Key takeaways:
~ The COMT enzyme is a key factor in the metabolism of neurotransmitters, including those involved in pain sensation.
~ Blocking the COMT enzyme causes chronic pain by sensitizing certain pain receptors and increasing inflammatory cytokines.
~ Polymorphisms in the COMT gene affect how the enzyme works and how sensitive people are to perceiving pain.
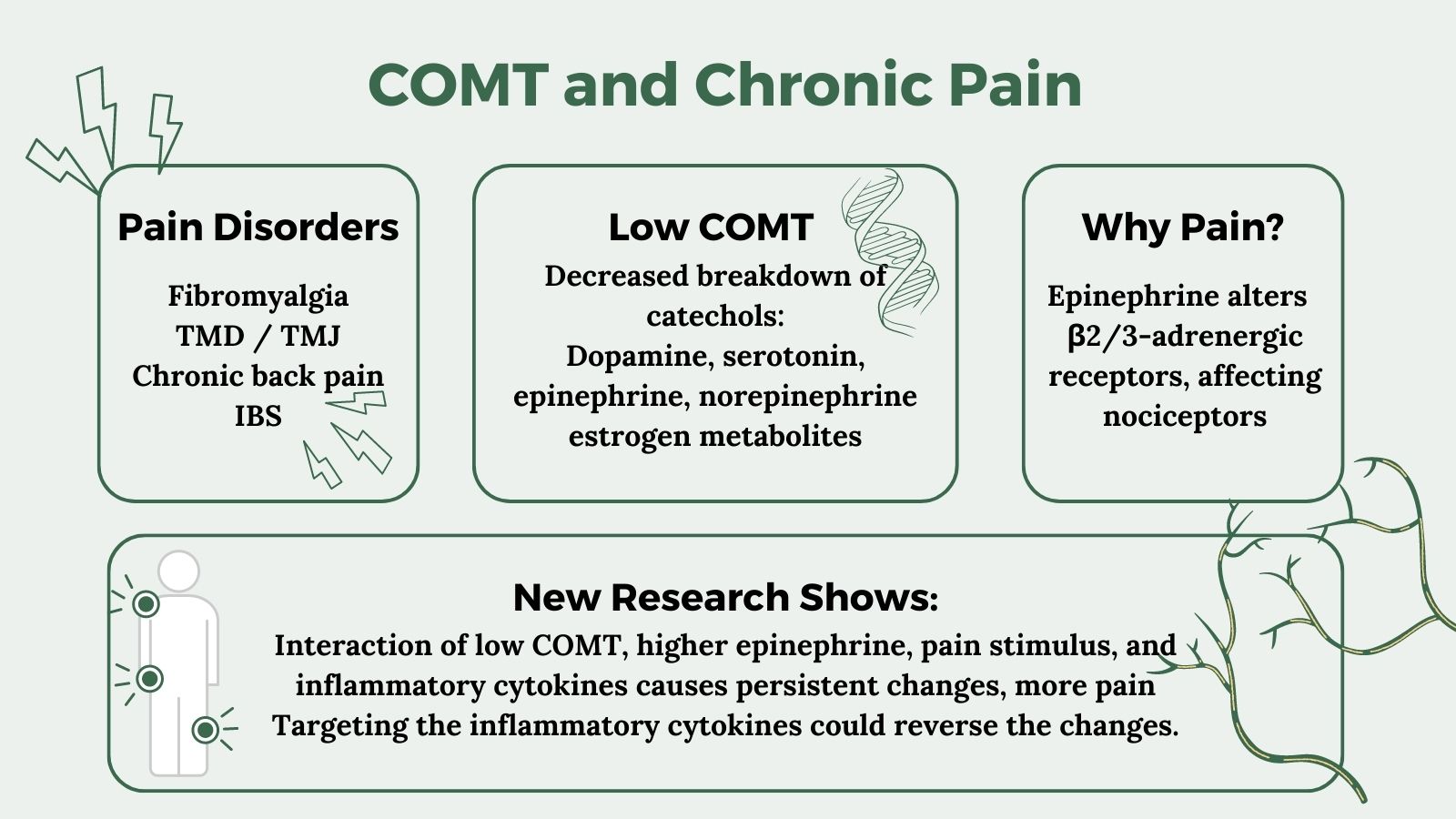
~ COMT SNPs affect an individual’s pain levels in chronic pain disorders such as fibromyalgia, TMJ, back pain, and IBS.
<b>Members</b> will see their genotype report below and the solutions in the Lifehacks section. <a href=”https://www.geneticlifehacks.com/membership/”>Consider joining today</a>.
COMT gene and feeling pain:
The COMT gene encodes an enzyme called catechol-O-methyltransferase, which breaks down catechols. Catechols are a class of molecules that includes neurotransmitters such as dopamine, epinephrine, and norepinephrine.
Other catechols include estrogen metabolites, certain drugs, and natural substances with a catechol structure.
Neurotransmitters are the molecules that nerve cells use to send signals – including telling the brain that you are experiencing pain. Genetic polymorphisms in the COMT gene can affect how much of the enzyme is produced, and thus how likely someone is to experience pain.[ref]
A well-studied variant in the COMT gene is known as Val158Met. The Met/Met genotype is associated with lower COMT activity, and thus slower breakdown of neurotransmitters. In regards to pain disorders, the decreased COMT enzyme alters the level of neurotransmitter available to activate a specific type of adrenergic receptor in peripheral nerves that send pain signals.
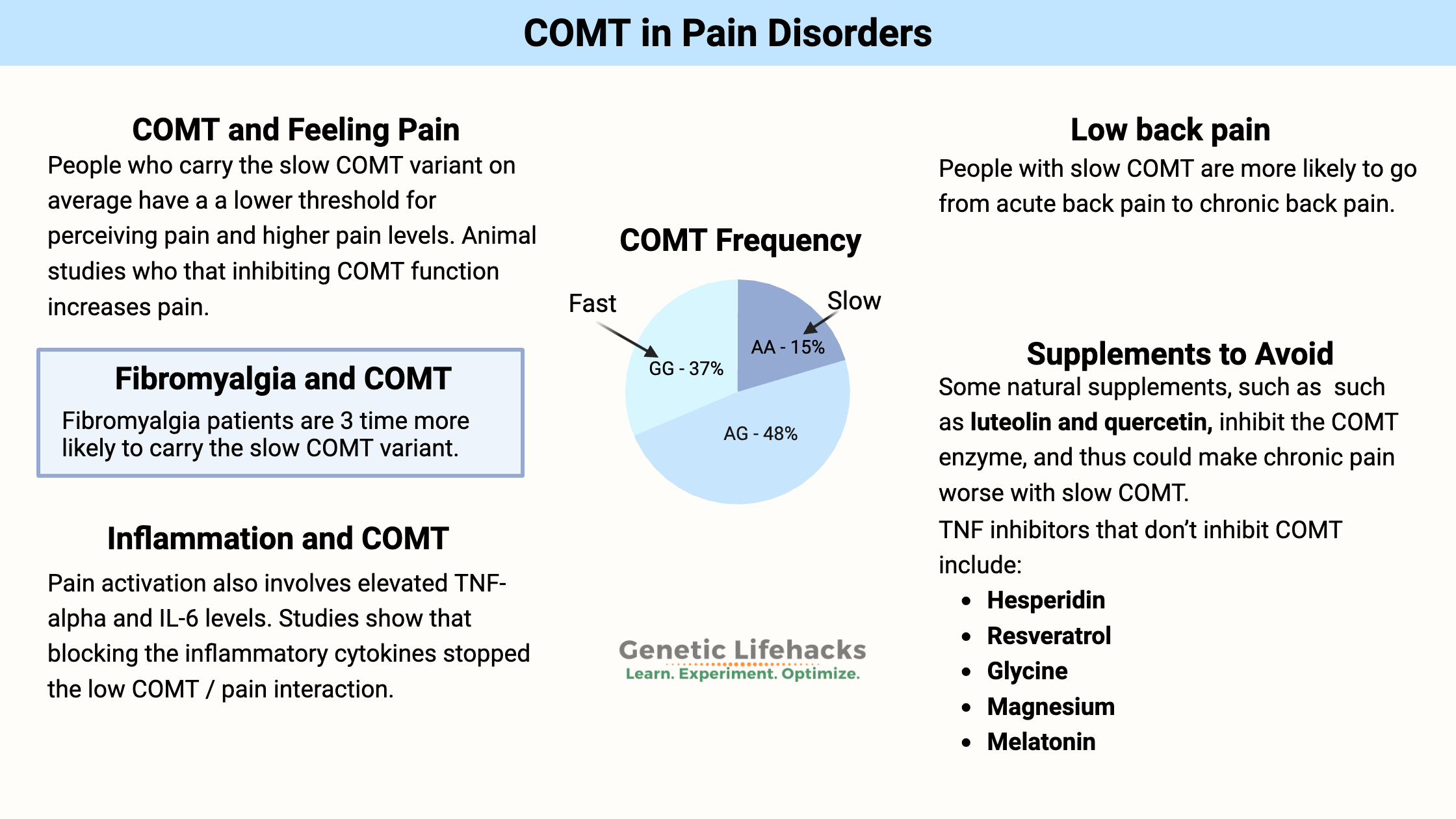
People with the Met/Met genotype are likely to have a lower threshold for perceiving pain and higher pain levels.[ref]
Take back pain, for example:
Many people end up dealing with chronic back pain that isn’t due to injury, and disc degeneration is often blamed. The majority of people with disc degeneration don’t actually feel it, but for some, there is chronic and debilitating back pain.[ref] Just to be clear: COMT isn’t the only gene involved in back pain. There are multiple factors, including other inflammation-related genes.
