Key takeaways:
~ Folic acid is a pre-vitamin form of folate that involves a conversion process to be used in your cells.
~ Many people have unmetabolized (unconverted) folic acid in their bloodstream.
~ The DHFR gene is essential in the conversion, and genetic variants in DHFR impact how much folic acid you can convert at one time.
Should you take folic acid if you have MTHFR variants?
There is a lot of buzz online about MTHFR variants and the need to avoid folic acid. I’ve read recommendations ranging from avoiding all foods fortified with folic acid to recommendations that people with MTHFR variants need to take extra folic acid.
What does research tell us about folic acid? Is it so evil that everyone should go out of their way to avoid it? Or is it ok for some of us?
How is folic acid different from folate?
Folic acid, a synthetic pre-vitamin form of folate (vitamin B9), remains both temperature and pH stable, allowing for easy addition to processed foods and multivitamins. The chemical name for folic acid is pteroylmonoglutamic acid or PteGlu.
Natural folates from foods differ a bit from synthetic folic acid. Because natural folates contain more than one glutamic acid, they are called pteroyl polyglutamic acid. They are less heat stable, and cooking or processing can decrease the amount of natural folate in foods.[ref]
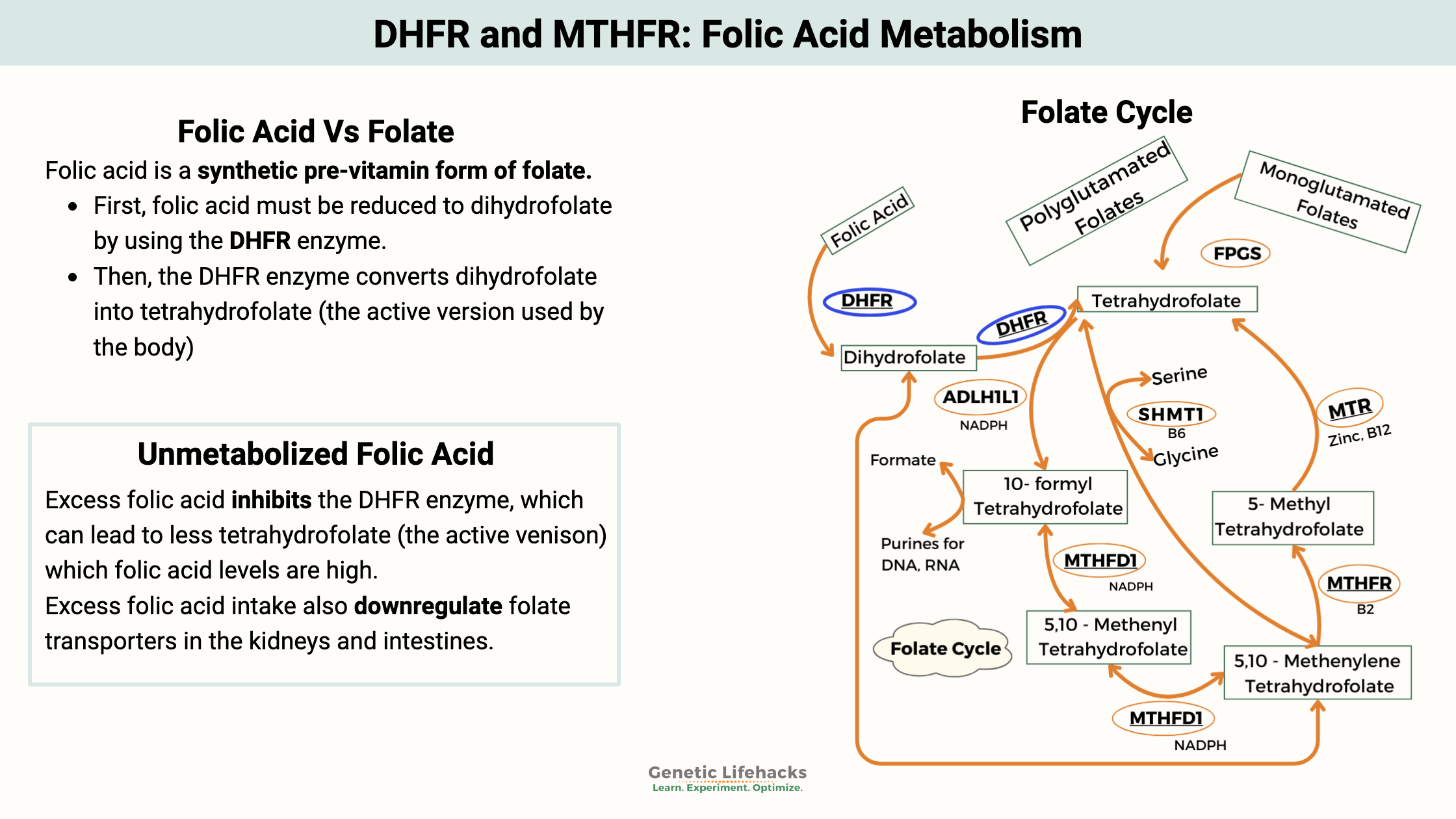
The body converts folates (folic acid and natural folates from plants) into tetrahydrofolate. This conversion process is a little different for natural folate vs. folic acid.
