Key takeaways:
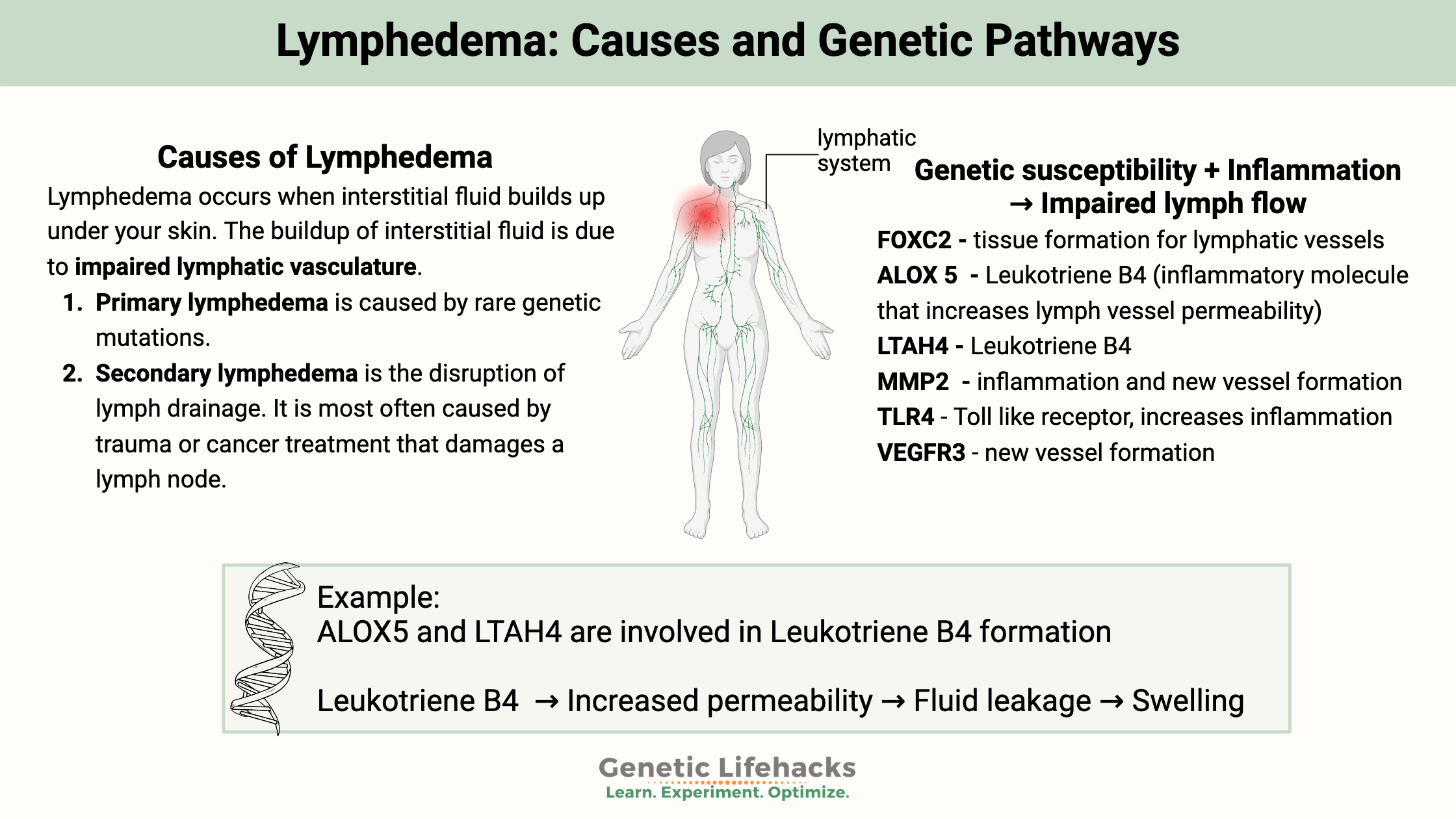
~ Lymphedema is caused by interstitial fluid building up under your skin, often in the legs or arms.
~ Impairments to the lymphatic vessels prevent the fluid from moving out of the tissue.
~ Genetic variants can increase the risk of lymphedema, pointing you toward the underlying cause as well as targeted solutions.
What is lymphedema?
Lymphedema occurs when interstitial fluid builds up under your skin—for example, noticeable swelling in one leg. Lymphedema affects about 3 million people in the US and 200 million worldwide.[ref]
Lymphedema can be mild, with minor swelling and minor discomfort. Or, it can be more severe, causing a lot of swelling and pain.