Related article: Back Pain and Your Genes
Functional Pain Syndromes (FPS):
Chronic pain conditions such as fibromyalgia, temporomandibular disorders, tension headaches, and irritable bowel syndrome are categorized as “functional pain syndromes”. Researchers tie these disorders to being influenced by the COMT genetic variants.[ref]
Let’s take a look at some of the research on how COMT plays a role in pain-related disorders.
Fibromyalgia pain and COMT:
A study involving 112 fibromyalgia patients compared to a matched control group found that they were 3-times more likely to have the slow COMT variant. [ref] Another study found that women with fibromyalgia and the slow COMT variant had more pain than women without the slow variant.[ref]
Is the COMT low-function (slow) variant more common in women with fibromyalgia? It seems that way. A study of over 100 fibromyalgia patients found that they were more likely to carry the slow COMT variant, compared to a healthy control group.[ref]
TMJ, jaw pain, and COMT:
Temporomandibular disorders (TMD) include pain and dysfunction of the temporomandibular joint (TMJ) and jaw pain, especially when chewing.
Pain sensitivity genotyping based on the COMT gene showed that the lower pain sensitivity type cuts the risk of TMJ pain by 2.3-fold.[ref]
Another study looked at the interaction of stress, low COMT activity, and TMD. The study showed that higher stress levels combined with low COMT activity significantly increased the risk of TMD pain.[ref]
Low back pain:
A study of people with low back pain and sciatica found that patients with the slow COMT variant had more back pain and slower recovery.[ref]
One study found that people who tend to go from acute back pain (e.g. threw my back out moving a piano) to chronic lower back pain also were more likely to have higher pain sensitivity throughout the body. This is consistent with other studies that show widespread hypersensitivity to pressure and cold in painful conditions such as TMJ, fibromyalgia, and more. The study also identified COMT and BDNF genetic variants as being important in determining whether acute back pain progresses to chronic lower back pain. [ref]
Not all studies show that COMT causes pain:
Genetic studies don’t always come to the same conclusion. A 2010 study of over 350 people with functional pain disorders found no differences in COMT variants.[ref]
Studies on pain after surgery often do not find that COMT variants make a significant difference.[ref][ref]
Why does low COMT cause more pain with chronic pain syndromes?
There’s a lot of research showing a connection between low COMT genetic variants and pain syndromes. However, the slower breakdown of neurotransmitters doesn’t really explain the ‘why’…
Research into the mechanisms and pathways involved in low COMT and pain shows that the decreased breakdown of epinephrine causes persistent changes in the beta 2 adrenergic receptors which are found on peripheral nerves that sense pain and mechanical stimulation.[ref]
β2 and β3-adrenergic receptors are activated by epinephrine, a catechol neurotransmitter that is broken down by COMT. One place in the body where β2 and β3 -adrenergic receptors are found is in nociceptive pain receptors that react to heat, pressure, cold, or acid. Activation of these receptors can directly cause pain.
A 2007 animal study showed that strong inhibition of COMT with a drug caused increased pain. The researchers found that: “low COMT activity leads to increased pain sensitivity via a β2/3-adrenergic mechanism.”[ref]
This discovery led to further research into how low COMT causes chronic pain via the β2– and β3-adrenergic receptors.
Research shows that pharmacological inhibition of COMT increases the mechanical sensitivity of pain receptors.
In an animal study, blocking COMT with an inhibitor drug for 14 days caused the pain hypersensitivity to persist for at least three weeks after the inhibitor was discontinued.
Two weeks of COMT inhibitor treatment also caused an increase in inflammatory cytokines (TNFα, IL-1β, and IL-6) and activated microglia and astrocytes in the nervous system.
