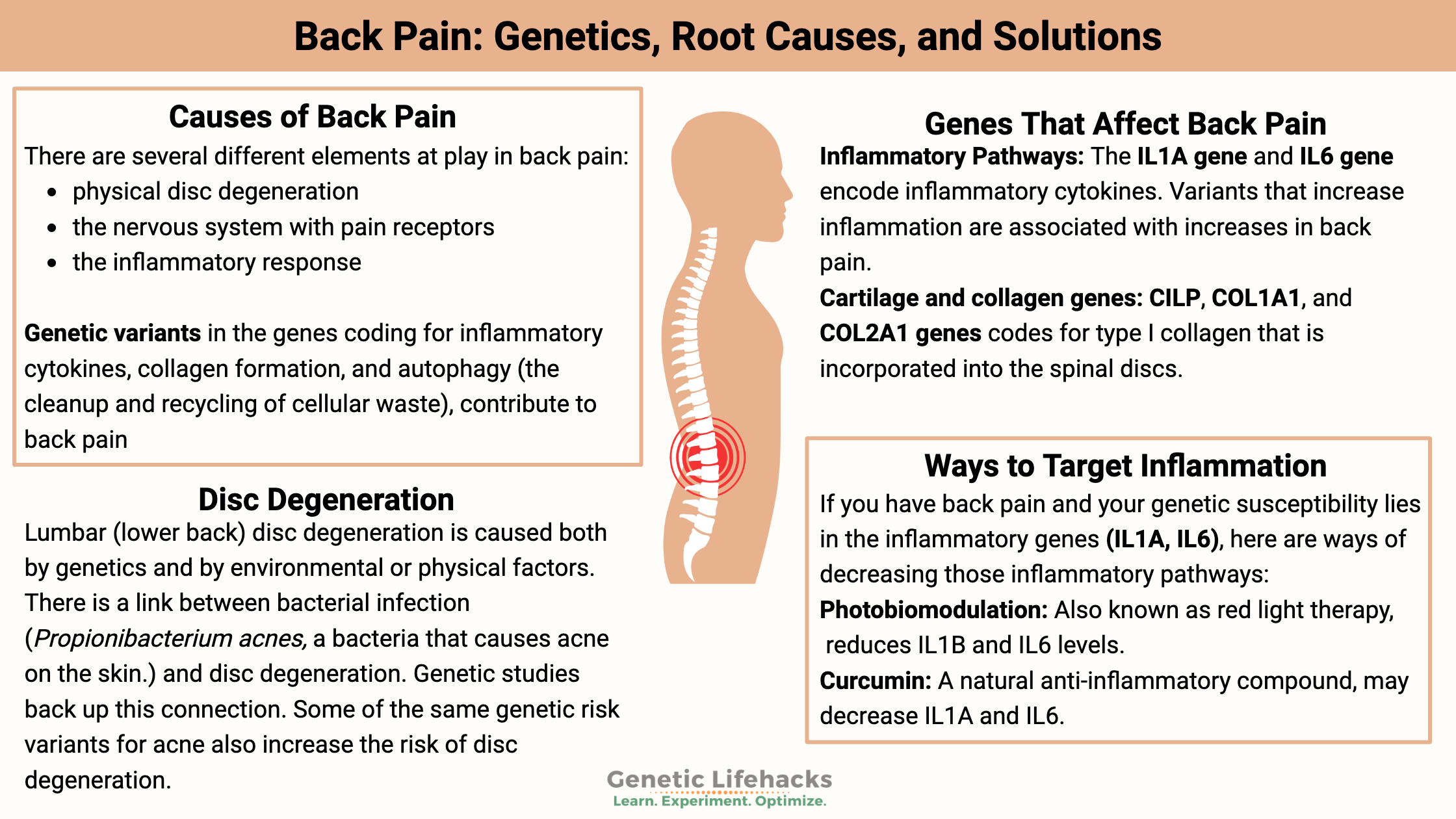
Key takeaways:
~ Back pain isn’t always a mechanical problem or injury. Instead, factors like inflammation, genetic variants, and nerve sensitivity play significant roles.
