Key takeaways:
~ BDNF (brain-derived neurotrophic factor) and serotonin are important for brain health and mood regulation.
~ A brain imaging study showed that the combination of a BDNF genetic variant plus a serotonin receptor variant physically changes the brain.
~The combination of these two variants interacts to increase the risk of depression, anxiety, and bipolar disorder.
BDNF + Serotonin receptor variants:
Mood disorders such as depression or anxiety are complicated. While it would be nice if you could just point to a specific SNP and say, “this causes my depression”, the reality is more complex. Genetic variants interact with each other and also with your environment.
| Factor | Role in Brain | Low Levels | Influenced By |
|---|---|---|---|
| BDNF | Promotes neuron growth, protects neurons, enhances plasticity | Linked to depression, cognitive decline, obesity | Genetics, stress, sleep, exercise, sunlight |
| Serotonin | Regulates mood, sleep, cognition | Linked to depression, anxiety, mood disorders | Genetics, diet (tryptophan), circadian rhythm |
Background on BDNF:
For a long time, people thought that you couldn’t add brain cells as an adult. However, research now shows new neurons form throughout life in certain areas of your brain, especially in the hippocampus. You can also increase the connections between the neurons, increasing the brain’s plasticity, and BDNF is a major part of this.
BDNF is a key to producing more neurons.
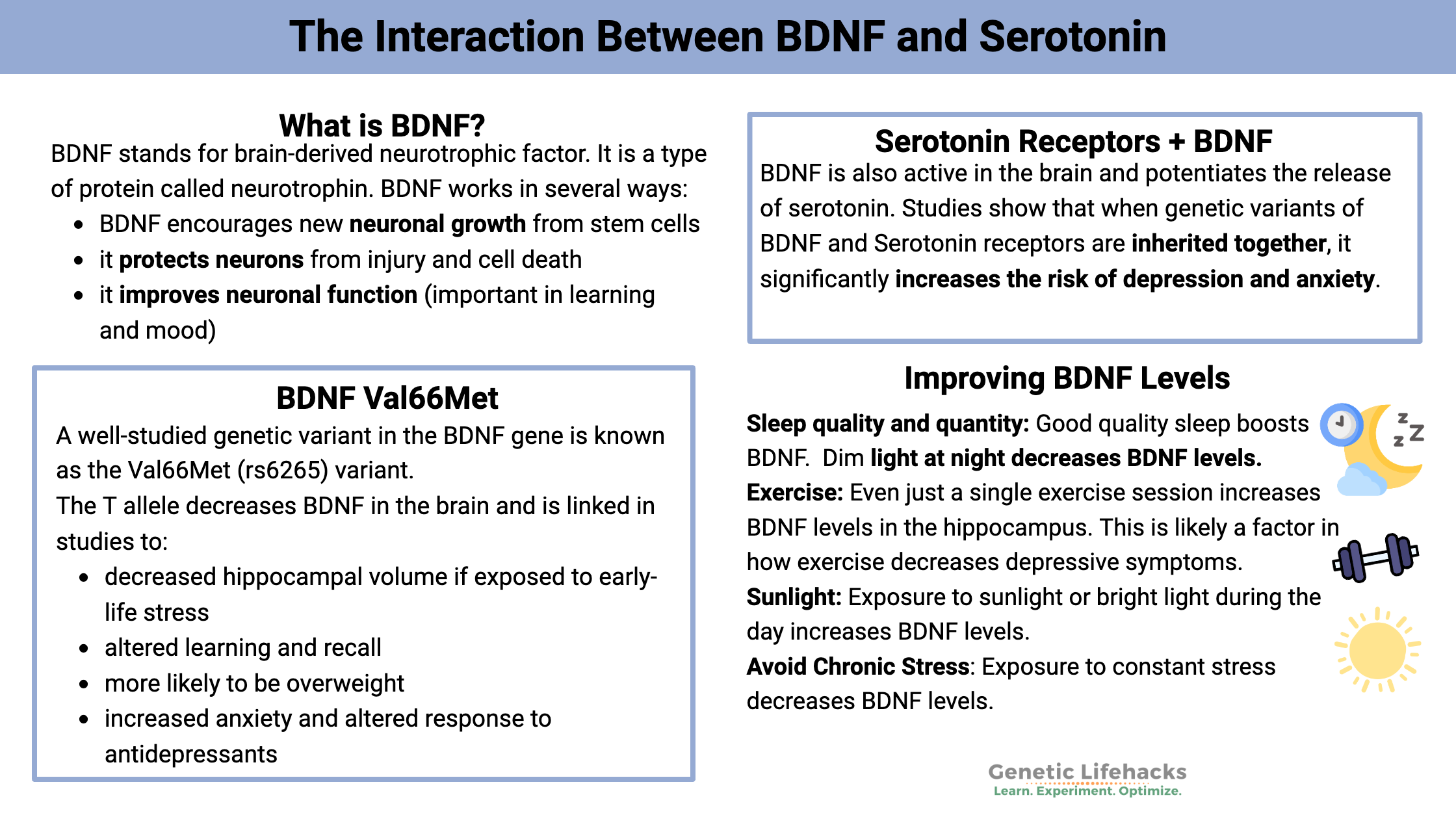
BDNF stands for brain-derived neurotrophic factor. It is a type of protein called a neurotrophin. BDNF works in several ways:
- BDNF encourages new neuronal growth from stem cells
- It protects neurons from injury and cell death
- It improves neuronal function (important in learning and mood)
To improve the way the neurons function, BDNF binds to receptors that are located in the synapses between neurons. BDNF potentiates or increases the signal from one neuron to the next.
In addition to being found in the brain, BDNF is also found in the peripheral nervous system, helping muscle nerves to function well throughout the body.
The connection with muscles is one way that exercise increases BDNF throughout the body and in the brain.
Studies on BDNF show:
- Chronic stress causes a decrease in BDNF.[ref]
- Low BDNF is linked to Alzheimer’s disease[ref] and Parkinson’s[ref][ref]
- People with depression usually have lower levels of BDNF.[ref][ref][ref]
- Mothers with postpartum or during-pregnancy depression have low BDNF[ref], and the elderly with depression also have low BDNF.[ref]
- Low BDNF is linked to obesity.[ref]
BDNF doesn’t necessarily act alone in causing diseases. It often interacts with neurotransmitters or cytokines. For example, a recent study found that in people with schizophrenia, lower BDNF levels correlated with higher IL-2 (interleukin-2) levels. IL-2 is an inflammatory cytokine that is part of the immune system.[ref]
~ BDNF is essential for neuron growth, protection, and function.
~ Low BDNF is associated with depression, neurodegenerative diseases, and obesity
BDNF Genotype Report:
The BDNF Val66Met (rs6265) variant has thousands of studies on it.
Check your genetic data for rs6265 (23andMe v4, v5; AncestryDNA):
- T/T: decreased BDNF[ref] referred to in studies as Met/Met
- C/T: somewhat decreased BDNF, referred to as Val/Met
- C/C: typical BDNF, referred to as Val/Val
Members: Your genotype for rs6265 is —.
The T allele (decreased BDNF in the brain) is linked in studies to:
- decreased hippocampal volume if exposed to early-life stress[ref]
- altered learning and recall[ref][ref]
- more likely to be overweight[ref]
- increased anxiety and altered response to antidepressants[ref]
- less likely to respond to citalopram and escitalopram (antidepressants).[ref] Note that this doesn’t mean that those antidepressants absolutely won’t work, just that a larger proportion of people carrying the T allele didn’t respond compared with people carrying the C/C genotype
Not all studies show that the rs6265 T allele affects depression or anxiety.[ref]
Interactions with BDNF – both positive and negative:
There are a lot of conflicting studies that muddy the water… It isn’t as simple as T-allele = bad brain.
- First, lifestyle factors increase or decrease BDNF (more on these in the Lifehacks section below).
- Second, other genetic variants are important. Such as the serotonin gene variant below.
- Third, the T-allele is also linked with positive traits, such as being more resistant to social defeat.[ref] The song lyrics “I get knocked down, but I get up again, You are never gonna keep me down…” may apply to people with the T-allele.
