Researchers recently posted a preprint publication showing that blood type seems to be related to susceptibility to the coronavirus. While this may seem odd at first, there are actually quite a few viral and bacterial pathogens – as well as chronic diseases – that are influenced by blood type.
Researchers recently posted a preprint publication showing that blood type seems to be related to susceptibility to the coronavirus. While this may seem odd at first, there are actually quite a few viral and bacterial pathogens – as well as chronic diseases – that are influenced by blood type.
This article explains how your blood type can influence cardiovascular disease and diabetes and how your immune response is linked to your blood type. We will wrap up with an explanation of the preprint article on COVID-19 and blood type, along with research from the original SARS outbreak that may shed some light on this link.
Blood groups and pathogen susceptibility
Let me start off with a quick explanation of blood groups (skip ahead if you know all of this). There are actually many different blood groups, but for this explanation, I’m going to focus only on ABO typing.
ABO blood types:
There are four ABO blood types: A, B, AB, or O.
All cells have a type of glycoproteins called an antigen on the plasma membranes. Your immune system recognizes these antigens as marking the cells as being ‘self’. In contrast, antigens on the surface of invading pathogenic bacteria or viruses are recognized as being foreign and then attacked by your immune system.
On red blood cells (RBCs) there is a specific type of antigen called and agglutinogen. A type has A antigens, B type has B antigens, AB has both, and O has no antigens.
People with type A blood produce the A antigen and have antibodies that react against type B blood. People with type B blood produce the B antigen and have antibodies that react against type A blood. Type AB, the rarest blood type, has both antigens produced and creates no antibodies. Type O blood produces no antigens but has antibodies against both A and B.
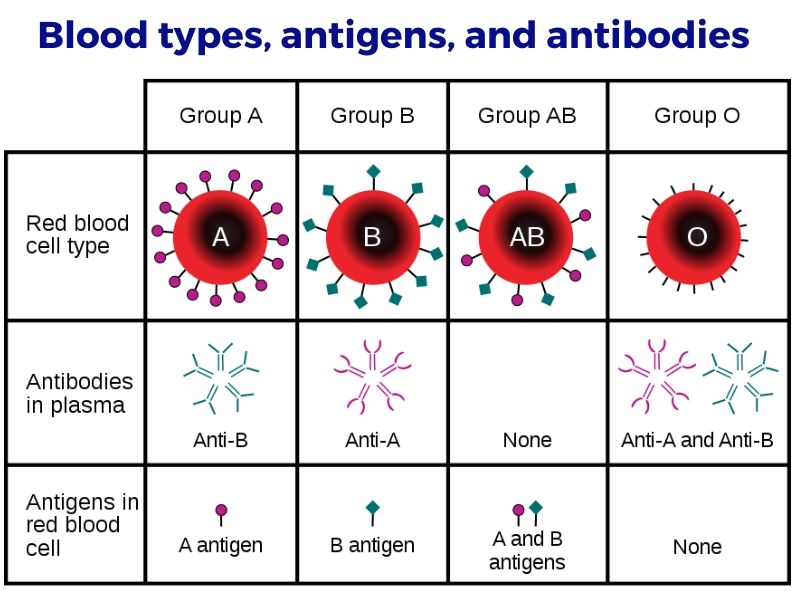
While we refer to this as your ABO blood type, these antigens are also found on platelets, leukocytes, plasma proteins, certain tissues, and some cell surface enzymes. Also, the antigens exist in a soluble form, not connected to the cell surface, and this can be secreted (by the majority of people) in the sweat, saliva, breast milk, urine, and gastric secretions. [ref]
While pictures of red blood cells may show these antigens as a few little spikes, each red blood cell can be decorated with about 2 million of the antigens for the ABO blood type. [ref]
A quick history time-out:
Blood types were first identified in the early 1900s. It had been observed that mixing some individual’s blood with others would cause agglutination – clumping together of red blood cells. By the mid-1940s, a test had been developed to determine which types of antibodies were in the blood, thus paving the way for blood transfusions.
It is hard to imagine in this day and age of genetic testing, machine learning, and world-wide connectivity that blood typing is such a relatively recent concept.
Digging into the specifics:
These antigens are made up of glycoproteins – a sugar molecule chain called an oligosaccharide with a protein. The oligosaccharides differ in the sugar molecule at the end of the chain, and this is what determines the A antigen and B antigen (with the lack of either being type O).
The A and B antigens come in two types (Type I and II). Type I antigens are the main type that is secreted by about 80% of the population in their saliva, mucus, semen, etc. The Type II antigens are present on red blood cells (e.g. different ones for type A vs type B) and also on epithelial cells and endothelial cells.[ref]
Getting a little bit deeper there, there are actually two types of blood type A antigens – A1 and A2. “A1 red cells express about 5 times more A antigen than A2 red cells…” [ref]
Infants are usually born without anti-A or anti-B antibodies. They develop the antibodies as they are exposed to bacteria and their immune system develops. [ref]
Variations by population group:
The percentage of a population who carries each blood type varies considerably from one play to another.
Keep in mind that people with type A blood can carry either two A alleles or an A and an O allele. Similarly, type B can carry either two B alleles or a BO combination. People with type O blood carry two O alleles.
Here is a map of the distribution of type A allele among native populations:
Here is a map of type B alleles among native populations:
Finally, a map of type O alleles by native population:
Want to dive deeper into this? Here is a breakdown by current country populations and by ethnic group.
Chronic conditions in which blood type matters:
The rest of this article is for Genetic Lifehacks members only. Consider joining today to see the rest of this article.
Related Genes and Topics:
Acute Respiratory Distress Syndrome (ARDS) genes
ARDS is caused by an overwhelming immune response to a virus, bacteria, or lung injury. Learn more about which of your immune system genes are involved in ARDS.
Viral Immunity: Your genes protect you
Your genetic variants shape your immune system and give you superpowers against some pathogens – and perhaps more susceptible to others.
Non-secretors: Norovirus resistance and gut microbiome
A genetic variant in the FUT2 gene controls whether or not you secrete your blood type into your saliva and other bodily fluids, such as your intestinal mucosa. This alters the gut microbiome – and protects you from Norovirus.
Hemochromatosis – Too Much Iron
A couple of common mutations can cause you to build up iron, leading to iron overload or hemochromatosis. This is one genetic disease where knowledge is really powerful – you can completely prevent hemochromatosis through blood donations.