Key takeaways:
~ Medium-chain acyl-CoA dehydrogenase enzyme deficiency makes it hard to use medium-chain fats for energy or to fast and go into ketosis.
~ MCAD deficiency is caused by two copies of mutations in the ACADM gene. It is usually discovered in infant blood screenings.
~ People with one copy of an ACADM mutation may have mild symptoms, including problems with a ketogenic diet.
Members will see their genotype report below, plus additional solutions in the Lifehacks section. Consider joining today.
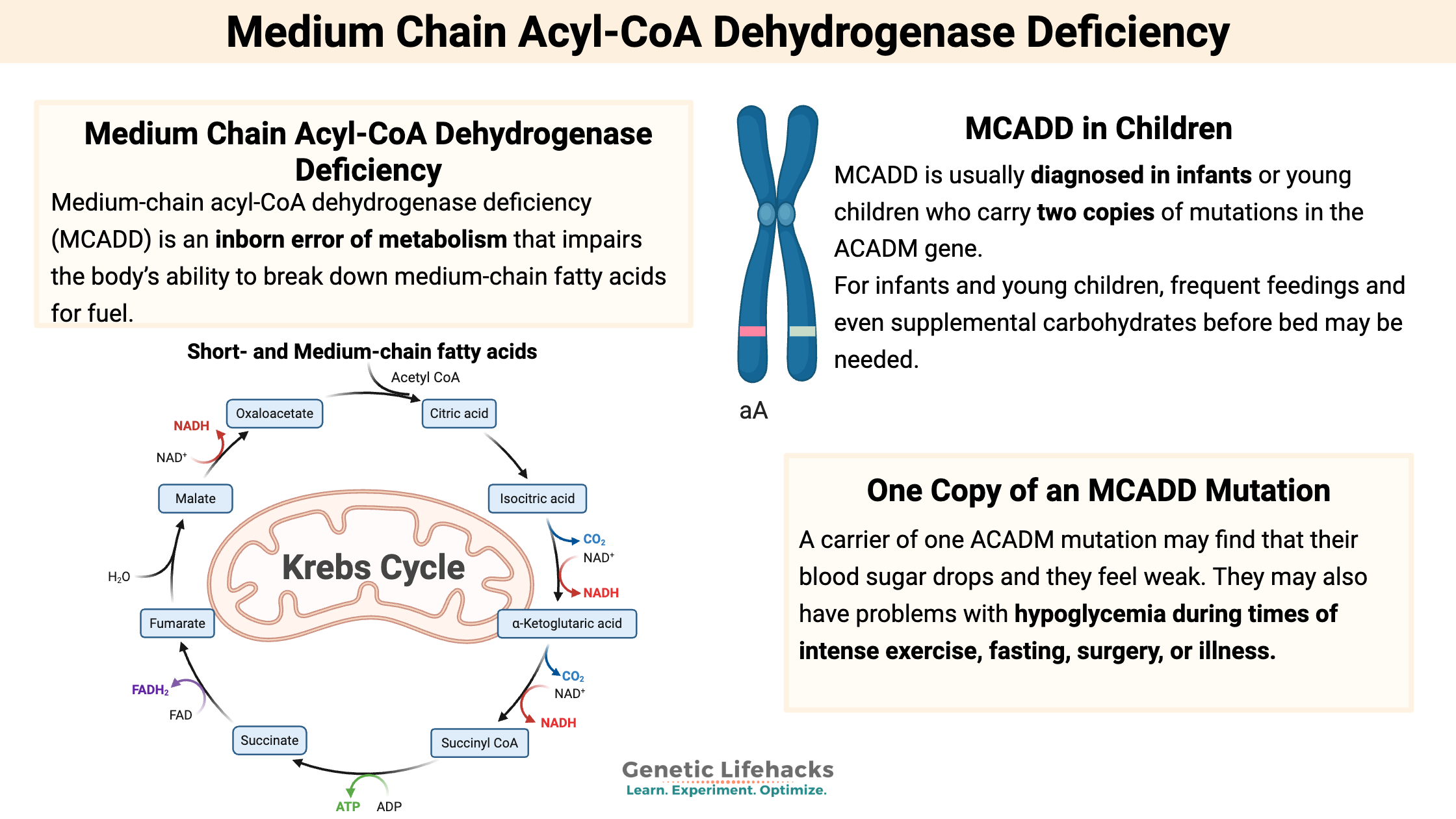
What is medium-chain acyl-CoA dehydrogenase deficiency?
Medium-chain acyl-CoA dehydrogenase deficiency (MCADD) is an inborn error of metabolism that impairs the body’s ability to break down medium-chain fatty acids for fuel.
Cells can use either glucose (through glycolysis) or fatty acids (through beta-oxidation) as the basis for producing energy in the mitochondria in the form of ATP.
Medium-chain acyl-CoA dehydrogenase affects the body’s ability to efficiently use medium-chain fatty acids for energy.
Medium-chain fatty acids are naturally found in coconut oil, palm oil, and dairy. They are defined as having 6 to 12 carbon atoms:
- C6:0 (caproic acid)
- C8:0 (caprylic acid)
- C10:0 (capric acid)
- C12:0 (lauric acid)
MCADD in infants and children:
MCADD is an autosomal recessive genetic disorder. It is usually diagnosed in infants or young children who carry two copies of mutations in the ACADM gene. Without the ability to break down medium-chain fatty acids, there’s a buildup of the unused fatty acids and a decrease in cellular energy production.
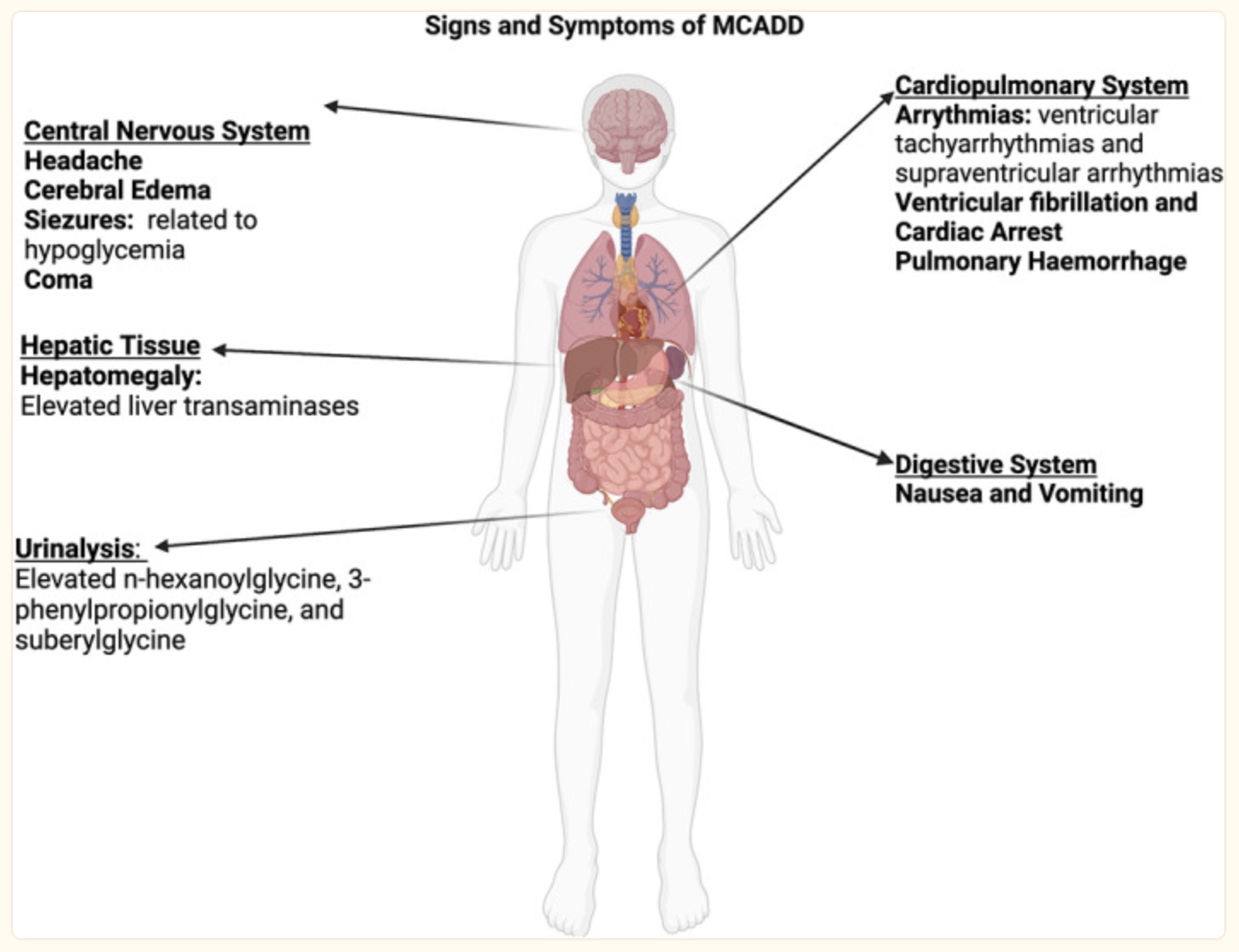
Symptoms of MCADD generally occur when an infant or child hasn’t eaten, often due to being sick with a cold, ear infection, or the flu. Because the body can’t utilize fatty acids efficiently for energy, children with MCADD can’t switch to using fatty acids for energy. They will end up having severe hypoglycemia (low blood sugar), which can progress into a more serious metabolic crisis.[ref] Often, the onset of MCADD happens during an illness (viral, bacterial) because the immune system needs a lot of energy, while at the same time, the child usually doesn’t feel like eating.
Not every child who has genetic mutations for MCADD ends up having problems with medium-chain acyl-CoA dehydrogenase deficiency. Newborn screenings are done to identify infants with MCAD deficiency.[ref]
For infants and young children, frequent feedings and even supplemental carbohydrates before bed may be needed. In older individuals, skipping meals and fasting is not recommended. For prolonged exercise, adequate carbohydrate intake and staying hydrated are important.[ref]
Under normal circumstances and while eating a regular diet, MCADD patients can compensate for the lack of beta-oxidation by using glycogen from the liver. However, some studies show that people with MCADD have overall impaired mitochondrial function in their skeletal muscles, which can result in muscle weakness.[ref]
Carnitine deficiency is a common occurrence in MCADD patients with more severe phenotypes and high concentrations of toxic acetylcarnitine.[ref]
Carrying one copy of an MCADD mutation:
It is now being recognized that people who carry one copy of an ACADM gene mutation may also have problems with hypoglycemia during times of intense exercise, fasting, surgery, or illness. When your body may rely only on fatty acids instead of glucose for energy, a carrier of one ACADM mutation may find that their blood sugar drops and they feel weak.[ref][ref][ref][ref]
People with one copy of the mutation may have no problems at all under normal conditions since fatty acid oxidation should still work — just at a less-than-optimal level.
Research shows that MCADD can be more of a spectrum than previously thought. Carrying one mutation may cause a very mild form of the disease, while someone with two different mutations may have a moderate form of MCADD. Environmental and lifestyle factors also come into play.[ref]
Organic acid tests:
An organic acid test (OAT) analyzes the byproducts of cellular metabolism. It is often used to assess how well different metabolic functions are working in the body.
If MCADD or partial deficiency is suspected, a common finding on the organic acid test is that ketones are low and the medium-chain dicarboxylic acids are elevated with a characteristic pattern: hexanoylglycine (C6) is higher than octanoylglycine (C8), which is higher than decanoylglycine (C10).[ref]
If you see lower-than-expected ketones on an OAT test without the altered medium-chain fatty acid metabolites, be sure to also check for Short Chain Acyl-CoA Dehydrogenase Deficiency and Long Chain Acyl-CoA Dehydrogenase Deficiency mutations.
Interesting tidbit: King Charles Spaniel is a dog breed that is more likely to have mutations causing MCADD. One study showed that almost 1 in 10 King Charles Spaniels likely have at least a mild form.[ref]
MCADD Genotype Report:
Access this content:
An active subscription is required to access this content.
Lifehacks:
Nutrition and lifestyle considerations:
If you are a carrier (heterozygous) for one of the MCAD deficiency mutations, you may find that a diet that is higher in carbohydrates and protein, and lower in fat, may work better for you. In this era of carbs being demonized, MCADD carriers may need to buck the keto trend — or at least be alert for signs of hypoglycemia if eating a low-carb diet.
Coconut oil is really high in medium-chain fatty acids and is recommended to be avoided by people with MCADD.[ref]
Falling blood sugar levels:
The key is to keep an eye out for signs of low blood sugar. If you exercise hard, eating before a workout may be beneficial.
Alcohol interaction:
Anecdotally, drinking a lot of alcohol without eating anything can also cause hypoglycemia in people with one copy of the MCAD mutation.
Access this content:
An active subscription is required to access this content.
Related Articles and Topics:
References: