Key takeaways:
~ Fibrinogen is essential for making blood clots, but high levels of fibrinogen are linked to several health conditions.
~ Fibrinogen levels rise during systemic inflammation, such as during illness, chronic diseases, or mental stress.
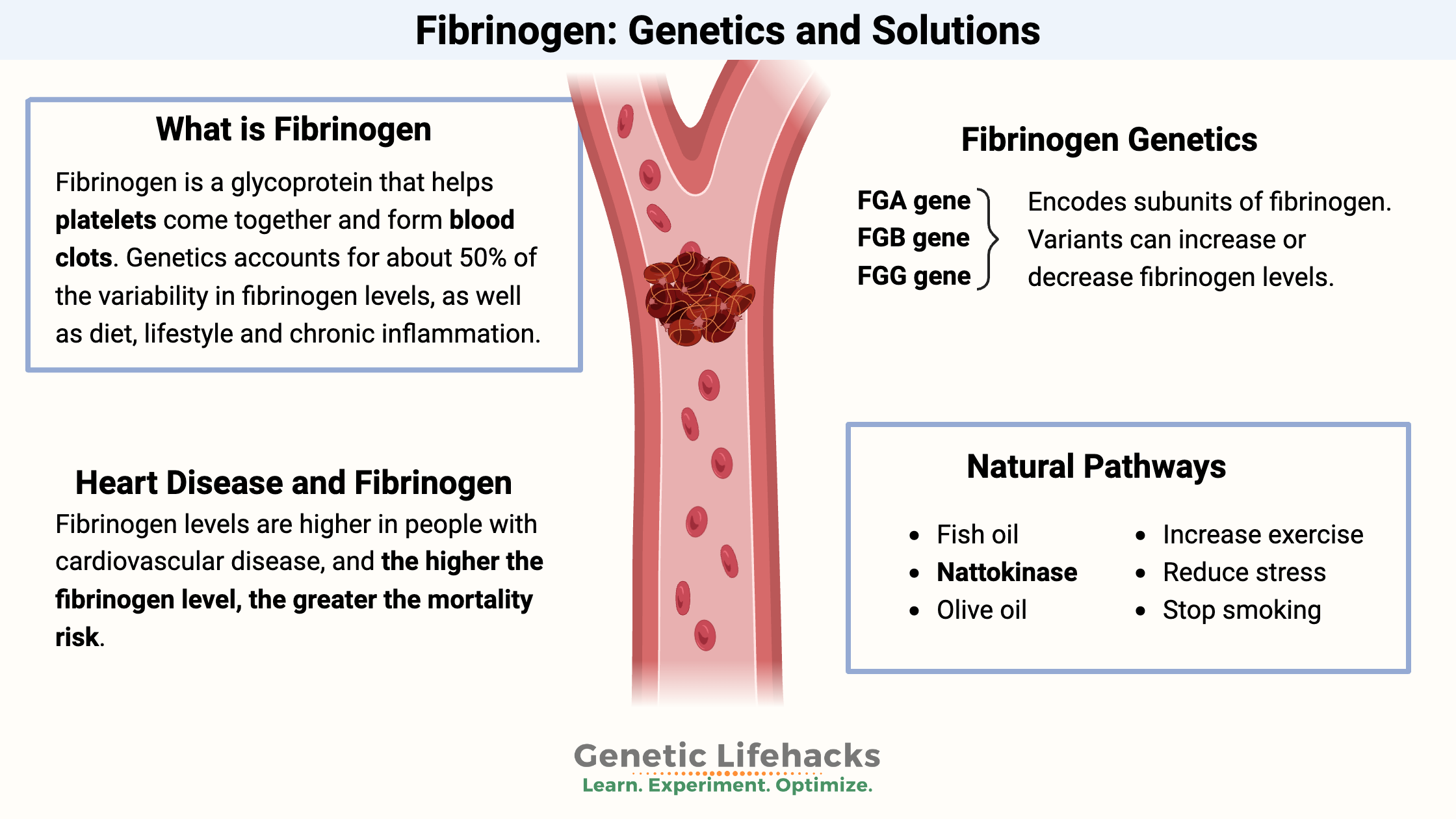
~ Genetics account for about 50% of the variability in fibrinogen levels, with specific genetic variants linked to increased clotting risk.
~ Elevated fibrinogen levels are associated with a higher risk of cardiovascular disease.
Fibrinogen, Heart Health, and Genetics:
- Fibrinogen is a glycoprotein that helps platelets come together and form blood clots. Genetics accounts for about 50% of the variability in fibrinogen levels (the rest is diet, lifestyle, overall health).[ref]
- The liver mainly produces fibrinogen, but the epithelial cells lining the lungs and intestines can also produce fibrinogen. Tumor cells also have been shown to produce fibrinogen.[ref]
- The levels of fibrinogen often rise during systemic inflammation.
Forming a clot from fibrinogen:
For a clot to form, an enzyme called thrombin is needed to convert fibrinogen into fibrin, forming the fibrous part of a blood clot.
The fibrin strand crosslinks with each other using factor XIIIa, forming a clumped network of fibrin.
A blood clot doesn’t just form and sit there forever (obviously). Instead, it is a dynamic event with the clot-forming and breaking down all the time. Plasmin, an enzyme that breaks down clots, and fibrin activate the formation of plasmin. When plasmin breaks down some of the fibrin, the d-dimer is released. (D-dimer levels are often tested in hospitals to see if there has been a clot.)
Inflammation and Fibrinogen
- In addition to its role in clotting, fibrinogen is activated by acute inflammation (whether from a wound or other sources).[ref]
- Fibrinogen production in the liver immediately increases in acute inflammatory situations.
- Additionally, fibrinogen causes macrophages to produce inflammatory cytokines.[ref]
Thus, fibrinogen is created in response to inflammation and can also cause an increase in inflammation under certain conditions.
Fibrinogen in Heart Disease
One of the key players in cardiovascular disease (CVD) is plasma fibrinogen. It is a main component of clots in the arteries.
In general, fibrinogen levels are higher in people with cardiovascular disease, and the higher the fibrinogen level, the greater the mortality risk.[ref]
Cardiovascular disease ‘endpoints’ in research are defined as stroke, heart failure, coronary heart disease, and peripheral artery disease. Some cardiovascular disease researchers believe that fibrinogen levels reflect the increased inflammation that accompanies heart disease. Thus, the increased inflammation causes high fibrinogen, which adds to atherosclerosis (plaque in the arteries).[ref]
Genetic variants that increase fibrinogen increase the risk of heart disease. But lifestyle factors play a significant role here — smoking, diet, lack of exercise all increase inflammation and thus raise fibrinogen levels. For example, cigarette smoking increases fibrinogen by over 10%.[ref]
The use of Mendelian randomization studies tries to determine whether something causes a disease (e.g., does higher fibrinogen cause cardiovascular disease vs. does CVD cause higher fibrinogen). A Mendelian randomization study on fibrinogen-related genes found that fibrinogen does have a small causal role in CVD.[ref] Again – this points to genetics + lifestyle factors.
Coagulation in COVID-19
Doctors and researchers have found that people with severe COVID-19 are likely to have hypercoagulation – too much clotting going on relative to the breaking down of clots.[ref]
- Patients with prothrombin time >3s were at a 4-fold risk of having a ‘thrombotic event’, including stroke, heart attack, deep vein thrombosis, or pulmonary embolism.[ref]
- Another study found elevated D-dimer levels and increased prothrombin time were predictive of mortality in COVID-19 patients in the hospital.[ref]
- A July 2020 study showed increased fibrinogen levels and ‘dramatically increased’ D-dimer levels in COVID-19 patients. CRP, Factor VIII, and von Willebrand factor – all involved in clotting – were also increased.[ref]
There are several theories as to what is going on with abnormal coagulation in COVID-19:
- First, plasmin (the enzyme that breaks down clots) activates whenever fibrinogen is activated to make a clot. Plasmin can also enhance the pathogenicity of certain viruses – and researchers think this is possible with the SARS-CoV-2 virus.[ref]
- Second, severe COVID-19 patients have increased pro-inflammatory cytokine levels. These inflammatory cytokines then tip the balance towards too much coagulation and not enough anticoagulation.[ref] Most patients now are started on anti-coagulants when in the hospital for COVID-19.[ref]
A new study (Aug. 2024) now shows that fibrin binds to the SARS-CoV-2 spike protein. This drives proinflammatory clotting and also causes neuroinflammation.[ref]
Fibrinogen levels in cancer
Fibrinogen levels show an elevation in certain types of cancer. Higher fibrinogen levels in lung cancers, such as NSCLC and mesothelioma, are predictive of outcome.[ref][ref] A study of women with uterine leiomyosarcoma, a rare uterine cancer, showed that patients with higher fibrinogen levels had a much lower survival rate.[ref]
Additionally, there may be a small causal role here. People with higher fibrinogen levels are also at a higher risk of lung cancer. Researchers think this is because increased coagulation could be a cause of lung cancer.[ref]
Stress and Fibrinogen:
Both mental stress and cellular stress can increase fibrinogen levels. Acute and chronic mental stress can increase inflammation levels throughout the body, resulting in higher fibrinogen levels.[ref]
Three proteins in fibrinogen: alpha, beta, and gamma
The fibrinogen molecule is composed of three different amino acid chains – α, β, and γ.[ref] These components come together to form the fibrinogen molecule circulating in the bloodstream, and when a coagulation event occurs, they break up to form the fibrin.
There are three genes that code for the three components of fibrinogen – FBA, FGB, and FGG. All three of these genes have genetic variants affecting fibrinogen levels in different ways, which you can see below in the genotype report.
Fibrinogen Genotype Report
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Lifehacks:
Fibrinogen is something you need at the right levels in your body — too much can increase the risk of blood clots, and too little could increase the risk of bleeding. Talk with your doctor if you have concerns about clotting. You can also test fibrinogen with a blood test, which you can order through your doctor or order on your own.
If you are on any medications, especially heart-related medications, talk with your doctor before adding any supplements.