The buildup of interstitial fluid is due to impaired lymphatic vasculature. Lymph moves through lymph vessels, and lymphedema occurs when the lymphatic system can’t filter and drain fluid out of areas downstream of the disrupted or impaired areas. Over time, this accumulation of fluid can cause swelling, discomfort, and even infections.
Recent research has shed light on the role of genetics in lymphedema. Studies have identified several genetic variants that can increase an individual’s risk of developing this condition. By understanding these genetic factors, you and your healthcare provider may be able to target the most effective solutions tailored for you.
Types of Lymphedema: Hereditary and Secondary
Primary lymphedema is caused by rare genetic mutations. It can start in infancy (Milroy’s disease), in the teen to young adult years (called Meige’s disease), or in middle age or beyond (lymphedema tarda).
Secondary lymphedema is the disruption of lymph drainage. It is most often caused by trauma or cancer treatment that damages a lymph node. Venous insufficiency or kidney disease can also be a cause of secondary lymphedema. In some regions of the world, exposure to a nematode parasite can cause lymphedema. This is the most common type of lymphedema.
Quick note – not all edema (fluid) is lymphedema. There can also be swelling and fluid retention problems with your veins.
What is going on in lymphedema?
Before we get into the details, let’s briefly tour the lymphatic system.
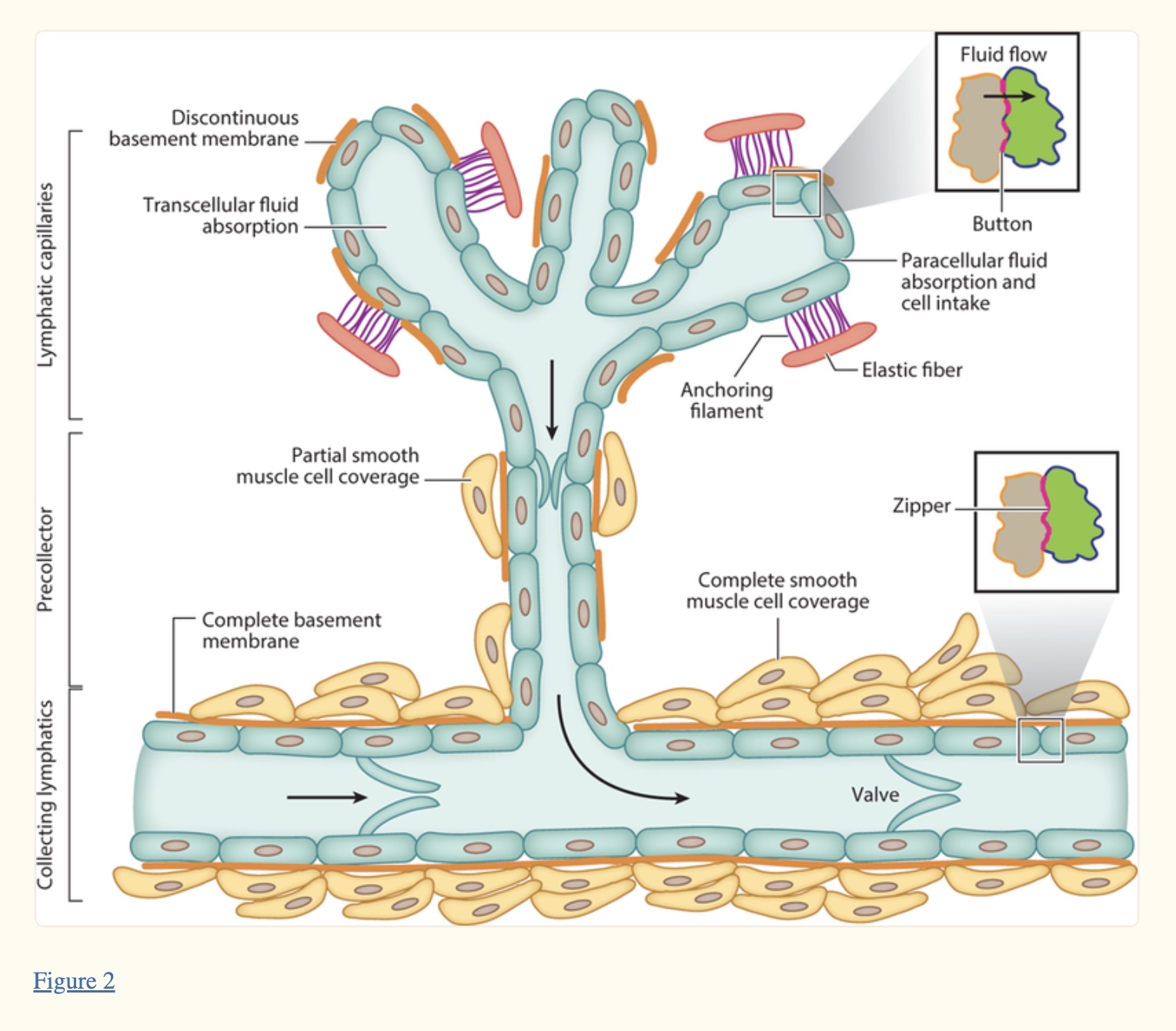
The lymphatic system moves a fluid called lymph throughout the body. Like the circulatory system for blood, the lymphatic system moves fluid from tissues back into central circulation.
Lymph fluid originates in interstitial fluid – the fluid between cells. The lymph fluid is similar to blood plasma. It moves into small lymph capillaries and then into larger vessels and through the lymph nodes.
In the lymph nodes, lymphocytes (a type of white blood cell) filter out any foreign particles — viruses, bacteria, and cancer cells.
Another job the lymphatic system does is to transport fats absorbed in the digestive system.[ref]
Circling back to lymph forming from interstitial fluid… This fluid comes from the circulatory system. At the end of the capillaries that bring in blood from the heart is an area where the lymph fluid is formed. Most of the blood in this area will return to the heart in the venous capillaries, but about 10% of the fluid will enter the lymphatic system.
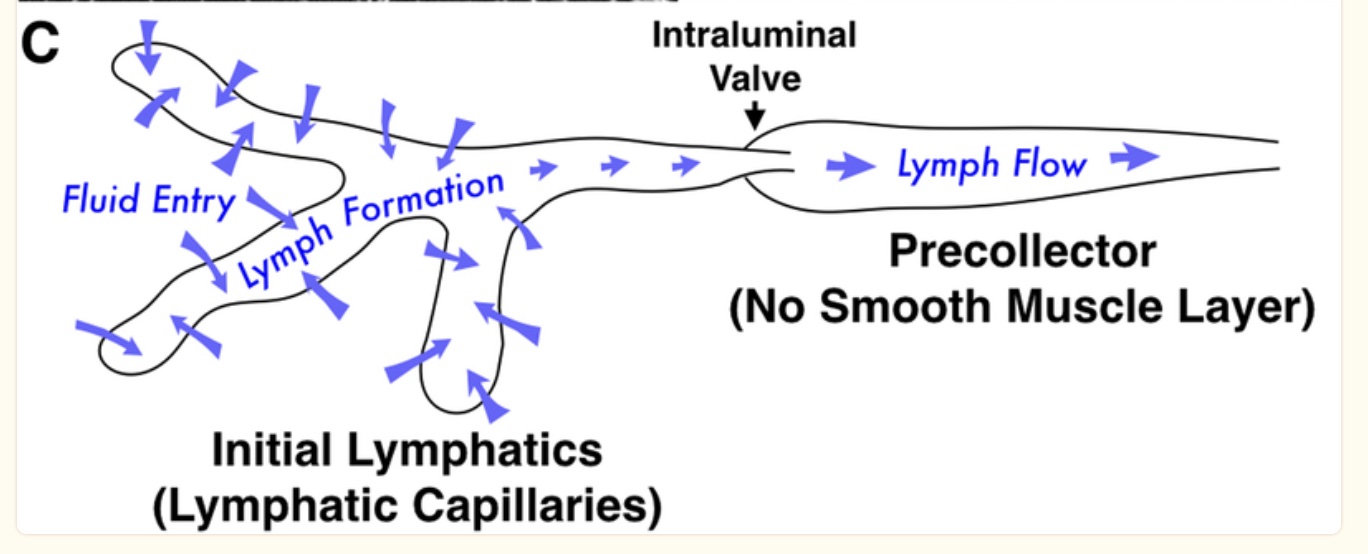
There is no pump for the lymphatic system like the heart pumps blood in the circulatory system. In the lymphatic system, the flow is slow due to peristalsis, various lymph valves, and the movement of adjacent muscles.
If excess pressure develops within the lymph system, fluid can leak back into the interstitial space. This causes the ‘swelling’ seen in lymphedema.
When the fluid accumulates, it can impact cell behavior within that specific tissue. One thing that can happen is that immune cells can be activated in the area, or fibrosis can occur.[ref]
Secondary Lymphedema: Diving Deeper
Secondary lymphedema is the most common type of lymphedema. It is caused by disruption or obstruction in the lymph vessels, resulting in the build-up of interstitial fluid.
For example, arm and chest lymphedema are a common problem for women who have had breast cancer treatment that damages the lymphatic vessels. A recent study on breast cancer survivors with lymphedema found that inflammatory biomarkers were elevated for several months after surgery.
Interestingly, women with lymphedema after cancer treatment were more likely to have had higher baseline (pre-surgery) levels of inflammatory biomarkers such as IL1A and IL6. Additionally, higher pre-surgery VEGF (Vascular Endothelial Growth Factor) levels were also linked to an increased susceptibility to secondary lymphedema.[ref]
Another common cause of lymphedema is the infiltration of the lymphatic vessels by a parasite called Wuchereria bancrofti. This is mainly a problem in tropical developing countries or for people who have traveled to those areas.
So… what initiates the lymphedema?
Leukotrienes: Inflammatory mediators driving lymphedema
Leukotrienes are inflammatory mediators derived from lipids. For example, immune system cells, such as neutrophils, macrophages, and mast cells, can form leukotrienes from arachidonic acid (omega-6 fat).
LTB4 (leukotreine B4) is a leukotriene that is involved in lymphedema. LTB4 is produced in response to inflammatory cytokines, increasing leukocytes’ ability (white blood cells) to cross through the endothelium (cells lining blood vessels and lymph vessels).
Animal studies show that LTB4 plays a central role in secondary lymphedema. Leukotrienes are produced in response to inflammation, thus making tissue inflammation central to the development of lymphedema.[ref]
Leukotriene B4 (LTB4) is an inflammatory lipid mediator synthesized from arachidonic acid using the enzyme 5-LO (ALOX5 gene, below in the genotype section). The final step in the production of LTB4 involves the LTAH4 enzyme (also below).
Once synthesized, LTB4 can increase vascular permeability. This is important during active infection for immune system cells to respond to the site of the inflammation. However, vascular permeability after the infection needs to be halted.
LTB4 binds mainly to the BLT1 receptor. Neutrophils (a type of white blood cell) react by increasing the inflammatory response.
The increased inflammatory response initiated by leukotriene B4 interacts with lymphedema in a couple of ways.
FOXC2 (in the genotype report) is essential for maintaining the integrity of the lymphatic system, especially in the areas around the lymphatic valves that keep lymph flowing in the right direction. FOXC2 also interacts with activated T cells in inflammation.[ref]
Increased fluid accumulation along with the leukotriene B4 molecule activates more of an inflammatory response to the area. It builds on itself. As the lymphedema persists for a longer time, the pro-inflammatory cytokines can cause fibrosis – thickening or scarring – in the area.[ref]
Genetic Polymorphisms and Lymphedema:
Lymphedema due to physically damaged lymph vessels can happen to anyone, especially after surgery or cancer treatment.[ref] However, some people are more susceptible to secondary lymphedema than others. The genetic variants listed below in the genotype report are linked to leukotriene B4 formation, inflammatory cytokines, and lymphatic system development.
Lymphedema Genotype Report:
Lifehacks: 10 Natural Solutions for lymphedema
Talk with your doctor about your options for lymphedema. Common treatments include compression garments and manual lymph drainage.
Research shows that the accumulated fluid in lymphedema exacerbates the problems and causes more immune cells to infiltrate the tissue. Early intervention may be key, so don’t put off talking to your doctor about your options.[ref]
1. Physical therapy plus manual lymphatic drainage therapy:
Clinical trials show that both physical therapy and manual lymphatic drainage are beneficial in reducing lymphedema in cancer patients.[ref]
2. Aquatic Training:
A study found that moderate-intensity aquatic training exercises (water bikes, aqua-jogging, trampoline) for six weeks significantly decreased limb circumference and lymphatic fluid.
Related Articles and Topics:
Hesperidin: An Anti-inflammatory and Immune Boosting Citrus Flavonoid
Ringing in your ears? Genetics, Tinnitus, and Meniere’s disease
References:
Ammon, H. P., et al. “Inhibition of Leukotriene B4 Formation in Rat Peritoneal Neutrophils by an Ethanolic Extract of the Gum Resin Exudate of Boswellia Serrata.” Planta Medica, vol. 57, no. 3, June 1991, pp. 203–07. PubMed, https://doi.org/10.1055/s-2006-960074.
Bertelli, Matteo, et al. “Molecular Pathways Involved in Lymphedema: Hydroxytyrosol as a Candidate Natural Compound for Treating the Effects of Lymph Accumulation.” Journal of Biotechnology, vol. 308, Jan. 2020, pp. 82–86. PubMed, https://doi.org/10.1016/j.jbiotec.2019.11.017.
BONETTI, GABRIELE, et al. “Dietary Supplements in Lymphedema.” Journal of Preventive Medicine and Hygiene, vol. 63, no. 2 Suppl 3, Oct. 2022, pp. E200–05. PubMed Central, https://doi.org/10.15167/2421-4248/jpmh2022.63.2S3.2761.
Breslin, Jerome W., et al. “Lymphatic Vessel Network Structure and Physiology.” Comprehensive Physiology, vol. 9, no. 1, Dec. 2018, pp. 207–99. PubMed Central, https://doi.org/10.1002/cphy.c180015.
Cluzan, R. V., et al. “Treatment of Secondary Lymphedema of the Upper Limb with CYCLO 3 FORT.” Lymphology, vol. 29, no. 1, Mar. 1996, pp. 29–35.
Du, Xinwen, et al. “Strategies in Activating Lymphatic System to Promote Lymph Flow on Lymphedema Symptoms in Breast Cancer Survivors: A Randomized Controlled Trial.” Frontiers in Oncology, vol. 12, 2022, p. 1015387. PubMed, https://doi.org/10.3389/fonc.2022.1015387.
Ezzo, Jeanette, et al. “Manual Lymphatic Drainage for Lymphedema Following Breast Cancer Treatment.” The Cochrane Database of Systematic Reviews, no. 5, May 2015, p. CD003475. PubMed Central, https://doi.org/10.1002/14651858.CD003475.pub2.
Jiang, Xinguo, et al. “Lymphatic Dysfunction, Leukotrienes, and Lymphedema.” Annual Review of Physiology, vol. 80, no. 1, Feb. 2018, pp. 49–70. DOI.org (Crossref), https://doi.org/10.1146/annurev-physiol-022516-034008.
Khan, Nawal, et al. “Effects of Diet-Induced Obesity in the Development of Lymphedema in the Animal Model: A Literature Review.” Obesity Research & Clinical Practice, vol. 16, no. 3, 2022, pp. 197–205. PubMed, https://doi.org/10.1016/j.orcp.2022.05.003.
McLaughlin, Sarah A., et al. “Breast Cancer–Related Lymphedema: Risk Factors, Screening, Management, and the Impact of Locoregional Treatment.” Journal of Clinical Oncology, vol. 38, no. 20, July 2020, pp. 2341–50. PubMed Central, https://doi.org/10.1200/JCO.19.02896.
Mr, Fu, et al. “Model-Based Patterns of Lymphedema Symptomatology: Phenotypic and Biomarker Characterization.” Current Breast Cancer Reports, vol. 13, no. 1, Mar. 2021. pubmed.ncbi.nlm.nih.gov, https://doi.org/10.1007/s12609-020-00397-6.
Nejatian, Nojan, et al. “5-Lipoxygenase (ALOX5): Genetic Susceptibility to Type 2 Diabetes and Vitamin D Effects on Monocytes.” The Journal of Steroid Biochemistry and Molecular Biology, vol. 187, Mar. 2019, pp. 52–57. PubMed, https://doi.org/10.1016/j.jsbmb.2018.10.022.
Newman, Beth, et al. “Possible Genetic Predisposition to Lymphedema after Breast Cancer.” Lymphatic Research and Biology, vol. 10, no. 1, Mar. 2012, pp. 2–13. PubMed Central, https://doi.org/10.1089/lrb.2011.0024.
Olszewski, Waldemar L., et al. “Predilection to Dermato-Lymphangio-Adenitis in Obstructive Lymphedema of Lower Limbs Depending on Genetic Polymorphisms at TNFα-308G>A, CCR2-190G>A, CD14-159C>T, TLR2 2029C>T, TLR4 1063A>G, TLR4 1363C>T, TGFβ 74G>C, and TGFβ 29T>C.” Lymphatic Research and Biology, vol. 16, no. 1, Feb. 2018, pp. 109–16. PubMed, https://doi.org/10.1089/lrb.2016.0040.
Sheikhi-Mobarakeh, Zahra, et al. “Herbs as Old Potential Treatments for Lymphedema Management: A Systematic Review.” Complementary Therapies in Medicine, vol. 55, Dec. 2020, p. 102615. ScienceDirect, https://doi.org/10.1016/j.ctim.2020.102615.
Souza, Patricia R., et al. “Enriched Marine Oil Supplements Increase Peripheral Blood Specialized Pro-Resolving Mediators Concentrations and Reprogram Host Immune Responses: A Randomized Double-Blind Placebo-Controlled Study.” Circulation Research, vol. 126, no. 1, Jan. 2020, pp. 75–90. DOI.org (Crossref), https://doi.org/10.1161/CIRCRESAHA.119.315506.