancy, and older age can also increase risk.
~ Understanding your genetic risk, along with lifestyle factors, can help you decide which pain reliever may be the best choice for you.
Members will see their genotype report below, plus additional solutions in the Lifehacks section. Consider joining today.
Acetaminophen, liver and organ damage, and genes:
Acetaminophen, commonly known by the brand name Tylenol or as paracetamol in Europe, is a widely used over-the-counter medication for pain and fever reduction.
There are still some questions about how exactly acetaminophen works to reduce pain and fever, but in general, it acts on the prostaglandin system in a way that is separate from how aspirin and ibuprofen work. By inhibiting COX2, acetaminophen blocks prostaglandin G2 production, reducing pain and fever but with less of an anti-inflammatory effect. A metabolite of acetaminophen also acts on the TRPV1 and TRPA1 receptors to decrease pain.[ref]
While generally safe when taken as directed, higher doses of acetaminophen can lead to severe liver damage and potentially fatal liver failure. In fact, acetaminophen-related liver damage is currently the most common cause of liver transplant in the US, with more than 56,000 emergency room visits per year from acetaminophen-related liver problems. Along with liver damage, acetaminophen in excess will induce kidney injuriy.[ref][ref]
In this article, we’ll explore the research on how acetaminophen is broken down in the body, why liver damage occurs with acetaminophen use, and why genetic variants can increase the risk of liver damage at levels that most people can handle. I’ll also touch on why acetaminophen use in pregnancy and infancy may cause problems due to the infant’s immature detoxification system.
Metabolism (breakdown) of acetaminophen:
When you take acetaminophen, it is easily and rapidly absorbed in the intestines and then transported to the liver for processing.
| Step | Enzyme / Pathway | Effect on Acetaminophen | Genetic Influence / Note |
|---|---|---|---|
| Sulfation | SULT enzymes | Safe excretion | SULT1E1 variants: reduced efficiency, higher liver enzymes |
| Glucuronidation | UGT (UGT1A9, UGT1A1, UGT2B15) | Safe excretion | UGT1A9/UGT2B15 variants: lower clearance, higher NAPQI |
| Oxidation | CYP2E1, CYP3A5 | Creates toxic NAPQI | CYP2E1 upregulated by alcohol; CYP3A5 variants: increased risk |
| Detoxification | Glutathione (GST) | Neutralizes NAPQI | Low glutathione (genetics, age, disease): higher risk |
Sulfation and glucuronidation:
Most of the acetaminophen will be metabolized through conjugation reactions using the SULT and UGT enzymes. The SULT family of enzymes drives conjugation with sulfur groups so that the substance, in this case acetaminophen, can be easily excreted in urine.
If the amount of acetaminophen exceeds the capacity of the liver for sulfation, it then utilizes the UGT genes for glucuronidation reactions, which also makes the acetaminophen more water-soluble and able to be excreted. [ref]
CYP2E1 and oxidative pathway:
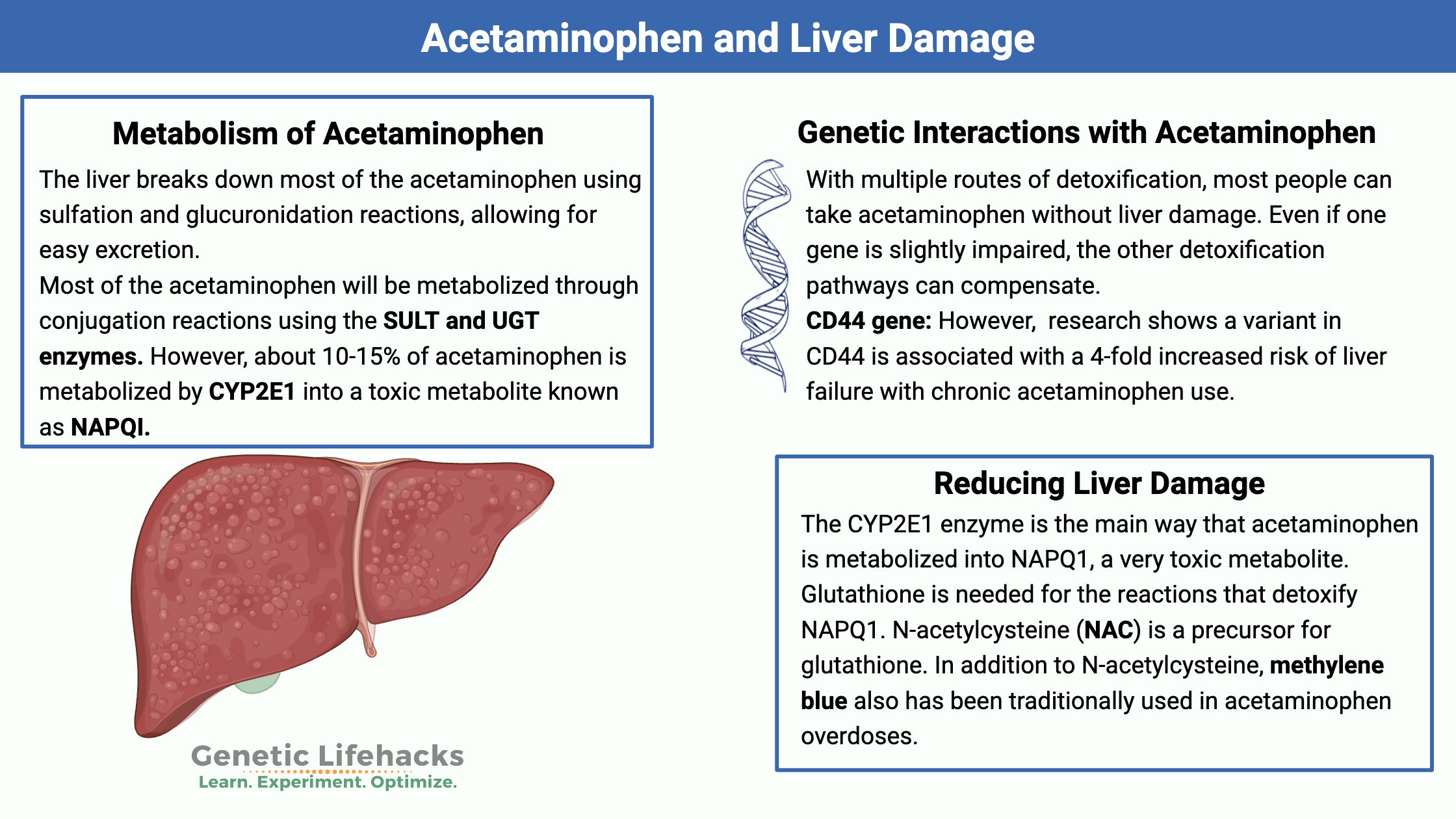
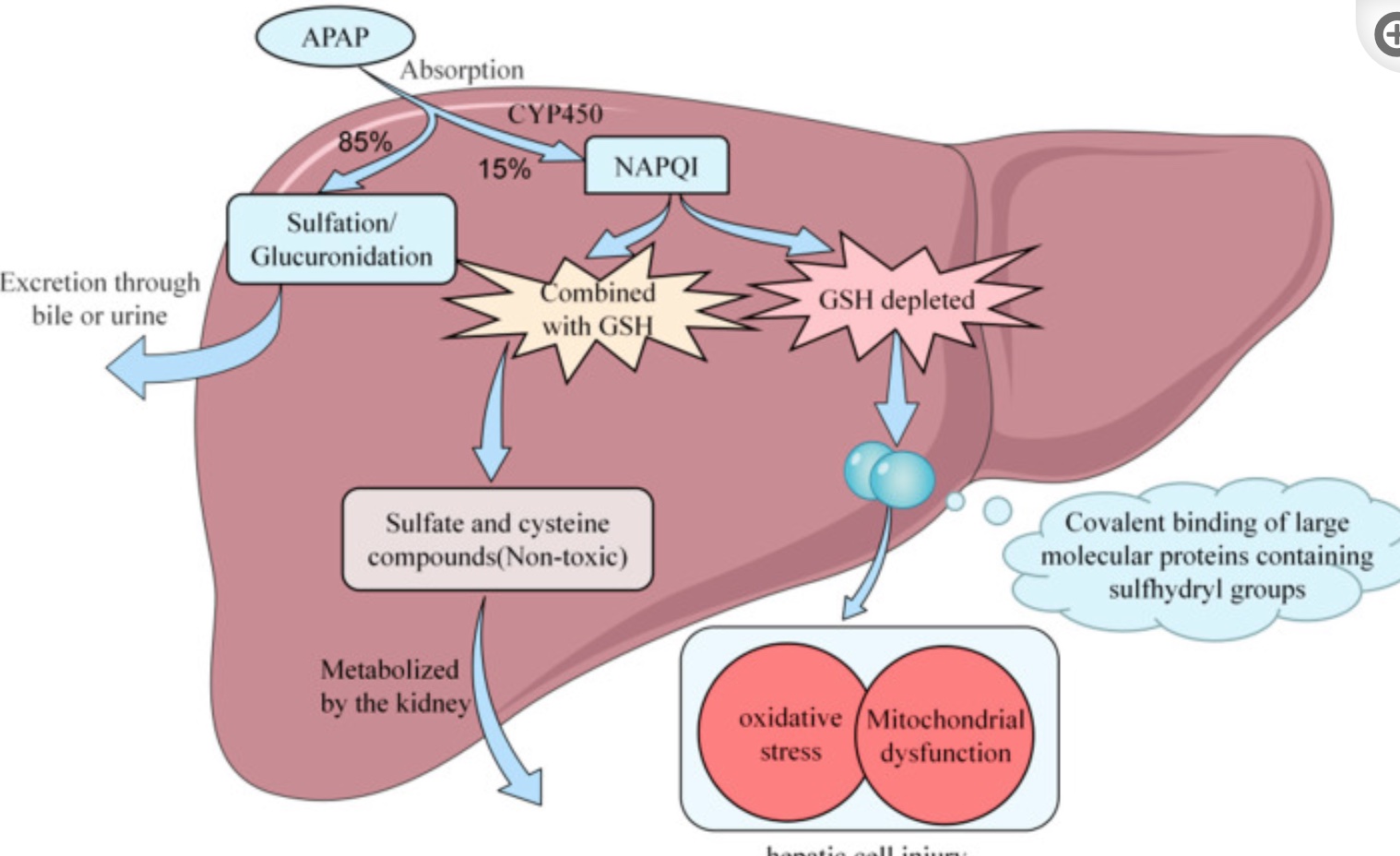