Background on Serotonin:
Serotonin is often thought of as a happy neurotransmitter and is linked to feelings of well-being. (Serotonin does many things in the body and is not just in the brain. But here, I’m just focusing on its role as a brain neurotransmitter.)
Tons of research exists showing links between serotonin and depression; however, it isn’t fully understood how and why depression is linked to serotonin. (Yep, pretty wishy-washy for decades of research.) Again, it doesn’t seem like there are simple answers here, such as simply increasing serotonin to cure depression.
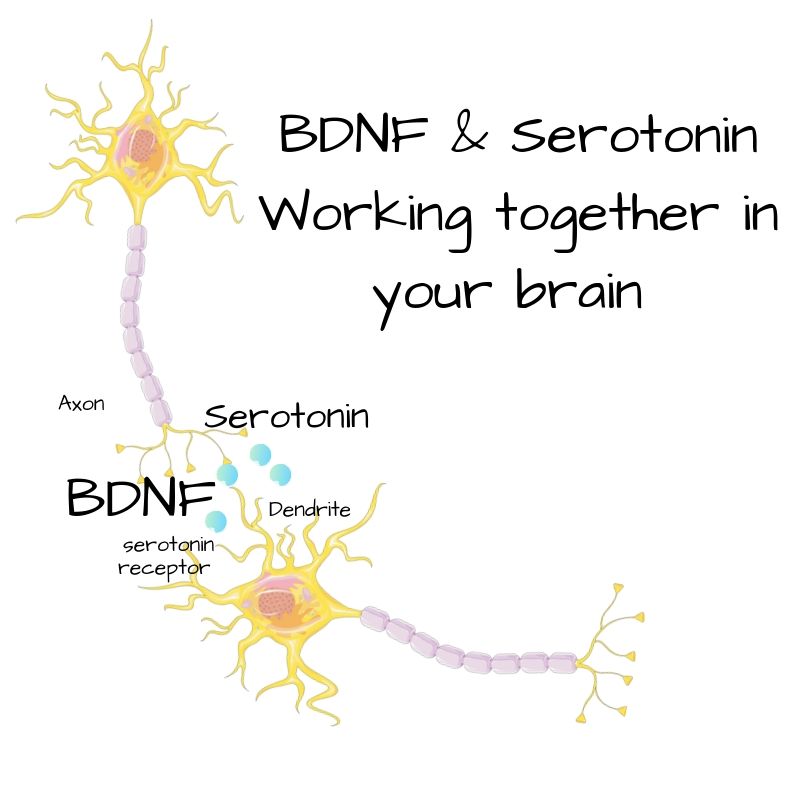
Serotonin works as a neurotransmitter to transmit signals in a variety of neurons in the brain. It is released by a neuron into the synapses and then binds to the next neuron, causing the signal to be transmitted.
Whole books could be (and have been) written on serotonin and depression. Instead of getting too deep into the weeds here, I’m going to dive into one specific serotonin receptor…
HTR1A Serotonin Receptor:
The serotonin receptor known as 5-HT1A is coded for by the HTR1A gene. Here, I’m just going to call it the serotonin 1A receptor. (There are a bunch of different serotonin receptors that do different things in the body.)
Basically, one neuron releases serotonin into the space (synapse) next to the beginning of the next neuron. Then serotonin binds to receptors on the next neuron, triggering a reaction that sends the signal along. The receptors are specific to serotonin — in this case, we’re talking about the serotonin 1A receptor.
BDNF is also active in the brain and potentiates the release of serotonin.[ref] It gives it a boost. Like adding nitrous to your car. OK, maybe not that big of a boost.
Research shows the serotonin 1A receptor variant has links to depression. A new study now points to an interaction between the serotonin receptor variant and the BDNF variant when it comes to depression.
Access this content:
An active subscription is required to access this content.
Related Articles and Topics:
- Bipolar disorder and the circadian clock genes:
New research shows that depression and bipolar disorder are linked to changes or disruptions in circadian genes. Some people carry genetic variants in the circadian genes that make them more susceptible to circadian disruption. - Tryptophan:
Tryptophan is an amino acid that the body uses to make serotonin and melatonin. Genetic variants can impact the amount of tryptophan that is used for serotonin. This can influence mood, sleep, neurotransmitters, and immune response. - Circadian Rhythm Genes: Mood Disorders
Circadian rhythm disruption can drive mood disorders. Learn more about the genes involved and the ways to normalize your circadian rhythm. - Anxiety: Genetics and personalized solutions
This article covers genetic variants related to anxiety disorders. Genetic variants combine with environmental factors (nutrition, sleep, relationships, etc.) when it comes to anxiety. There is not a single “anxiety gene”. Instead, there are many genes that can be involved – and many genetic pathways to target for solutions.
References:
Albert, Paul R., et al. “Genetic, Epigenetic and Posttranscriptional Mechanisms for Treatment of Major Depression: The 5-HT1A Receptor Gene as a Paradigm.” Journal of Psychiatry & Neuroscience : JPN, vol. 44, no. 3, May 2019, pp. 164–76. PubMed Central, https://doi.org/10.1503/jpn.180209.
Avgan, Nesli, et al. “BDNF Variants May Modulate Long-Term Visual Memory Performance in a Healthy Cohort.” International Journal of Molecular Sciences, vol. 18, no. 3, Mar. 2017, p. E655. PubMed, https://doi.org/10.3390/ijms18030655.
Chen, Zhe-Yu, et al. “Genetic Variant BDNF (Val66Met) Polymorphism Alters Anxiety-Related Behavior.” Science (New York, N.Y.), vol. 314, no. 5796, Oct. 2006, pp. 140–43. PubMed, https://doi.org/10.1126/science.1129663.
Chui, D. H., et al. “A Double-Blind, Rct Testing Beneficial Modulation of BDNF in Middle-Aged, Life Style-Stressed Subjects: A Clue to Brain Protection?” Journal of Clinical and Diagnostic Research: JCDR, vol. 8, no. 11, Nov. 2014, pp. MC01-06. PubMed, https://doi.org/10.7860/JCDR/2014/10301.5141.
Dinoff, Adam, et al. “The Effect of Acute Exercise on Blood Concentrations of Brain-Derived Neurotrophic Factor in Healthy Adults: A Meta-Analysis.” The European Journal of Neuroscience, vol. 46, no. 1, July 2017, pp. 1635–46. PubMed, https://doi.org/10.1111/ejn.13603.
Duman, Ronald S., and Lisa M. Monteggia. “A Neurotrophic Model for Stress-Related Mood Disorders.” Biological Psychiatry, vol. 59, no. 12, June 2006, pp. 1116–27. ScienceDirect, https://doi.org/10.1016/j.biopsych.2006.02.013.
Dwivedi, Yogesh. “Involvement of Brain-Derived Neurotrophic Factor in Late-Life Depression.” The American Journal of Geriatric Psychiatry : Official Journal of the American Association for Geriatric Psychiatry, vol. 21, no. 5, May 2013, pp. 433–49. PubMed Central, https://doi.org/10.1016/j.jagp.2012.10.026.
Fonken, Laura K., and Randy J. Nelson. “Dim Light at Night Increases Depressive-like Responses in Male C3H/HeNHsd Mice.” Behavioural Brain Research, vol. 243, Apr. 2013, pp. 74–78. PubMed, https://doi.org/10.1016/j.bbr.2012.12.046.
Gatt, J. M., et al. “Interactions between BDNF Val66Met Polymorphism and Early Life Stress Predict Brain and Arousal Pathways to Syndromal Depression and Anxiety.” Molecular Psychiatry, vol. 14, no. 7, July 2009, pp. 681–95. www.nature.com, https://doi.org/10.1038/mp.2008.143.
Goggi, Julian, et al. “Modulation of Neurotransmitter Release Induced by Brain-Derived Neurotrophic Factor in Rat Brain Striatal Slices in Vitro.” Brain Research, vol. 941, no. 1–2, June 2002, pp. 34–42. PubMed, https://doi.org/10.1016/s0006-8993(02)02505-2.
Goldberg, Terry E., et al. “BDNF Val66Met Polymorphism Significantly Affects d’ in Verbal Recognition Memory at Short and Long Delays.” Biological Psychology, vol. 77, no. 1, Jan. 2008, pp. 20–24. PubMed, https://doi.org/10.1016/j.biopsycho.2007.08.009.
Hettema, J. M., et al. “Association Study between the Serotonin 1A Receptor (HTR1A) Gene and Neuroticism, Major Depression, and Anxiety Disorders.” American Journal of Medical Genetics. Part B, Neuropsychiatric Genetics: The Official Publication of the International Society of Psychiatric Genetics, vol. 147B, no. 5, July 2008, pp. 661–66. PubMed, https://doi.org/10.1002/ajmg.b.30656.
Hock, C., et al. “Region-Specific Neurotrophin Imbalances in Alzheimer Disease: Decreased Levels of Brain-Derived Neurotrophic Factor and Increased Levels of Nerve Growth Factor in Hippocampus and Cortical Areas.” Archives of Neurology, vol. 57, no. 6, June 2000, pp. 846–51. PubMed, https://doi.org/10.1001/archneur.57.6.846.
Karege, Félicien, et al. “Low Brain-Derived Neurotrophic Factor (BDNF) Levels in Serum of Depressed Patients Probably Results from Lowered Platelet BDNF Release Unrelated to Platelet Reactivity.” Biological Psychiatry, vol. 57, no. 9, May 2005, pp. 1068–72. PubMed, https://doi.org/10.1016/j.biopsych.2005.01.008.
Kautzky, Alexander, et al. “Epistasis of HTR1A and BDNF Risk Genes Alters Cortical 5-HT1A Receptor Binding: PET Results Link Genotype to Molecular Phenotype in Depression.” Translational Psychiatry, vol. 9, Jan. 2019, p. 5. PubMed Central, https://doi.org/10.1038/s41398-018-0308-2.
Kishi, Taro, et al. “Serotonin 1A Receptor Gene and Major Depressive Disorder: An Association Study and Meta-Analysis.” Journal of Human Genetics, vol. 54, no. 11, Nov. 2009, pp. 629–33. PubMed, https://doi.org/10.1038/jhg.2009.84.
Krishnan, Vaishnav, et al. “Molecular Adaptations Underlying Susceptibility and Resistance to Social Defeat in Brain Reward Regions.” Cell, vol. 131, no. 2, Oct. 2007, pp. 391–404. www.cell.com, https://doi.org/10.1016/j.cell.2007.09.018.
Li, I.-Chen, et al. “Neurohealth Properties of Hericium Erinaceus Mycelia Enriched with Erinacines.” Behavioural Neurology, vol. 2018, May 2018, p. 5802634. PubMed Central, https://doi.org/10.1155/2018/5802634.
Ma, Xian-Yong, et al. “Association between BDNF Rs6265 and Obesity in the Boston Puerto Rican Health Study.” Journal of Obesity, vol. 2012, Dec. 2012, p. e102942. www.hindawi.com, https://doi.org/10.1155/2012/102942.
Mandelman, Samuel D., and Elena L. Grigorenko. “BDNF Val66Met and Cognition: All, None, or Some? A Meta-Analysis of the Genetic Association.” Genes, Brain, and Behavior, vol. 11, no. 2, Mar. 2012, pp. 127–36. PubMed Central, https://doi.org/10.1111/j.1601-183X.2011.00738.x.
Mandolini, G. M., et al. “Association between Serum BDNF Levels and Maternal Perinatal Depression: A Review: Special Section on ‘Translational and Neuroscience Studies in Affective Disorders’ Section Editor, Maria Nobile MD, PhD.” Journal of Affective Disorders, vol. 261, Jan. 2020, pp. 271–76. ScienceDirect, https://doi.org/10.1016/j.jad.2019.08.007.
Miranda, Magdalena, et al. “Brain-Derived Neurotrophic Factor: A Key Molecule for Memory in the Healthy and the Pathological Brain.” Frontiers in Cellular Neuroscience, vol. 13, Aug. 2019, p. 363. PubMed Central, https://doi.org/10.3389/fncel.2019.00363.
Molendijk, Marc L., et al. “Serum BDNF Concentrations Show Strong Seasonal Variation and Correlations with the Amount of Ambient Sunlight.” PLoS ONE, vol. 7, no. 11, Nov. 2012, p. e48046. PubMed Central, https://doi.org/10.1371/journal.pone.0048046.
Mrówczyński, Włodzimierz. “Health Benefits of Endurance Training: Implications of the Brain-Derived Neurotrophic Factor—A Systematic Review.” Neural Plasticity, vol. 2019, June 2019, p. 5413067. PubMed Central, https://doi.org/10.1155/2019/5413067.
Ostrovskaya, R. U., et al. “Noopept Stimulates the Expression of NGF and BDNF in Rat Hippocampus.” Bulletin of Experimental Biology and Medicine, vol. 146, no. 3, Sept. 2008, pp. 334–37. PubMed, https://doi.org/10.1007/s10517-008-0297-x.
Ozan, Erol, et al. “The Effect of Depression, BDNF Gene Val66met Polymorphism and Gender on Serum BDNF Levels.” Brain Research Bulletin, vol. 81, no. 1, Jan. 2010, pp. 61–65. ScienceDirect, https://doi.org/10.1016/j.brainresbull.2009.06.022.
Phillips, Cristy. “Brain-Derived Neurotrophic Factor, Depression, and Physical Activity: Making the Neuroplastic Connection.” Neural Plasticity, vol. 2017, 2017, p. 7260130. PubMed Central, https://doi.org/10.1155/2017/7260130.
Rendeiro, Catarina, et al. “Dietary Levels of Pure Flavonoids Improve Spatial Memory Performance and Increase Hippocampal Brain-Derived Neurotrophic Factor.” PLoS ONE, vol. 8, no. 5, May 2013, p. e63535. PubMed Central, https://doi.org/10.1371/journal.pone.0063535.
Sandrini, Leonardo, et al. “Association between Obesity and Circulating Brain-Derived Neurotrophic Factor (BDNF) Levels: Systematic Review of Literature and Meta-Analysis.” International Journal of Molecular Sciences, vol. 19, no. 8, Aug. 2018, p. 2281. PubMed Central, https://doi.org/10.3390/ijms19082281.
Thakare, Vishnu N., et al. “Silymarin Ameliorates Experimentally Induced Depressive like Behavior in Rats: Involvement of Hippocampal BDNF Signaling, Inflammatory Cytokines and Oxidative Stress Response.” Physiology & Behavior, vol. 179, Oct. 2017, pp. 401–10. ScienceDirect, https://doi.org/10.1016/j.physbeh.2017.07.010.
Wang, Yu, Hong Liu, Xiang-Dong Du, et al. “Association of Low Serum BDNF with Depression in Patients with Parkinson’s Disease.” Parkinsonism & Related Disorders, vol. 41, Aug. 2017, pp. 73–78. ScienceDirect, https://doi.org/10.1016/j.parkreldis.2017.05.012.
Wang, Yu, Hong Liu, Ben-Shu Zhang, et al. “Low BDNF Is Associated with Cognitive Impairments in Patients with Parkinson’s Disease.” Parkinsonism & Related Disorders, vol. 29, Aug. 2016, pp. 66–71. ScienceDirect, https://doi.org/10.1016/j.parkreldis.2016.05.023.
Xiu, Mei Hong, et al. “Interaction of BDNF and Cytokines in Executive Dysfunction in Patients with Chronic Schizophrenia.” Psychoneuroendocrinology, vol. 108, Oct. 2019, pp. 110–17. ScienceDirect, https://doi.org/10.1016/j.psyneuen.2019.06.006.
Youssef, Mariam M., et al. “Association of BDNF Val66Met Polymorphism and Brain BDNF Levels with Major Depression and Suicide.” International Journal of Neuropsychopharmacology, vol. 21, no. 6, Feb. 2018, pp. 528–38. PubMed Central, https://doi.org/10.1093/ijnp/pyy008.
Zainullina, L. F., et al. “Drug with Neuroprotective Properties Noopept Does Not Stimulate Cell Proliferation.” Bulletin of Experimental Biology and Medicine, vol. 166, no. 4, Feb. 2019, pp. 466–68. PubMed, https://doi.org/10.1007/s10517-019-04373-8.