TNF-blocking drugs, such as those used in autoimmune diseases, were able to alleviate the pain. The study concluded: “These results suggest that peripheral β2– and β3ARs drive persistent COMT-dependent functional pain via increased activation of immune cells and production of pro-inflammatory cytokines, which promote neuroinflammation and nociceptor activation. Thus, therapies that resolve neuroinflammation may prove useful in the management of functional pain syndromes.”[ref]
Thus, lower COMT levels combined with inflammation cause persistent pain when specific beta-adrenergic receptors are involved in the sensing of the pain stimulus.
One paper explains that increased adrenergic receptor activation can actually decrease pain in certain situations, but it increases pain in other types of receptors.
- In peripheral pain (muscles, joints) and nociceptive pain, the higher catecholamine neurotransmitter levels increase the pain, especially when inflammation is involved.
- The opposite seems to be true for neuropathic pain (e.g. peripheral neuropathy), where increasing the catecholamine neurotransmitters may help relieve the pain. [ref]
Propranolol response:
Propranolol is a beta-adrenergic receptor antagonist (beta blocker) that is sometimes prescribed for persistent pain.
Researchers have found that propranolol is more effective in reducing facial nerve pain in people with the faster COMT variants than in those with the slow COMT enzyme function.[ref]
For musculoskeletal pain, researchers found that people with intermediate or slow COMT function were more likely to benefit from propranolol for pain relief.[ref]
COMT Genotype Report:
Members: Log in to see your data below.
Not a member? Join here. Membership lets you see your data right in each article and also gives you access to the members’ only information in the Lifehacks sections.
COMT Val158Met:
Check your genetic data for rs4680 Val158Met (23andMe v4, v5; AncestryDNA):
- G/G: Val/Val – fast (higher) COMT activity[ref] higher pain threshold
- A/G: Val/Met – intermediate COMT activity (most common genotype in Caucasians); intermediate pain sensitivity[ref]
- A/A: Met/Met – slow (40% lower COMT activity) [ref] lower pain threshold, higher dopamine; more pain in chronic pain situations[ref][ref] more common in fibromyalgia patients[ref]
Members: Your genotype for rs4680 is —.
Additional variants that may affect pain:
Check your genetic data for rs6267 (23andMe v4, v5; AncestryDNA):
- G/G: typical
- G/T: risk of higher pain sensitivity[ref][ref]
- T/T: risk of higher pain sensitivity[ref][ref]
Members: Your genotype for rs6267 is —.
Lifehacks:
In a nutshell, the catechol-o-methyltransferase – COMT – enzyme transfers a methyl group to a catechol to change the molecule.
A methyl group is simply one carbon plus three hydrogens. It is used in several different cellular reactions to change one molecule into another. For example, serotonin is converted to melatonin in a two-step process, one of which is the addition of a methyl group.
It may seem that a chronic pain condition could be helped by adding more methyl groups through supplements, but this may not be the best plan.
With the low (slow) COMT genetic variant, you may want to be careful and not overload the system with too many methyl groups at one time.
Many people with low COMT function report that supplements such as methylfolate, SAMe, and methylB12, which provide a large dose of methyl donors, can cause mood swings — feeling good shifts to irritability, anger, and anxiety.
The influx of methyl groups can be used by COMT to convert neurotransmitters, estrogens, and other molecules with a catechol structure. Suddenly altering the rate at which neurotransmitters are metabolized may cause mood changes.
Blocking inflammation to stop COMT-driven pain:
Researchers have found that low COMT or drug inhibition of COMT leads to increased pain sensitivity through activation of beta-2 adrenergic receptors.
Recently, a study showed that this pain activation also involves inducing nitric oxide formation and that elevated TNF-alpha and IL-6 are involved. Blocking the inflammatory cytokines stopped the low COMT / pain interaction.
The conclusion of the study: “Additionally, inhibition of NO synthases and neutralization of the innate immunity cytokines TNFα, IL-1β, and IL-6 blocked the development of COMT-dependent pain.”[ref]
Reversing pain takes time:
Another study on pain induced by blocking the COMT enzyme found that the pain persisted for weeks after the COMT enzyme was unblocked. The authors concluded: “This study demonstrates that sustained stimulation of β2– and β3ARs produces functional pain that persists after removal of the causal stimulus…”[ref]
In addition, this research study also found that the persistent pain was due to increased TNFα, IL-1β, and IL-6 and microglial activation, and that blocking TNF-alpha was effective in reducing the pain (in animals).[ref]
Natural TNF inhibitors:
Graphical Overview:
Related articles:
Familial Mediterranean Fever: Mimics fibromyalgia, arthritis, inflammation