~ Disc degeneration is common and often painless. Elevated inflammatory cytokines explain why some experience pain while others do not.
~ Genetic variants in inflammatory pathway genes make some people more susceptible to back pain.
~ Sciatica has a strong genetic component, with studies indicating up to 40% heritability.
What causes back pain?
If you are like me, you may have thought back pain was always a mechanical or structural type of problem — something is broken down in the back that hurts. We talk about it as a mechanical problem: “I was moving a piano yesterday, and I threw out my back.” (Or, more realistically, for people that I know: “I was sitting on the couch… reached to grab a blanket and threw out my back.”)
But that isn’t all that there is to the story. It turns out that the majority of people by middle age have disc degeneration. But most don’t have pain from it. Piano movers can move that piano all day long and be perfectly fine; someone else might step off of a curb wrong – and be in pain for months. And yes, your genes are involved.
Mechanics of your back:
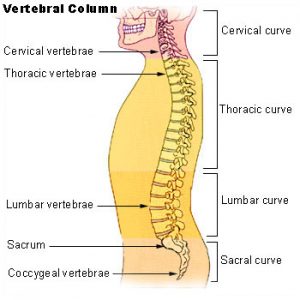
The spinal column is made up of 33 vertebrae, separated by spongy discs.
- The first 7 vertebrae are the cervical spine (your neck).
- The next 12 vertebrae are called the thoracic vertebrae (chest area).
- The lumbar region comes next with 5 vertebrae.
- The final five vertebrae are called the sacral spine (includes the 4 vertebrae that make up your tailbone).
In between the vertebrae are the discs that are made up of connective tissue. The outer part of the disc is called the annulus fibrosus, which is a tough yet flexible material. The inner part of the disc is called the nucleus pulposus, which is more of a gel-like material.
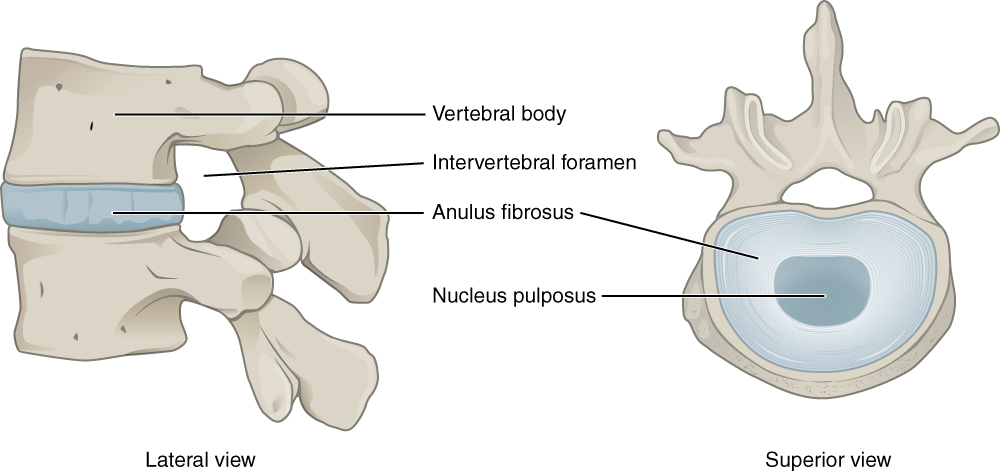
The annulus fibrosus is made up of layers of cartilage that are made from type I and type II collagen. The nucleus pulposus consists of loose fibers suspended in a gel. This acts as a shock absorber for the spine. The composition of the extracellular matrix making up the gel includes a couple of types of collagen and specific glycoproteins.
What causes the pain?
There are several different elements at play in back pain:
- physical disc degeneration
- activation of pain receptors in the nervous system
- the inflammatory response
We are all different in our genetic variants in the genes coding for inflammatory cytokines, collagen formation, and autophagy (the cleanup and recycling of cellular waste).
Back pain can come from a combination of those sources – inflammation, altered collagen in the extracellular matrix, and oversensitive pain receptors. These causes work together. For example, inflammatory cytokines can cause the breakdown of the extracellular matrix of the disc. Excessive autophagy can cause cell death which increases inflammatory cytokines.[ref]
Herniated or slipped disc:
You will often hear people talk about a slipped disc, which brings to mind a terrible picture of a vertebra off to one side.
A herniated or slipped disc refers to when part of the nucleus pulposus protrudes through the annulus fibrosus (see the picture above). The terminology is a bit misleading here because nothing is really ‘slipped’, more of a bulging in one direction.
What causes disc degeneration?
Lumbar (lower back) disc degeneration is caused both by genetics and by environmental or physical factors. It is estimated that genetic factors are more important than environmental factors.
Research shows that multiple things are going on in disc degeneration:[ref]
- degradation of the matrix that makes up the soft, gelatinous center of the disc
- decreased hydration
- inflammation infiltrating the disc
- physical changes to the biomechanics of the spine
- nerve and blood vessel growth in the area
You’ll notice below in the Genotype report section that the back pain susceptibility genes are grouped by whether they relate to inflammation, the collagen matrix, or autophagy (the turnover and recycling of mitochondria and other damaged cell parts).
Pain — or no pain?
A lot of people have disc degeneration – and don’t know it! They have no pain or symptoms.
Researchers looked at the MRIs of individuals without lower back pain compared to MRIs of people with lower back pain — and came up with interesting results! Of the people without lower back pain, 64% had disc degeneration. In the study, half of the people with disc degeneration had bulging discs, and about a quarter had protrusions.[ref]
Inflammation:
Why does disc degeneration cause pain only for some people?
Elevated inflammatory cytokines may be at least part of the answer.
Interestingly, there is a link between bacterial infection and disc degeneration. Researchers had suspected for more than a decade that a portion of diseased discs was due to chronic infection from Propionibacterium acnes. (This is one of the bacteria that causes acne on the skin.)
Quite a few studies have shown that Propionibacterium acnes is present in disc degeneration, but there was always a question of whether the bacteria could have been contaminated from the skin instead of colonizing the disc material. A recent study has put this question to rest. It looked at samples of 162 discs from people undergoing surgery for disc herniation. The samples showed that 44% of the discs had bacteria in them, with most of those having Propionibacterium acnes in them. Furthermore, the samples showed high levels of bacteria and biofilms having formed in the disc material.[ref]
Genetic studies back up this connection to bacterial infection causing inflammation in the disc. Some of the same genetic risk variants for acne also increase the risk of disc degeneration.
The gooey center:
The nucleus pulposus is constantly renewing – breaking down the extracellular matrix and rebuilding it.[ref]
Here’s the image of this again:
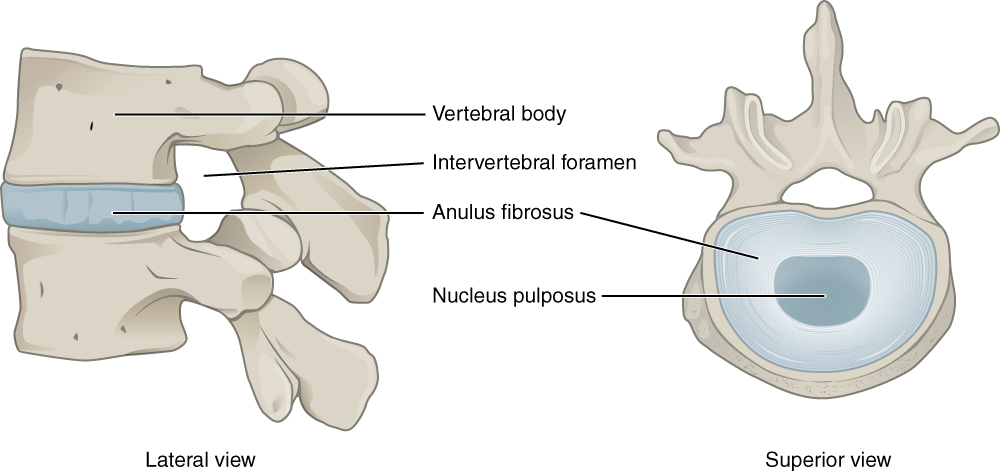
The breakdown process utilizes matrix metallopeptidase (MMP enzyme) and ADAMTS, another protease enzyme. When the process is unbalanced, such as in aging, there will end up being an increased proportion of type I collagen which makes the nucleus pulposus – the gooey center – more fibrous. This results in a decreased capacity for the disc to withstand stressors, loss of disc height, and eventually an influx of inflammatory factors, such as TNF-alpha and IL-1. These inflammatory cytokines then increase the secretion of MMP and ADAMTS, causing a vicious cycle of more breakdown, more fibrosis, and then more inflammation.[ref]
Thus – stopping the initial imbalance of the nucleus pulposus breakdown to rebuilding rate would prevent disc disease. Stopping the increase in inflammation will also prevent it from getting worse.
Mitochondrial dysfunction:
Mitochondrial dysfunction is thought to be one of the initiating factors in initiating the cascade of events that causes disc degeneration. Mitochondria are the ‘powerhouse of the cell’, making ATP for the cell to use for energy. When mitochondria aren’t functioning optimally, they also create an excess of ROS (reactive oxygen species). The environment of the center of the disc is one that is naturally lower in oxygen and higher in water, which results in the cells having less ability to handle too much ROS. The excess ROS ends up damaging the extracellular matrix and activates the inflammatory pathways.[ref]
What about sciatica?
Pain, numbness, and tingling shooting down your hip and leg can be caused by a herniated lumbar disc pressing on the sciatic nerve. However, it isn’t always due to spine problems — other possible causes of sciatica include the piriformis muscle in the butt constricting the nerve. Sciatica can be extremely painful and aggravating. Genetic studies using twins estimate the genetic component of sciatica could be as high as 40%.[ref]
Back Pain Genotype Report
Lifehacks: Natural solutions for back pain
I’m assuming that if you have back pain, you’ve tried various pain relievers (NSAIDs, aspirin) and either a heating pad or ice pack already… Hopefully, you have already looked into stretches and gentle exercise options, as well as consulting with your doctor for medical advice.
Instead, this section will focus on targeted natural therapies with clinical trial data – to go along with specific genetic variants. This is all for informational purposes only; please talk with a doctor if you have questions.
Natural Ways to Target Inflammation in Back Pain:
If you have disc disease and your genetic susceptibility lies in the inflammatory genes (IL1A, IL6), here are ways of decreasing those inflammatory pathways:
Photobiomodulation:
Red light therapy, also known as photobiomodulation or low-level laser light therapy, reduces IL1B and IL6 levels at specific wavelengths. For example, 808 nm in an animal study reduces inflammation and pain in joints.[ref][ref] Note that this is dependent on the wavelength used, with some wavelengths (460 and 660 nm) upregulating IL6.[ref][ref]
Photobiomodulation, or red light therapy, seems like a powerful therapy option, but one that needs to be done correctly.[ref][ref] Read through the reference links, do your own research, and consider getting an expert to help with this.
Related article: Red light and mitochondrial energy
Related Articles and Topics:
TNF-alpha: Inflammation, Chronic Diseases, and Genetic Susceptibility
HLA B27: Genetic Variant That Increases Susceptibility to Autoimmune Diseases