Key takeaways:
~ The WHO lists light at night as a possible carcinogen.
~ Melatonin, which helps prevent cancer, is suppressed by light at night.
~ Circadian rhythm is altered by exposure to light at night.
~ Genetic variants can make people more susceptible to the harms of circadian disruption.
~ Simple solutions can help prevent circadian disruption.
Members will see their genotype report below, plus additional solutions in the Lifehacks section. Consider joining today.
Light at night and cancer
The World Health Organization listed ‘light at night’ as a possible carcinogen in 2007. Let’s let that sink in for a minute… On the same list of possible carcinogens that includes formaldehyde, aflatoxin, and the HPV virus is something as innocent as artificial light at night.[ref]
From streetlights and outdoor accent lights to the glow of TVs, lamps, and cell phones… artificial light at night is ubiquitous.
How can light increase the risk of cancer? Will turning on the TV or an overhead light after dinner suddenly cause you to sprout a tumor?
Let me give you the background science on the biological pathway through which light at night impacts cancer risk. Then I’ll cover the epidemiological evidence and genetic connections.
Finally, I’ll wrap up by putting the risk into perspective, because – no, turning on the TV for one night after dinner will not cause you to sprout tumors. Instead, this is a more complex picture involving a fundamental change to our society with the invention of electric lights.
Melatonin and cancer prevention:
Melatonin, which most people think of as ‘the sleep hormone’, rises at night and falls during the daytime. Maintained in almost all animals, this is a circadian rhythm governed by the light hitting the retina of the eye.
Melatonin, though, is not just a sleep hormone. In addition to circadian signaling, recent research shows that melatonin acts as an antioxidant within cells, helping to combat oxidative stress in our cells at night. While we sleep, our cells go into rest and repair mode, cleaning up the waste from the active period during the day. When cells are exposed to too much oxidative stress, it can lead to DNA damage.
There are two factors governing melatonin production overnight:
- Exposure to light during the day – and –
- Absence of light at night.
First, let’s look at light exposure during the day:
Melatonin levels are affected by the amount of light (specifically in the blue wavelengths) that you get during the daytime. An animal study showed that increasing blue wavelengths (465-485) during the day caused a 7-fold increase in nighttime melatonin levels compared to animals kept under standard fluorescent lighting. The animals exposed to blue-enriched light during the day also had markedly reduced tumor growth. The increased melatonin production leads to a decrease in the Warburg Effect, which is the shift to glycolytic metabolisms that cancer cells exhibit.[ref]
Other studies have shown similar results – increased melatonin causing decreased tumors (prostate, oral, breast).[ref][ref][ref]
The second factor impacting overnight melatonin production is exposure to light at night:
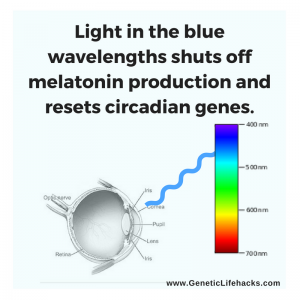 The rise in melatonin at night is governed by the decreasing amount of blue light hitting our eyes in the evening hours. Researchers refer to this rise in melatonin in the evening as ‘dim light melatonin onset’.
The rise in melatonin at night is governed by the decreasing amount of blue light hitting our eyes in the evening hours. Researchers refer to this rise in melatonin in the evening as ‘dim light melatonin onset’.
While suppressing melatonin with lots of blue light during the day is good, the opposite needs to occur after the sun sets. At night, we need melatonin levels to rise as much as possible.
Studies over the last twenty-plus years have made it clear that light at night (dim or bright) causes a decrease in melatonin levels.
Animal studies clearly show decreased melatonin levels increase the risk of certain types of cancer:
- breast cancers[ref][ref]
- tumors and the warburg effect [ref]
- prostate cancers[ref]
- glioblastomas[ref]
- metastasis[ref]
Stress hormones also play a role:
In addition to affecting melatonin levels, light at night also increases cancer risk through the activation of stress hormones.[ref]
The connection between an increased risk for hormonal cancers and salivary cortisol levels has been well established, and disruption to the normal circadian rhythm of cortisol is linked to doubling the risk of death in breast cancer.[ref]
So there is a bit of a double whammy here: light at night decreases melatonin (a cancer preventative) and increases stress hormone levels (cancer-causing).
What do epidemiological studies show about cancer and light at night?
Epidemiological studies on cancer risk are often based on correlating environmental factors with an increase in risk. In most studies, researchers do their best to account for risk factors such as socioeconomics, exposure to pollutants, and ethnicity.
Let me start with two recent – and contradictory – studies on exposure to artificial light at night.
The first example is an Israeli study that investigated breast cancer incidences in relation to light at night in a unique way. The study used spectral imaging – a satellite mapping method looking at the color spectrum of light – to investigate a link between the wavelengths of light at night and breast cancer. When looking at artificial light from a streetlight, the color of the light can change from the yellow glow of sodium-vapor light to the blue-white of LED lights. The researchers theorized that the light spectrum would matter based on animal studies showing light in the shorter wavelengths (blue light) increased breast cancer incidence. Additionally, the researchers factored in differences in socio-economics, age, ethnicity, and other environmental factors which could increase the risk of breast cancer. The results showed light at night increased breast cancer risk, but only in areas of the country with more light in the blue wavelengths at night.[ref]
Similar studies back up the findings that increasing light exposure increases the risk of breast cancer.[ref]
Not all studies agree that light at night impacts cancer risk, of course. But when looking at epidemiological studies, you really need to examine whether the methods make sense. Take for example a study published in the British Journal of Cancer showing exposure to light at age 20 didn’t increase the risk of breast cancer. To come to this conclusion, researchers asked women who were currently in their mid-40’s to report on how much light they were exposed to at night when they were 20. (Do you remember where all you lived in your 20s and how much light crept around the curtains at night?)[ref]
A more recent study also found that light at night (satellite imagery) is not linked to liver cancer.[ref] However, the same study group participants did have an increase in pancreatic cancer associated with more artificial light at night.[ref]
Studying light exposure at night is difficult, which makes it hard to prove causation for cancer. The majority of the world is exposed to more and more light at night, and measuring the impact of that exposure over years or decades is imprecise, to say the least.
One group of people exposed to bright light all night long, though, is night shift workers.
Night shift workers have an increased risk of breast cancer.
Evidence from studying shift workers (mainly nurses) showed varying results for the increased risk of breast cancer.
- One large study found a 79% increase in breast cancer risk for women working the night shift for 20 years.[ref]
- Another study looking at the combined data from the Nurses Health Studies found that for women exposed at younger ages to night shift work (light at night) there was a more than doubled risk of breast cancer.[ref]
- Not all studies show such a large risk, with one study estimating only a 7 – 21% increase in risk.[ref]
- A meta-analysis combining data from 28 studies found the increase in relative risk from night shift work to be 19%.[ref]
Dim light at night and cancer:
What about the risk from general light at night (street lights, lights at home)?
It turns out that you don’t have to work the night shift to have an increased risk of cancer due to light at night. A California study of over 100,000 women found a 34% increased risk of breast cancer for premenopausal women exposed to higher amounts of light at night.[ref]
There are quite a few smaller studies on breast cancer and light at night with similar findings to the larger ones – with a few interesting tidbits thrown in.
- One study found a 51% increased risk with higher ambient light at night.[ref] It also found that sleeping longer (thus more melatonin) cut the risk of breast cancer in half.
- Closing the shutters at night (shutting out the streetlights) was also associated with a significant decrease in cancer risk.[ref]
Why does a dim light at night matter?
You may wonder why dim light matters when you have your eyes shut at night. Light in the blue wavelengths passes through your eyelids fairly well.
A study from a few years ago tested a light device to see if they could shift melatonin levels while the participants were asleep. The researchers used sleep masks with different colored led lights built into them; the lights turned on for two seconds every minute for an hour — while the study participants slept! The results showed that exposure to blue wavelengths through their closed eyelids affected melatonin. It significantly shifted the time that melatonin onset began the following night.[ref]
How much light is too much?
The answer may surprise you… Even 0.2 lux (way less than a nightlight) was found to affect cancer rates in rats.[ref]
People may not be as sensitive as rats, and most studies on dim light at night use 5 lux as a test amount. This is similar to the amount of light from a night light in the hall near your bedroom.
How bright is a ‘lux’? On a sunny day, the outdoor illuminance can be as high as 120,000 lux, and on a cloudy day, it is about 1,000 lux. Contrast this with a moon-lit night which ranges from 0.002 lux to 0.25 lux (quarter moon vs full moon).
Using genetics to determine causality:
One way researchers determine if a correlation found in an epidemiological study is causal is to determine if there is a mechanism of causation, such as with melatonin and cancer risk. Another way to determine causation is to see if genetic variants that impact the system are linked to an increase in risk. In this case, we would be looking at whether genetic variants in the circadian-rhythm-related genes are linked to cancer risk.
First, a quick overview of the key genetic players in the circadian clock, and then we’ll look at several examples of how circadian-related genetic variants increase cancer risk.
The core circadian clock is driven by a transcription-translation feedback loop with two central proteins (CLOCK and BMAL1 genes) rising and then inhibiting the creation of two other pairs of proteins (CRY and PER family of genes).
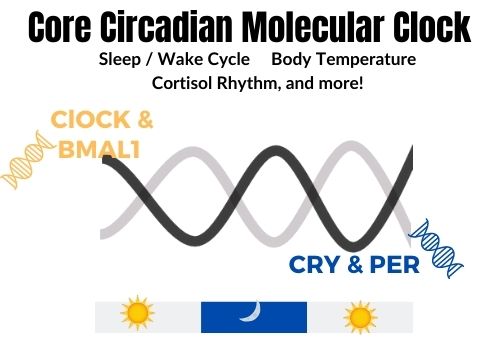
In addition to these core circadian genes, it is likely that genetic variants impacting melatonin should also alter cancer risk.
Genotype Report: Circadian Rhythm and Cancer
Members: Log in to see your data below.
Not a member? Join now.
BMAL1: core circadian clock gene The BMAL1 protein is coded for by the ARNTL gene.
Check your genetic data for rs969485 (23andMe v4, v5;; AncestryDNA):
- G/G: increased risk of breast cancer with night shift work[ref]
- A/G: increased risk of breast cancer with night shift work (64%)
- A/A: typical
Members: Your genotype for rs969485 is –.
Check your genetic data for rs2278749 (23andMe v4, v5; AncestryDNA):
- T/T: night shift work less likely to increase breast cancer risk[ref] more fertile[ref]
- C/T: night shift work less likely to increase breast cancer risk[ref]
- C/C: typical
Members: Your genotype for rs2278749 is –.
CRY2 gene: encodes a core circadian clock gene (negative arm of the clock)
Check your genetic data for rs7123390 (23andMe v4; AncestryDNA):
- A/A: over 50% decreased risk of estrogen and progesterone receptor-negative breast cancer[ref]
- A/G: decreased risk of ER estrogen and progesterone receptor-negative breast cancer
- G/G: typical
Members: Your genotype for rs7123390 is –.
MTNR1A gene: This gene codes for the MT1 melatonin receptor.
Check your genetic data for rs2375801 (23andMe v4)
- C/C: increased risk of cancer metastasis (liver)[ref]
- C/T: increased risk of cancer metastasis (liver)
- T/T: typical
Members: Your genotype for rs2375801 is —.
Check your genetic data for rs6553010 (23andMe v4, AncestryDNA):
- A/A: increased risk of cancer metastasis (liver)[ref]
- A/G: increased risk of cancer metastasis (liver)
- G/G: typical
Members: Your genotype for rs6553010 is –.
These genetic variants are just given as examples to strengthen the evidence that light at night increases the risk of cancer by suppressing melatonin and disrupting the circadian clock. There are numerous other circadian gene variants also linked to either increasing or decreasing the risk for certain cancers, so you would need a bigger picture – a polygenic risk score – to understand your true risk.[ref][ref][ref]
Quantifying the risk:
So after all of the studies (and there are hundreds more than are referenced here), what is the consensus for the cancer risk from light at night? Both the World Health Organization and the American Medical Association place light at night as a probable carcinogen.
One problem with quantifying the impact of artificial light at night is that there are few places left that are unaffected. To get around this problem, one study investigated protected or natural areas, such as forests and conservation areas, in 158 different countries and compared cancer incidences to areas with higher artificial light at night. The study showed, when all confounders were taken into account, that colorectal, prostate, and breast cancer relative risk increased by up to 35% with light at night.[ref]
Other studies show a range of increased relative risk – from 35% to 79% to 200%.
Keep in mind this is relative risk, not absolute risk.
To conceptualize the risk, let’s take breast cancer as an example. First, we need to know some statistics for breast cancer prevalence.
The lifetime risk in the US of breast cancer for women is 1 in 8, with the risk increasing with age.[ref] Thus, a 35% increase is going to change that risk to about 1 in 6, while a 2-fold increase would increase the lifetime risk to 1 in 4.
Let’s put this into perspective against other known breast cancer carcinogens:
- According to some studies, hormone replacement therapy increases the relative risk of breast cancer by 75% (~1 in 5)[ref]
- BRCA gene mutations can increase the absolute risk of breast cancer to about 1 in 2.[ref]
This puts light at night in the “not as risky as carrying the BRCA mutations” category, but possibly similar to hormone replacement therapy.
Mendelian Randomization Studies:
Correlation doesn’t always mean causation. Using known genetic connections as well as large data models, researchers can use a technique called a Mendelian randomization study to determine causation.
Mendelian randomization studies have been used to determine that being a morning person instead of a night owl is causally linked to a (slightly) decreased risk of digestive tract cancers, stomach cancer, and colorectal cancer.[ref] A morning chronotype usually means that a person is exposed to less light at night because they are asleep.
Lifehacks for preventing the increased cancer risk:
The rest of this article is for Genetic Lifehacks members only. Consider joining today to see the rest of this article.
Related Genes and Topics:
Using your genetic data to solve sleep problems
A good night’s sleep is invaluable – priceless, even – but so many people know the frustration of not being able to regularly sleep well. Not getting enough quality sleep can lead to many chronic diseases such as diabetes, obesity, dementia, and heart disease. Yes, sleep really is that important!
Circadian Rhythms: Genes at the Core of Our Internal Clocks
Circadian rhythms are the natural biological rhythms that shape our biology. Most people know about the master clock in our brain that keeps us on a wake-sleep cycle over 24 hours. This is driven by our master ‘clock’ genes.