Key takeaways:
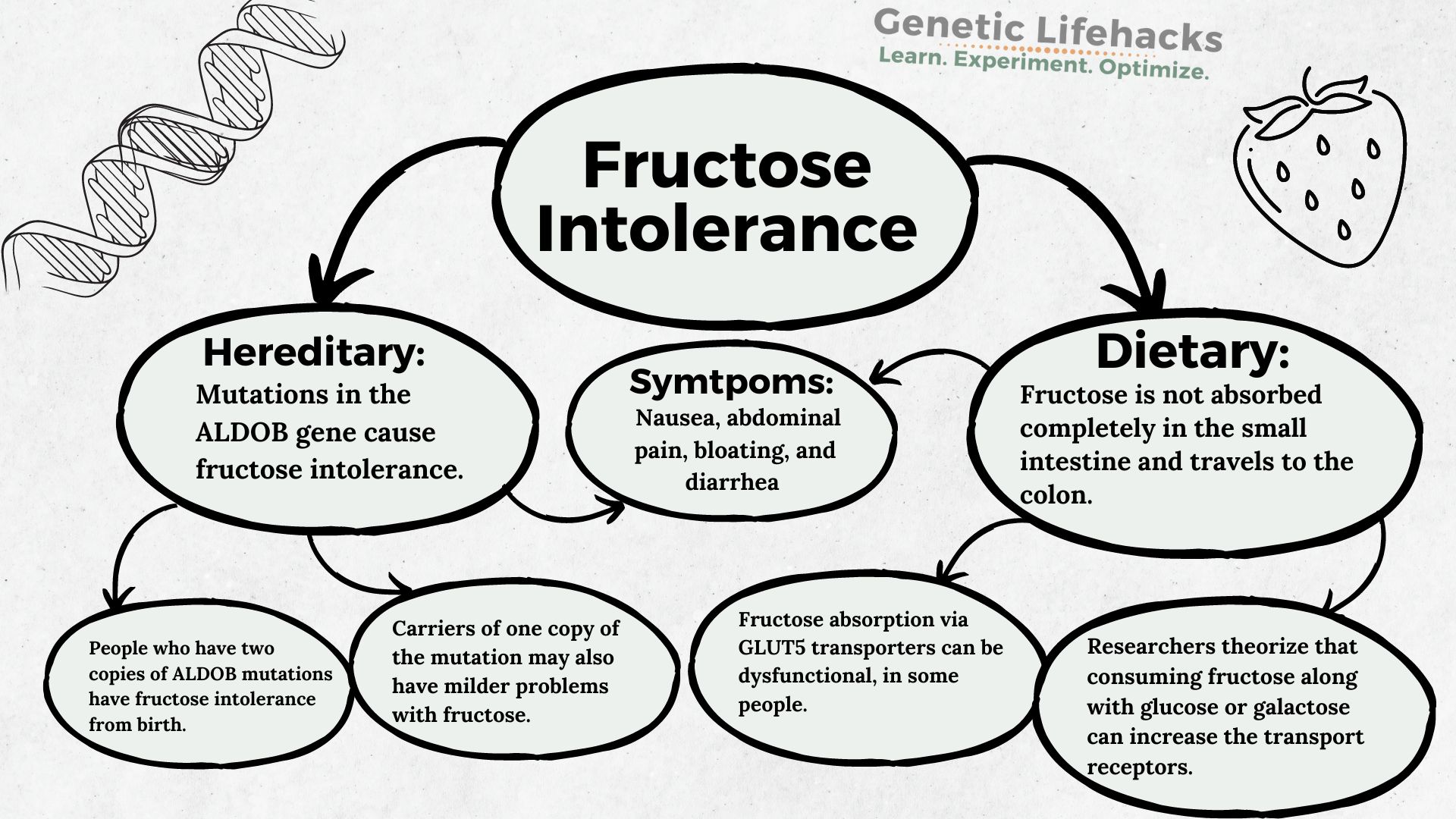
~ Fructose intolerance can be hereditary (genetic) or dietary (due to intestinal absorption problems).
~ Rare genetic mutations in the ALDOB gene cause hereditary fructose intolerance.
~ Carriers of a single ALDOB mutation (more common) can still process some fructose, but they may be prone to insulin resistance with higher fructose consumption.
Members see their genotype report below, plus solutions in the Lifehacks section. Consider joining today.
What is fructose intolerance? Symptoms and Causes
Fructose intolerance causes digestive symptoms, such as nausea, diarrhea, bloating, gas, and abdominal pain, after eating foods that contain fructose.
Fructose is a sugar found in fruits and vegetables. People with fructose intolerance may need to avoid many fruits, juices, honey, table sugar, peas, zucchini, asparagus, maple syrup, sorghum, molasses, agave, palm sugar, coconut sugar, and corn syrup.
According to the Mayo Clinic, some fruits with low fructose content, such as blueberries, bananas, avocados, strawberries, and carrots, may be okay in limited amounts with meals. Sorbitol should also be avoided.[ref]
How is fructose absorbed in the small intestine?
While fructose and glucose are similar sugars in many ways, their absorption in the gut is a little bit different.
- Glucose is completely absorbed in the small intestine and is facilitated by GLUT2 and GLUT5 transporters. Glucose can also be absorbed without the transporters.
- Fructose is absorbed in the small intestine through carrier-mediated facilitative diffusion and by the GLUT5 transporter. Without adequate GLUT5 transporters, fructose may not be completely absorbed and thus ends up in the colon.
Dietary vs. Hereditary fructose intolerance:
Fructose intolerance can be classified as either hereditary or dietary fructose intolerance.
- Hereditary fructose intolerance is caused by rare mutations in the ALDOB gene and is present from birth.
- Dietary fructose intolerance shares some of the symptoms of hereditary fructose intolerance, but the disorder is caused by decreased fructose absorption in the small intestine.
Let’s start with hereditary fructose intolerance…
What happens in hereditary fructose intolerance?
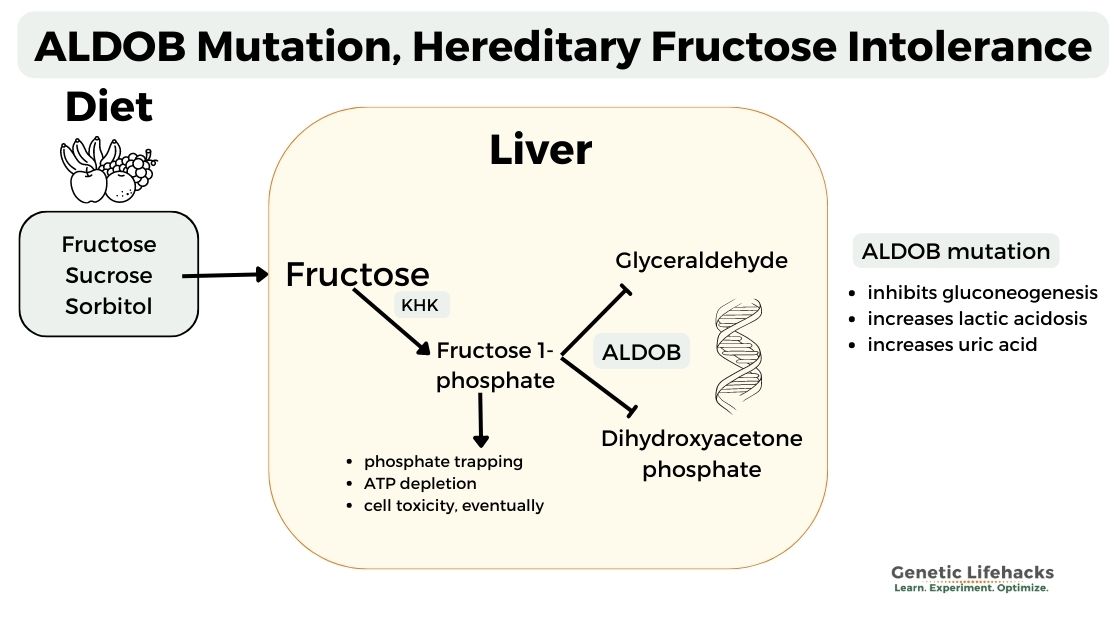
In hereditary fructose intolerance, two copies of mutations in the aldolase B (ALDOB) gene cause the enzyme not to function.
The aldolase B enzyme breaks down fructose-1-phosphate into glyceraldehyde and dihydroxyacetone phosphate in the liver.[ref]
The inability to break down fructose 1-phosphate causes phosphate trapping and ATP depletion in the liver. Additionally, it inhibits glycolysis and gluconeogenesis, leading to hypoglycemia or even lactic acidosis. The buildup of phosphate also causes uric acid to rise.
Symptoms of hereditary fructose intolerance include nausea, bloating abdominal pain, diarrhea, vomiting, and hypoglycemia.[ref]
In hereditary fructose intolerance, liver and kidney dysfunction will eventually occur if fructose continues to be consumed.[ref]
Hereditary fructose intolerance is rare and found in 1 in 10,000 people.[ref]
It is usually diagnosed in infants when they are introduced to fructose-containing foods.
However, it is estimated that around 1 in 80 people carry a single copy of an ALDOB mutation, which may cause issues with consuming larger amounts of fructose in one sitting.[ref]
Can hereditary fructose intolerance be diagnosed in adulthood?
Very rarely, hereditary fructose intolerance is discovered later in life. A case study showed that a 41-year-old woman who reported sweating, nausea, and vomiting after consuming sweets actually carried two mutations in the ALDOB gene. She had avoided eating sweets since infancy. This instinctive avoidance of foods containing fructose meant that she had no negative effects, with normal laboratory findings. [ref]
What happens if you have one copy of a hereditary fructose intolerance mutation?
Carrying one copy of an ALDOB mutation decreases the enzyme efficiency to about 50%. This is usually enough of the functional enzyme to digest moderate amounts of fructose.
A study of people carrying one ALDOB mutation showed that eating a meal high in fructose causes increased fasting uric acid, reduced fasting insulin sensitivity, and increased insulin resistance.[ref]
Thus, while mutation carriers likely will not have acute symptoms of hereditary fructose intolerance, limiting the amount of fructose consumed may help with metabolic health.
Dietary fructose intolerance or fructose malabsorption:
Dietary fructose intolerance causes bloating, abdominal pain, and diarrhea due to fructose not being absorbed in the small intestine and traveling through to the large intestine. It can be misdiagnosed as IBS. [ref]
Fructose is transported across the epithelial cells in the intestines by the GLUT-5 or GLUT-2 transporters, which also transport glucose and galactose.
Researchers theorize that consuming fructose along with glucose or galactose can upregulate the GLUT receptors and decrease problems with fructose malabsorption. Excess fructose consumption at one time can overwhelm the transport system in the small intestines.[ref]
When fructose isn’t completely absorbed in the small intestine, it ends up in the colon where it gets fermented by bacteria, causing bloating, gas, and loose stools.[ref]
Tests for fructose malabsorption and intolerance use a breath test to determine the amount of hydrogen being produced by the gut bacteria. [ref]
There have been no human gene variants identified that relate to fructose malabsorption.
Studies in mice show that a protein, ChREBP, that regulates the number of GLUT-5 transporters plays a role in causing dietary fructose intolerance.[ref] This indicates that dietary fructose intolerance is likely due to decreased GLUT-5 transporters, with one cause being the genetic or epigenetic regulation of the transporter.
The ChREBP is encoded by the MLXIPL gene. While there aren’t any studies directly associating MLXIPL variants with fructose intolerance, there is indirect evidence of an association. High fructose corn syrup often causes elevated triglycerides.[ref] Certain MLXIPL SNPs are linked to lower triglyceride levels, which ties into decreased absorption of fructose. [ref] (The MLXIPL variant is included in the triglycerides genotype report.)
Fructose Intolerance Genotype Report
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Lifehacks for Fructose Intolerance
Keep in mind that sucrose – table sugar – is a combination of fructose and glucose. Honey is also high in fructose.
Reduce fructose with hereditary fructose intolerance mutation:
For carriers of one copy of an ALDOB mutation, reducing the amount of fructose overall and avoiding large amounts at one time may help with liver health and intestinal problems. Carriers of one copy of the mutation may have insulin resistance and poor metabolic health if they eat a diet high in fructose.
Supplements that may help with fructose intolerance:
Related articles and topics:
Histamine intolerance:
Many healthy foods also contain histamine, which may cause problems for people with certain genetic variants.
Lactose intolerance: check your genes
You can easily see whether you genetically produce lactase as an adult.