The liver breaks down most of the acetaminophen using sulfation and glucuronidation reactions, allowing for easy excretion. However, about 10-15% of acetaminophen is metabolized by CYP2E1 into a toxic metabolite known as NAPQI (N-acetyl-p-benzoquinone imine).[ref]
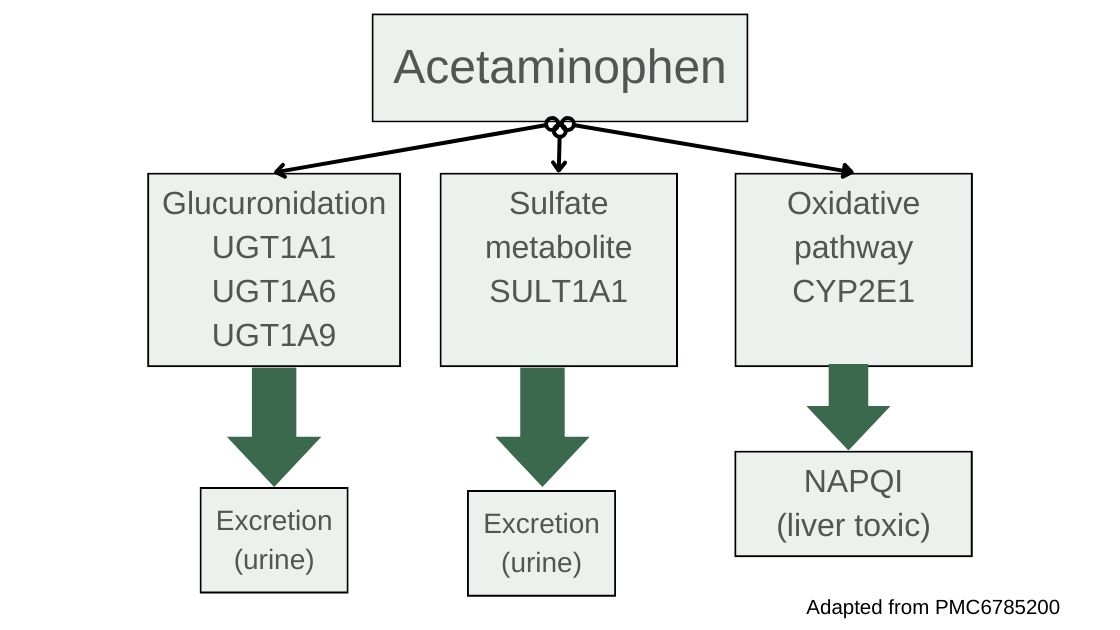
Detoxification with glutathione:
NAPQI then needs to be neutralized with glutathione, which is catalyzed using the GST genes. With sufficient glutathione present, NAPQI is very quickly metabolized into sulfate and cysteine compounds, which are readily excreted through the kidneys.[ref] However, when it isn’t neutralized, NAPQI is highly reactive and can cause oxidative stress and damage to the liver cells, hepatocytes, leading to cell death.
What goes wrong in acetaminophen-induced liver damage?
When NAPQI levels are higher than the liver’s capacity to neutralize, NAPQI will form protein adducts on the mitochondria of liver cells. This causes high oxidative stress, mitochondrial dysfunction, and cell death of the hepatocytes.[ref] As these cells die, inflammatory cascades perpetuate the oxidative stress, leading to bleeding, fibrosis, or possibly liver failure.
Importantly, people who already have liver disease are at a higher risk of liver damage from acetaminophen because they likely aren’t producing enough glutathione. If you have pre-existing liver damage, talk with your doctor about whether acetaminophen is safe for you.
There are a couple of other scenarios in which acetaminophen is more likely to cause liver damage:
Alcohol Use Disorder:
Normally, alcohol is metabolized using the alcohol dehydrogenase enzymes, but in cases of chronic overconsumption or binge drinking, the CYP2E1 enzyme is upregulated to metabolize the extra alcohol. People who drink a lot on a regular basis are more likely to have the CYP2E1 enzyme constantly upregulated, potentially increasing the conversion of acetaminophen into the toxic metabolite, NAPQI. This increases the risk of liver damage when using acetaminophen along with chronic alcohol consumption — adding to the damage to the liver from alcohol.[ref]
Glutathione System Overwhelmed:
Under normal circumstances, NAPQI is quickly neutralized by conjugation with glutathione, a powerful antioxidant found in liver cells, and then excreted from the body. However, when excessive amounts of acetaminophen are ingested, the liver’s supply of glutathione can be depleted rapidly, leaving NAPQI unneutralized.[ref]
Glutathione is the master antioxidant, but there are several situations in which glutathione levels may already be low and thus unable to rise to the occasion for high doses of acetaminophen. People with chronic diseases, such as cancer or liver disease, are likely to have low glutathione levels. Additionally, glutathione levels naturally decrease with age, partly due to a decline in the rate of synthesis. Additionally, some medications reduce glutathione levels by being substrates for conjugation. The irony here is that you’re more likely to reach for acetaminophen for pain when you have a chronic condition that is draining your glutathione reserve.
Related article: Glutathione, genetics, and detoxification
In infants and in utero:
In young babies, the sulfation and glucuronidation pathways are not fully formed, and the metabolism of acetaminophen is shifted in utero and in preterm babies, potentially increasing the risk of problems.[ref][ref]
Acetaminophen, estrogen, and pregnancy:
Estradiol (E2) is the primary form of estrogen in the reproductive years, and one way that estradiol is metabolized is through sulfation. Acetaminophen affects the sulfation pathway for estradiol.
A study found that acetaminophen use causes decreased sulfation of sex hormones. “The effect of taking acetaminophen on sulfated sex hormones was roughly equivalent to the effect of 35 years of aging.” [ref]
This brings up a lot of concerns about acetaminophen and estrogen: its impact on pregnancy and implications for the fetus.
For example, a 2020 study showed that higher levels of acetaminophen in umbilical cord blood correlated with a two-fold increase in ADHD and a three-fold increase in the risk of autism spectrum disorder.[ref] Another study showed that acetaminophen alters gene expression in the placenta, reducing aromatase (CYP19A1) and increasing HSD17B1, along with increasing estradiol. Estradiol levels play an important role in the developing fetus, affecting brain and reproductive organ development.[ref]
If you’re pregnant, be sure to talk with your doctor about the risk of acetaminophen use.
Acetaminophen and autism spectrum disorder (ASD), ADHD, and asthma:
There have been questions around the use of acetaminophen during pregnancy for a couple of decades. In 2015, the FDA addressed the concerns with a Safety Communication stating that it is safe and that the studies showing that it wasn’t safe were all flawed.[ref]
Let’s take a look at some of the studies and then dig into the mechanism of action.
- A large study in 2024 found that 7.5% of children were exposed to acetaminophen during pregnancy, and the rate of autism was higher in those children compared to children whose mothers hadn’t taken acetaminophen while pregnant. However, when the researchers adjusted for other things, including siblings with autism, the increased risk was no longer statistically significant.[ref][ref] (Note that other researchers point out bias in that paper.[ref])
- Another large study published in 2021 involving 73,000 children and mothers found that there was a 19% increase in relative risk of ASD with prenatal acetaminophen exposure.[ref]
- A 2025 meta-analysis of studies on acetaminophen use during pregnancy and infancy shows that the majority of studies and the higher-quality studies show a positive association between acetaminophen use and ADHD, ASD, or neurodevelopmental disorders.[ref]
A couple of things to consider here.
- First, it is known that under-reporting of acetaminophen usage is a big problem in these studies. Asking someone a few years later to remember whether they took acetaminophen during pregnancy is just not all that accurate.[ref]
- The second question is whether the cause of autism is related to whatever caused the mother to take a pain reliever, versus whether it is due to the type of pain reliever.
Another extensive research paper looked at whether the timing of acetaminophen exposure was relevant. The conclusion was that, based on animal studies and epidemiological studies, acetaminophen exposure during infancy was a greater risk factor than in utero exposure for ASD. [ref – open access]
Why could the risk be greater during infancy? Again, studies in infants and in animals show that an inability to detoxify the metabolites of acetaminophen is due to lower levels of glutathione and sulfation. Animal studies show that the metabolites can be toxic to neurons at levels that are much lower than those required for liver damage.[ref][ref] I can’t help but think that the times when you give an infant acetaminophen – circumcision, shots, and illnesses – are also the times when the antioxidant system is already taxed, bringing about two hits to their young detox system.
The risk of asthma is higher in children exposed to acetaminophen during pregnancy, and that risk is exacerbated by maternal genetic variants related to acetaminophen detoxification.[ref]
Genetic interactions with acetaminophen:
With multiple routes of detoxification, most people can take acetaminophen without liver damage. Even if one gene is slightly impaired, the other detoxification pathways can compensate. However, a small percentage of the population may still encounter problems from chronic acetaminophen usage or high doses.
Genetic studies on the topic are actually pretty extensive, and several genetic variants have been identified that increase the risk of liver damage from chronic or high acetaminophen usage.
For example, more than a decade ago, researchers found that the CD44 gene was likely involved in the risk of liver damage from high doses of acetaminophen. For the chronic dosing studies, most studies are looking at doses of 4 g/day.[ref] (This used to be the maximum recommended acetaminophen dose per day, but that has now changed to 3g/day.) For reference, a single over-the-counter Extra Strength Tylenol is 500 mg, with the directions saying not to exceed 6 tablets in 24 hours (so 3g/day). Prescription doses can be up to 4g/day.[ref]
With the research pointing to CD44 and increased liver damage markers, researchers used mouse models and human genetics to understand which SNP (single nucleotide polymorphism) causes the increased risk.[ref][ref]
What is CD44? The CD44 gene encodes a cell-surface receptor involved in various processes, including cellular differentiation, cell-to-cell adhesion, recruitment of immune system cells, and as a receptor for hyaluronic acid. Studies in humans and animals with non-alcoholic fatty liver disease show that CD44 plays a key role in the inflammation and liver damage in NAFLD.[ref]
Other genetic studies have looked at genes in pathways known to be involved in acetaminophen metabolism, including genes related to sulfation, glucuronidation, and glutathione production.
For example, a study that looked at genetic differences in a group of 192 individuals who took 4 g/day of acetaminophen found that variants that decreased sulfation (specifically in the SULT1E1 gene) were more likely to have elevated liver enzymes. The study showed a huge variation in liver enzyme levels (image below), but it didn’t identify any specific SNP. It just showed that SULT1E1 was likely involved and that combinations of SULT variants plus GST variants were likely deleterious.[ref]
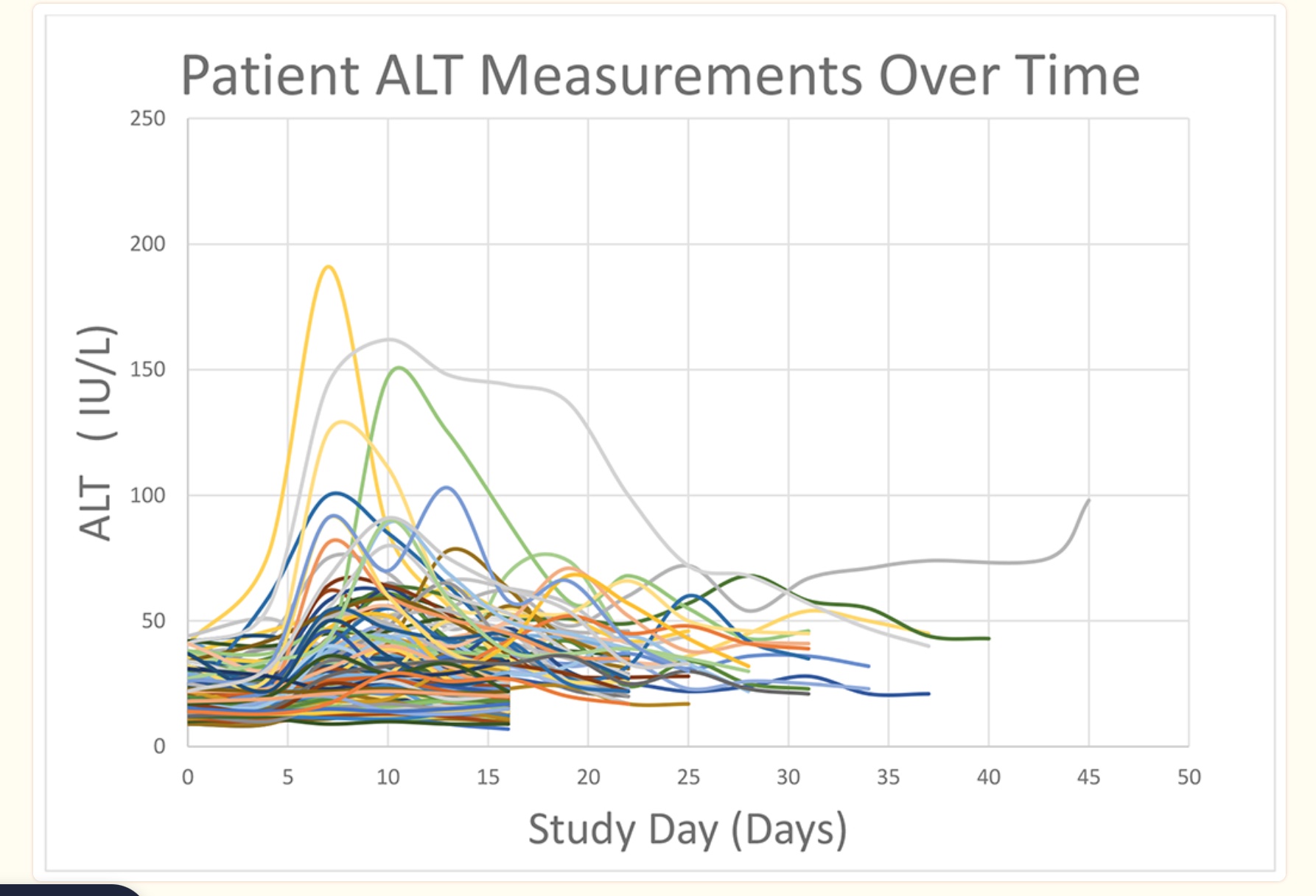
Another cell line genome-wide study found more than 22 genes related to susceptibility to acetaminophen-induced liver damage. The combination of variants linked to a slightly increased risk of liver damage could add together to increase the risk more significantly. [ref]
In summary, knowing your risk factors may help you figure out whether acetaminophen is a safe choice for you as a pain reliever when using it at higher doses or for longer periods of time. The genotypes section below includes genetic variants associated with liver problems from acetaminophen, but please keep in mind that more research is needed on this topic to fully understand individual risk.
Again – talk to your doctor if you have medical questions.
Other studies on side effects or risks from acetaminophen:
Ototoxicity: Regular use of acetaminophen increases the relative risk of hearing loss by 22%. [ref] Research shows that regular acetaminophen use decreases autophagic degradation and causes lysosomal dysfunction leading to hearing loss. In mice, the ototoxicity could be mitigated or reversed with NAC.[ref]
Gastric bleeding: Similar to NSAIDs, acetaminophen can also increase the risk of gastrointestinal bleeding or ulcers. One study in older adults found a 25% increased relative risk of bleeding ulcers in individuals who had been prescribed acetaminophen twice in six months in the UK.[ref]
Heart problems: Acetaminophen increases ROS in the heart and other organs, and at higher concentrations can cause mitochondrial dysfunction in the cells of the heart muscle.[ref] In older adults in the UK, regular acetominophen use increases the relative risk of heart failure or hypertension by a little bit.[ref][ref]
Hematological malignancies: High use of acetaminophen (> 4 days/week for 4+ years) increases the ris myeloid neoplasms, non-Hodgkin’s lymphomas, and plasma cell disorders. The study on this also looked at other NSAIDs, including aspirin and ibuprofen, and found that they did not increase the risk of blood cancers.[ref]
Genotype report: Acetaminophen and liver damage
The genotypes section of the article includes genetic variants associated with liver problems from acetaminophen, but if you have any concerns about your acetaminophen use, talk with your healthcare provider.
Access this content:
An active subscription is required to access this content.
Related articles and topics:
References:
Debbie Moon is a biologist, engineer, author, and the founder of Genetic Lifehacks where she has helped thousands of members understand how to apply genetics to their diet, lifestyle, and health decisions. With more than 10 years of experience translating complex genetic research into practical health strategies, Debbie holds a BS in engineering from Colorado School of Mines and an MSc in biological sciences from Clemson University. She combines an engineering mindset with a biological systems approach to explain how genetic differences impact your optimal health.