A 2014 review in Preventive Nutrition and Food Science explained the breakdown of folic acid:
- First, folic acid must be reduced to dihydrofolate by using the DHFR enzyme.
- Secondly, the DHFR enzyme converts dihydrofolate into tetrahydrofolate (the active version used by the body).
Tetrahydrofolate, along with the MTHFR enzyme, is required in a critical step within the methylation pathway. This vital pathway’s responsibility includes creating the methyl groups needed in DNA synthesis, detoxification reactions, the creation of certain neurotransmitters, and more.
How is folic acid different from methylfolate?
While folic acid has to go through a couple of reactions to become the active form of folate used by the body, methylfolate (L-5-methyltetrahydrofolate) skips all those steps and can be used immediately.
Methylfolate is available in supplemental forms. However, it isn’t added to fortified foods, in part because it is quite a bit more expensive than folic acid and because it isn’t as stable.
What does DFE mean on the supplement label?
DFE stands for dietary folate equivalent. For folic acid and methylfolate, the conversion is 0.6 mg folic acid/methylfolate = 1 mg folate from food. It is thought that absorption of folic acid is greater than that of folate from foods. [ref]
Example:
400 mcg folic acid = 680 mcg DFE (folate from food)
What happens to folic acid that isn’t used by the body?
Often when reading about folic acid, you will see it mentioned that it is a non-toxic, water-soluble vitamin. This may lead some to assume that extra folic acid won’t hurt you. But this may not be the correct assumption….
The unused folic acid can often be found in the bloodstream as unmetabolized folic acid. There are concerns that excess folic acid could inhibit the DHFR enzyme from converting dihydrofolate into tetrahydrofolate when the body is needing it. Both reactions use the DHFR enzyme, but most of the time, the enzyme is preferentially used for creating the active form (tetrahydrofolate) when needed. Some studies indicate too much unmetabolized folic acid, though, inhibits DHFR from completing that second reaction. This could leave cells lacking in tetrahydrofolate when high levels of folic acid are in circulation.[ref]
There are also concerns that excess folic acid intake could downregulate folate transporters in the kidneys and intestines.[ref]
How much folic acid does it take to get unmetabolized folic acid in the bloodstream?
- One study shows the level is around 400μg for the average adult.[ref]
- Another study completed in the UK, which had not mandated fortification of flour, meant the participants had no unmetabolized folic acid in their bloodstream prior to beginning the study. The study found around 200 μg doses would show up in the bloodstream. The timing was also important, and repeated exposures close together had a cumulative effect.[ref]
- Finally, a 2012 study examining the effects of supplementing with either 1.1mg or 5 mg of folic acid found a great variation in people’s capacity for metabolizing folic acid.[ref]
How much folic acid are people eating?
In the US, flour is fortified at 140 mcg/100g. But since I have no idea how many grams of flour are in most foods, let’s take a look at servings of some popular foods[ref]:
- A bowl of Cheerios gives you 50% of the daily value for folic acid (200mcg?)[website]
- Two slices of bread for a sandwich gives you 70 mcg.
- A bagel contains 119 mcg of folic acid.
- 1 cup of macaroni gives you 179 mcg.
- 1 cup of enriched white rice gives you about 200 mcg, 50% of your daily value for folic acid.
This is just folic acid — keep in mind that foods may contain natural folate as well.
Unmetabolized folic acid in the US population:
A study of over 2,700 US children, adolescents, and adults found unmetabolized folic acid in almost all blood samples.[ref]
Does folic acid cause cancer?
Folate is needed for cells to reproduce and grow, and cancer cells can use a lot of folate.
The question of whether added folic acid increases cancer rates is one that researchers have been looking into for a few decades. It’s a controversial topic without totally clear answers.
The mandating of folic acid fortification in 1998 correlates to an increase in the number of colon cancer cases in the US. The sharp increase in colon cancers from 1998-2002 came after a long period when colon cancer rates had been declining.[article][ref]
Recent studies show folic acid in higher amounts, such as 1mg/day, has links to breast cancer, prostate cancer, and colon cancer.[ref]
High amounts of unmetabolized folic acid are also associated with decreased natural killer cells (a cytokine that is part of the body’s defense against cancer).[ref]
People with a higher daily intake of folate (dietary folate along with some fortified foods with folic acid) have an increased risk of skin cancers.[ref]
One commonly used cancer-fighting drug is methotrexate, which blocks the action of an enzyme (DHFR) that is part of the folate pathway. This essentially inhibits the synthesis of DNA, RNA, and more in cancer cells — and healthy cells.
Here are a few of the studies on cancer and folic acid:
- A study of 848 women with breast cancer and a control group of 28,345 women without cancer found premenopausal women with higher plasma folate levels were at a higher risk of breast cancer. The study was to determine if B12 and folate prevented breast cancers; researchers noted the results were ‘unexpected’.[ref]
- Another study found women with higher plasma folate levels (top third) were at double the odds of ERβ− breast cancer.[ref]
- A 2009 randomized placebo-controlled trial for colorectal adenomas found folic acid supplementation (1 mg/day) more than doubled the risk of prostate cancer. “Among the 643 men who were randomly assigned to placebo or supplementation with folic acid, the estimated probability of being diagnosed with prostate cancer over a 10-year period was 9.7% (95% confidence interval [CI] = 6.5% to 14.5%) in the folic acid group and 3.3% (95% CI = 1.7% to 6.4%) in the placebo group “.[ref]
- Animal studies can point to the mechanisms of how folic acid affects tumor growth. A study in animals with mammary tumors showed that a diet containing higher amounts of folic acid (2.5 to 5 times the recommended amount) increased tumor size.[ref] Another animal model of breast cancer also found that a high folic acid diet increased tumor volume significantly.[ref]
Don’t freak out or just stop eating folate altogether... Folate in the right amounts has been repeatedly shown to reduce the risk of getting cancer. The key here seems to be that adding folic acid when there is cancer already present will increase the growth of cancer.
Does folic acid cause autism?
This is another controversial topic and again without a clear answer.
A meta-analysis that combined data from multiple studies showed the overall effect of supplementing with folic acid while pregnant reduces the risk of autism.[ref]
Other studies, though, raise some serious questions about folic acid on an individual level. A study of 1,391 mothers in Boston found that really high maternal folate and/or B12 levels significantly increased the risk of autism in their children. Overall, though, women using multivitamins were at a lower risk. The researchers did factor in MTHFR genetic variants and found they were not a risk factor.[ref]
Mouse studies also raised questions about the impact of higher levels of folic acid during pregnancy. The results showed high folic acid during pregnancy leads the offspring to have disturbed choline/methyl metabolism, memory impairment, and embryonic growth delays.[ref]
History of how Folic Acid came to be supplemented in the US:
Widespread folic acid fortification began in the US in 1996 and then became mandatory in 1998. It is currently added to all “enriched bread, flour, cornmeal, rice, pasta, and other grain products”.[ref] This mandate was made to reduce the risk of neural tube defects, which happened at the rate of 2,500 babies with NTD/year in the US in 1992. A 2015 CDC article claims: “The birth prevalence of NTDs (proportion of babies in the population born with an NTD) has decreased by 35% in the United States since folic acid fortification was required in 1998.”[ref]
The history of the FDA’s decision to mandate fortification with folic acid is interesting to read. It states that:
“Folic acid fortification, for all practical purposes, was not even on the regulatory horizon when it was first included in the 1990 Nutrition Labeling and Education Act (NLEA). FDA scientists at the time felt that the charge to consider the link between folic acid and neural tube defects literally came “out of the blue.” Later, they concluded it probably started with a science workshop hosted by CDC in the late 80s in which unpublished data on folic acid and neural tube defects were presented and seized upon by the supplement industry.” The article goes on to explain that a British study published in 1991 showed women who already had a child with neural tube defects reduced their risk of having a second child with NDT when they supplemented with 4 mg of folic acid per day. This study was in contrast to the FDA contracted report in 1991, which stated that studies had failed to show the connection between folic acid and NTD.
By August of 1992, the FDA had changed its stance on folic acid. The article goes on to say:
“In August and September 1992, FDA reviewed results obtained from two additional, unpublished studies, and worked closely with authors and journals publishing them to ensure that the results were made public early. The first, a Hungarian research study, showed a reduced risk of ntd’s in women consuming .8 mg. of folic acid as part of a multivitamin/mineral supplement. The study had been conducted with a sample of women in the general population without a previous history of an ntd pregnancy. The second study was a case-control study of women in the general population of Boston, Toronto, and Philadelphia and was referred to as the “Werler study.” This study suggested that .4 mg. of folic acid daily from multivitamin/mineral supplements was associated with a reduced risk of ntd. It also suggested that a diet adequate in folate with more than .25 mg. daily was protective. The new preponderance of scientific evidence on folic acid created a platform from which the Public Health Service (PHS) spoke on September 14, 1992. PHS formally recognized the link between folic acid intake and ntd’s as a compelling public health issue. It recommended that all women of childbearing age should have adequate folate intakes (.4 mg. daily) throughout their childbearing years, but warned that the total intakes should not exceed 1 mg.”
The Werler study that the FDA used for their recommendation looked at 436 cases of NTD with a control group of 2,615 babies that had other types of birth defects. They based the conclusion on the reported use of daily multivitamins containing folic acid. I admit I am confused by this study, specifically by why the control group was only babies with birth defects and how the conclusion was reached that it was the folic acid in the multivitamin that lowered the risk of NTD.
Please don’t get me wrong… I am not questioning a link between NTD and folate levels since there is other evidence for this. The CDC estimates folic acid fortification in the US prevents 1,300+ cases of NTD each year.[ref] (You can decide if it is a good trade-off for possibly increased cancer risk.)
Instead, I’m surprised at how little data the FDA used in making the decision to force the fortification of folic acid on the public. I had rather naively assumed there were lots of good studies showing without a doubt that 400 μg/day of folic acid was exactly what we all needed.
Folic Acid Genotype Report:
Lifehacks: Folic acid, folate, or methylfolate
Here are some common-sense ways to apply the research on the DHFR SNPs.
Figure out how much folic acid you get in a day:
I think caution is warranted for higher doses of folic acid, especially in older people or anyone at a higher risk for cancer.
Related article: Are you getting too much folate?
The question remains whether a “higher dose” is 200 mcg or 400 mcg since the studies referenced above showed different answers for the point at which unmetabolized folic acid is found. My guess is that for anyone with a DHFR variant, that is on the lower side if you eat a diet that also contains sufficient folate.
Be sure to check the ingredient labels on multivitamins, prepackaged shakes, vitamin drinks, etc., to see how much you are getting.
The European Union set the upper limit for folic acid and/or methylfolate at 1,000 mcg (1mg)/day.[ref]
What about prenatal vitamins?
The research is pretty clear that women trying to conceive during the first trimester need plenty of folate, but this doesn’t mean that folic acid is your only option. There are many options now for prenatal vitamins with methylfolate rather than folic acid.
What about MTHFR? Should I limit folic acid due to having MTHFR SNPs?
Related Articles and Topics: