Key Takeaways:
~ An excess of fat in the legs that is lumpy and painful to the touch can be lipedema.
~ Researchers now believe that lipedema affects ~10% of women.
~ Lipedema involves fluid surrounding hypertrophic fat nodules.
~ Genetics plays a role in who gets lipedema, but the research here is very new and not yet complete.
~ There are some natural supplements and physical options that may help.
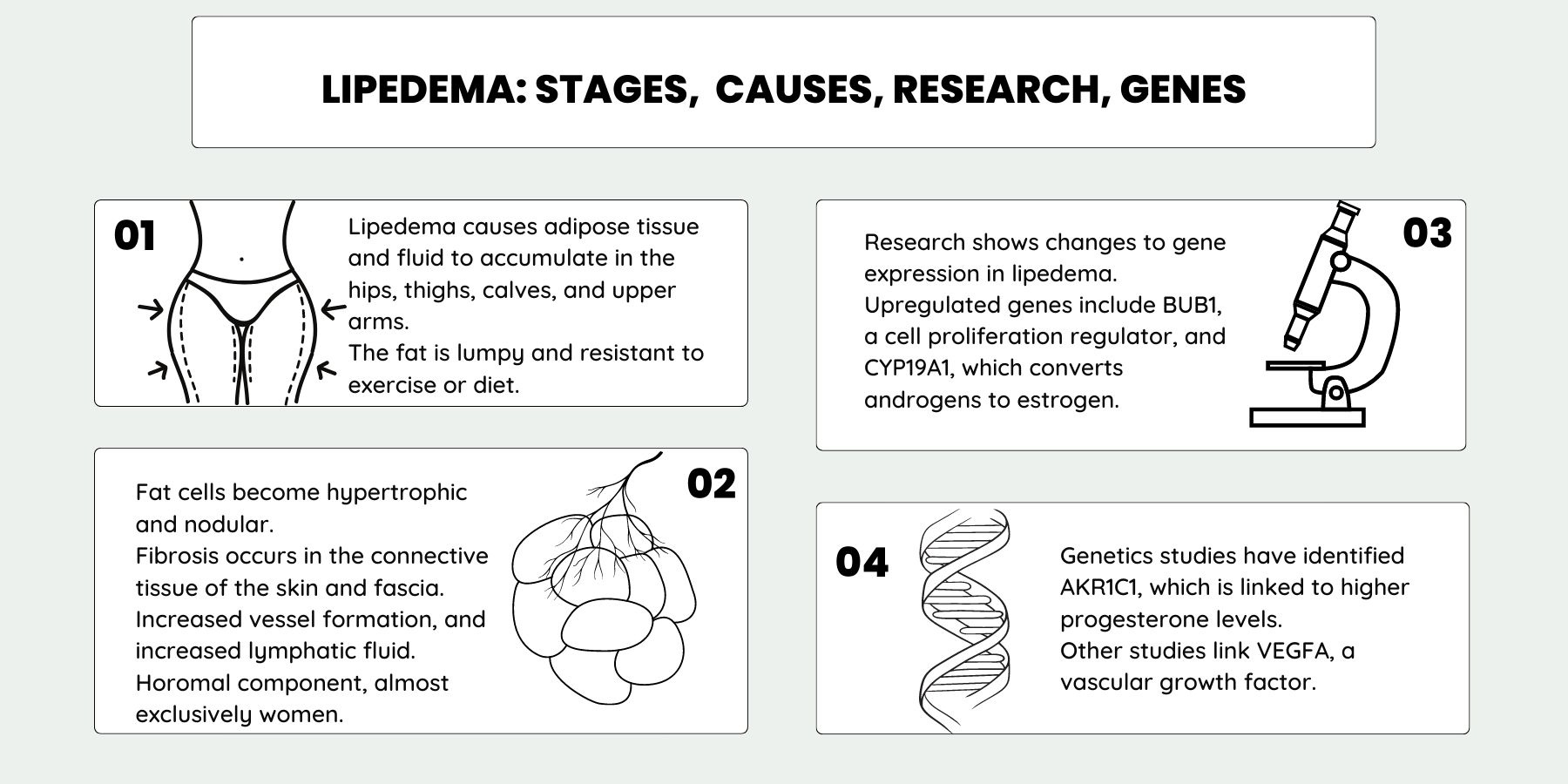
Graphical overview:
What is lipedema?
Lipedema is a disorder of subcutaneous adipose tissue – the fat that lies under the skin. The fat cells become overly large and there is excess fluid around the cells. (Lipedema is also spelled lipoedema.)
People with lipedema have excess subcutaneous fat that feels nodular – like a beanbag with small lumps under the skin. The fat most commonly accumulates in the hips, thighs, and calves, giving someone a pear-shaped body. In some people, it can also accumulate in the back of the arms and under the skin of the lower abdomen.
In general, lipedema is thought to involve excessive expansion of adipose cells, changes in the blood and lymph vessels, and dysfunction of the lymphatic system that drains fluid from the fat tissue.
How can you tell if it is lipedema or normal excess fat?
The lipedema areas may be tender to the touch and easy to bruise. The areas may also feel cool to the touch. In more severe cases, the pain and tenderness may make it difficult to move your limbs. In essence, it becomes uncomfortable to move.
The fat that accumulates in lipedema doesn’t go away with diet, exercise, or even bariatric surgery.[ref]
Importantly, pure lipedema can cause high BMI due to the excess fat and fluid in the legs and arms, but it doesn’t cause the metabolic dysfunction that is common in obesity.[ref] In fact, diabetes is found at much lower levels in people with with lipedema than in people with similar BMIs without lipedema.[ref]
To differentiate between lymphedema, excess fluid in the tissue, and lipedema, clinicians look for the Stemmer sign. In lymphedema, the skin fold between the second and third toes is thickened and cannot be lifted (called the Stemmer sign). In lipedema, the Stemmer sign is negative.[ref]
How common is lipedema?
Researchers now estimate that 8-10% of women are affected by lipedema, but older studies estimated it to be present in 1 in 10,000 women. To put this in perspective, under the current diagnostic standards, millions of women in the U.S. have lipedema.[ref]
Lipedema is found almost exclusively in women, although there are a few rare case studies of it being found in men. It often begins at a time of hormonal change, such as after puberty, birth control pills, pregnancy, or menopause.[ref]
What are the stages of lipedema?
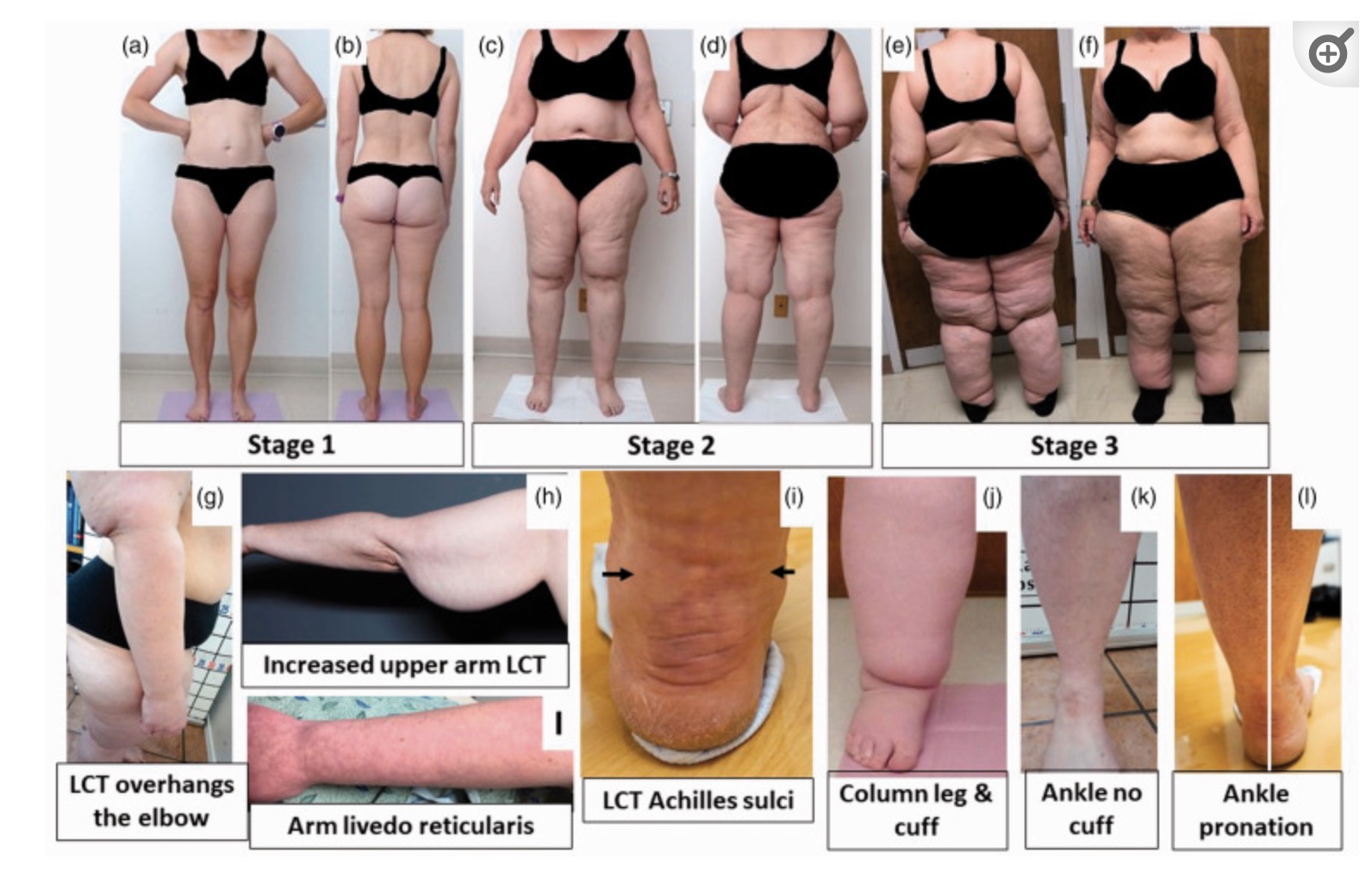
Lipedema is classified into three stages (or sometimes four, depending on the study). A standard of care review for lipedema in the U.S. includes the following three stages of lipedema:[ref]
Stage one skin has a smooth texture, but it may feel pebble-like due to fibrosis in the connective tissue.
Stage two involves more lipedema tissue and skin dimpling. There is excess tissue and progressive fibrosis. The subcutaneous fat has lumps that are easily palpable and larger than in stage one. Stage two lipedema in the arms involves drooping tissue.
Stage three lipedema involves more lipedema tissue with large and numerous nodules. Legs can look like “columns” and a “tissue cuff” can form at the ankles.
Additionally, lipedema is typed by the areas it affects, such as the buttock, thigh, entire lower limbs, arm, or primarily lower legs.[ref]
What is the underlying cause of lipedema?
This is where the research is less clear. While advanced stages of lipedema have been recognized as a condition separate from obesity since the 1950s, much of the research on the cellular changes that occur in lipedema has only been done in the last five years.
Connective tissue: In women with lipedema without non-lipedema obesity, there is an excess of loose connective tissue that is fibrotic, meaning that thick fibers connect the skin to the fascia. Lipedema is also anecdotally associated with hypermobility disorders.[ref]
Immune system: There is also an excess of macrophages in the adipose tissue in lipedema.[ref] Macrophages are a type of white blood cell that can be polarized into either M1 or M2 macrophages. In lipedema, as opposed to obesity, the macrophages are the M2 type.[ref] Mast cells and T cells are not increased in lipedema.[ref]
Increased vessel formation: Additionally, there is increased angiogenesis, or an increase in small blood vessels, promoted by inflammatory signals.[ref]
Thyroid: Hypothyroidism affects about one-third of women with lipedema.
Migraines: Migraines are common in about a quarter of women with lipedema. Interestingly, the frequency of migraines is often reduced in women after they have liposuction for lipedema.[ref]
Hereditary: Genetic factors are thought to play a strong role in who develops lipedema as it runs in families with at least 60% of patients with an affected first-degree relative.[ref]
Estrogen and/or progesterone: A hormonal component is likely because lipedema often begins in women at times of hormonal change such as puberty or after childbirth.
Vascular: Changes in the microvascular system of the lymphatic and capillary systems are also seen, which could lead to hypoxia, or lack of oxygen, to the tissue. In addition, there is hyperpermeability in the vessels, which leads to increased fluid in the tissue.[ref][ref]
Sodium and fat to water ratio: Tissue sodium content is altered in the skin and muscle of the calf in women with lipedema. Additionally, the fat-to-water ratio in the calf is significantly higher than in healthy controls.[ref]
All of this points to a distinct profile of changes that occur in lipedema. But what is the driving factor?
Genetic and proteomic studies point to what is happening at the tissue level
Aldo-keto reductase 1C1:
One of the first genes identified as likely being involved in lipedema is AKR1C1, which encodes aldo-keto reductase family 1 member C1. This enzyme is part of the aldo-keto reductase superfamily, which converts aldehydes and ketones to alcohols using NADH / NADPH. This particular enzyme catalyzes the reduction of progesterone to the inactive form. The researchers who discovered the link between ald0-keto reductase 1C1 and lipedema think that the decreased and less efficient reduction of progesterone to hydroxyprogesterone in adipose tissue is responsible. “Specifically, AKR1C1 can catalyze the reduction of progesterone to 20α-hydroxyprogesterone and allopregnanolone to 5α-pregnane-3α-20α diol by its 20α-HSD activity. In this way, AKR1C1 decreases the levels of progesterone and allopregnanolone in peripheral adipose tissue”. The impaired AKR1C1 could increase progesterone in peripheral adipose tissue, which promotes subcutaneous fat.[ref]
Gene expression changes:
A transcriptional profiling study found that there were over 900 differences noted in lipid composition and 600 different metabolite levels in the adipose tissue of women with lipedema. The researchers found that one of the upregulated genes was BUB1, a cell-cycle regulator that is involved in cell proliferation (and often studied in cancer). The upregulation of BUB1 then enhanced the activation of a number of cell proliferation genes. Importantly, inhibitors of BUB1 stopped the hyper-proliferation of the adipose tissue stem cells. [ref]
Another gene expression study looked specifically at the endothelial cells that line the blood and lymph vessels. This study found that there were altered gene expression factors in estrogen metabolism genes and immune cell infiltration into the lipedema tissue. Specifically, CYP19A1, the enzyme that converts androgens to estrogens was upregulated in the thigh adipose tissue of women with lipedema. In addition, the researchers found that there were no differences in the levels of genes that are normally associated with obesity, such as leptin or adiponectin.[ref]
Genetic studies on lipedema:
A genetics study in 2022 identified possible rare mutations involved in lipedema. The study identified mutations in genes related to adipose tissue differentiation, obesity, and lipids.[ref]
Recently, a genome-wide association study was published that identified several more common variants that may increase susceptibility to lipedema. The study linked variants in the VEGFA gene, which encodes a vascular endothelial growth factor that promotes angiogenesis, to lipedema, as well as genes previously associated with waist-to-hip ratio.[ref]
Another genome-wide association study estimated the SNP-based heritability of lipedema to be 50-60%, demonstrating a strong genetic component combined with environmental or lifestyle factors. The study also found the strongest genetic signal in a gene that is in a member of the HMGIC gene family, which is associated with high levels of polyunsaturated fat in chickens’ thighs, as well as with lipomas in humans.[ref]
More questions than answers:
Reading through the research on lipedema left me with more questions than answers…
Is an increase in the percentage of women with lipedema part of the cause of the increase in obesity rates? The rate of obesity has skyrocketed since 1980, with many different correlations being drawn. Some point to omega-6 vegetable oils or glyphosate, while others blame endocrine disruptors or light at night. The obesity numbers are based simply on BMI and would include people with lipedema.
Given the hormonal aspects of lipedema, is there a link to endocrine-disrupting chemicals such as BPA or phthalates? Something in personal care products or cosmetics?
What causes the increased macrophages in lipedema? And what triggers fibrosis in the adipose tissue?
Genotype report:
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Lifehacks:
There is no quick fix for lipedema, and most websites say that it can’t be cured. However… recent research shows that it can be helped, if not completely cured, by focusing on the lymphatic system and reducing inflammation.
Talk with your doctor about surgery options such as liposuction for lipedema. Keep in mind that liposuction for lipedema is not without risk.[ref]
Talk with your doctor also about what can be covered by your insurance, such as lymphatic massage or compression leggings, if needed. Additionally, you may want to see about getting your thyroid hormones tested due to the overlap with about a third of lipedema patients having hypothyroidism.
Let’s dive into the research on the natural treatment options for lipedema.
Natural Supplements for Lipedema:
Related articles and topics:
Genetics of Double Lashes:
The mutation that causes a double row of eyelashes, as Liz Taylor had, is also linked to lymphatic system problems.
Lymphedema: Causes and Genes
Find out the causes and the solutions for lymphedema.