Key takeaways:
~ Many sleep disorders, including insomnia and restless leg syndrome, have a strong genetic component. Specific gene variants can affect sleep quality, timing, and duration.
~ Deep sleep and REM sleep are essential for memory, emotional regulation, and physical health. Sleep deprivation is linked to impaired cognition, cardiovascular problems, and obesity.
~ Adenosine builds up during the day to induce sleep pressure, while neuropeptide S and neurotransmitters like GABA and serotonin influence sleep stages and quality.
~ Exposure to blue light at night disrupts melatonin production and circadian rhythms. Reducing light exposure in the evening can improve sleep.
What is sleep, and why do we need it?
“Why do we sleep?” turns out to be a more difficult question to answer than you would think.
We are asleep for about a third of our lives. All animals, both big and small, sleep. So you would think that scientists would know exactly why and how sleep works… Instead, we have almost as many questions about sleep as we have answers.
Let’s look at the definition of sleep from a prominent sleep medicine textbook: “Sleep is a recurring, reversible neuro-behavioral state of relative perceptual disengagement from and unresponsiveness to the environment. Sleep is typically accompanied (in humans) by postural recumbence, behavioral quiescence, and closed eyes.”[ref] Yep – big words for laying down, closing your eyes, and going to sleep.
The important thing here, though, is what goes on in the brain while you sleep. While your body is inactive (hopefully), your brain is doing some pretty cool and weird stuff while you sleep. Plus, there are different metabolic processes going on in your body while you are asleep compared to when you’re awake.
Why is sleep so important?
While you sleep, your brain consolidates memories — it makes the things that you learned during the day stick in your brain. This has been known for a long time and is something that researchers frequently experiment with.[ref]
Recently, researchers experimented with just decreasing certain stages of sleep and showed that the neuroplastic changes to the brain in learning happen specifically during deep sleep.[ref]
Another role of sleep is to reduce oxidative stress in the gut. A couple of studies in animals show that the lack of sleep causes death due to oxidative stress in the intestines.[ref]
Studies of sleep deprivation show there can be devastating consequences.
- For most people, sleep deprivation causes a decrease in speed and accuracy in tests for attention, working memory, processing speed, short-term memory, and reasoning.[ref]
- One-third of accidents in a survey of commercial truck drivers were caused by drowsy driving due to sleep deprivation.[ref]
- According to the NTSB, going 20+ hours without sleep is equivalent to driving legally drunk. And your risk of being in a car crash goes up 3-fold![ref]
- This pretty much sums up the rest of the effects of sleep deprivation: ‘studies have shown that short sleep duration is associated with an increased incidence of cardiovascular diseases, such as coronary artery disease, hypertension, arrhythmias, diabetes, and obesity, after adjustment for socioeconomic and demographic risk factors and comorbidities.'[ref]
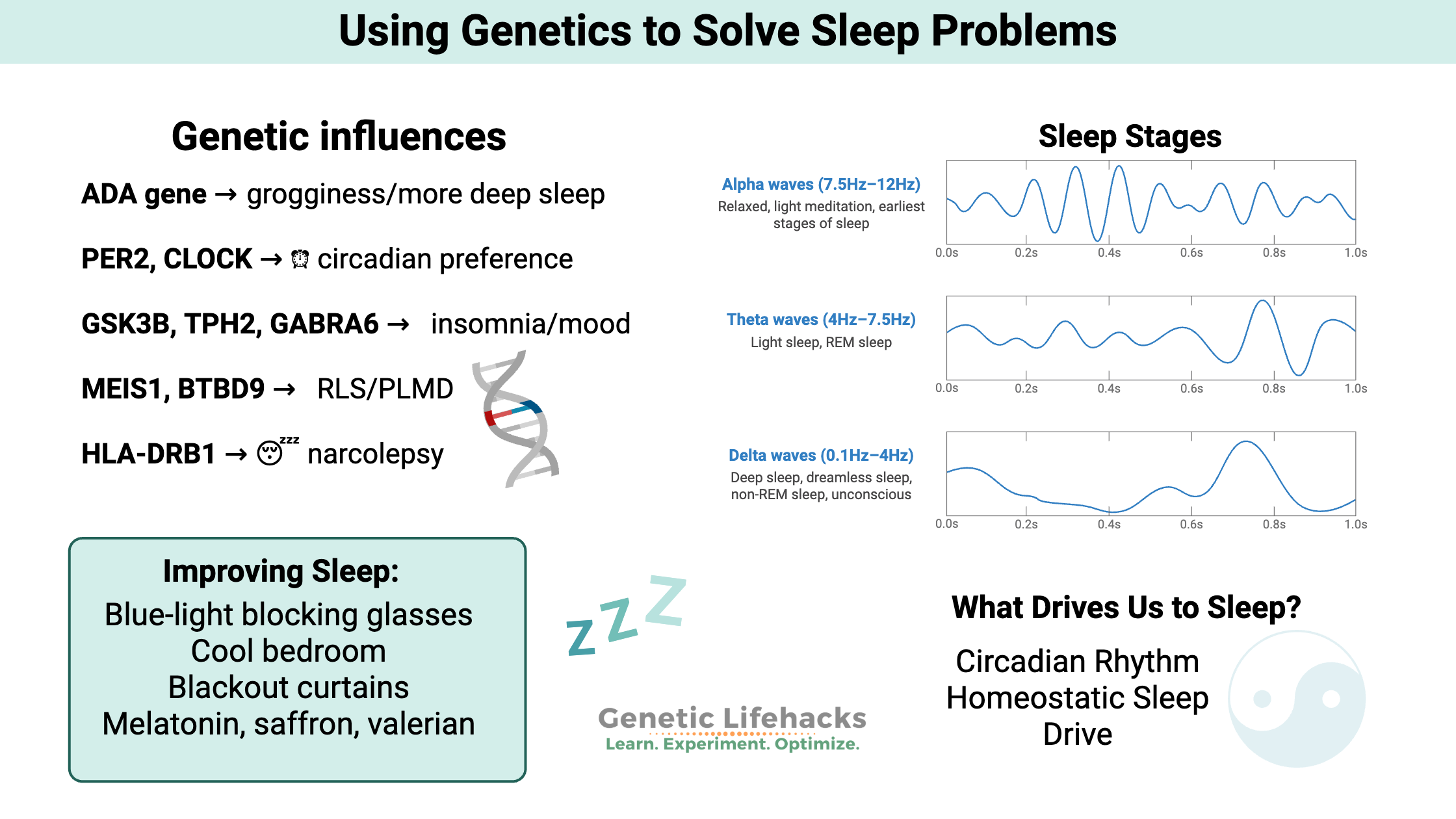
Stages of sleep:
When you sleep, your brain goes through different periods of activity. These are categorized into slow-wave sleep and REM (rapid eye movement) sleep.
Slow-wave sleep can further be broken down into deep sleep and light sleep. About 50% of sleep time (in adults) is light, non-REM sleep.
Most of your deep sleep comes during the early part of the night, while the latter half of the night has much more REM sleep.[ref]
Brain waves during sleep:
Your brain waves slow down during sleep, becoming more synchronized with lower frequency and higher amplitude.
- Light sleep and REM sleep = theta waves
- Deep sleep = delta waves
During non-REM sleep, the brain is consolidating memories, which is important in learning and recall. During REM sleep, emotions are being recorded and modulated within the hippocampus.[ref]
Different types of neurons are firing or silenced during the sleep stages. During NREM sleep, serotonergic and noradrenergic neurons decrease their firing rate, and they become nearly inactive during REM sleep. Acetylcholine levels in the brain are at their low point during NREM sleep, but levels rise considerably during REM sleep.
Sleep Disorders and Genes:
Let’s take a look at some of the ways that sleep can be disrupted or disturbed – along with the genetic connections that are included in the Genotype report section below.
| Disorder | Prevalence | Key Genetic Contributors | Notable Features |
|---|---|---|---|
| Insomnia | 10% adults, 22% elderly | GSK3B, PER2, TPH2, GABRA6 | Difficulty falling/staying asleep |
| Restless Leg Syndrome | ~10% US population | MEIS1, BTBD9, MAP2K5, PTPRD | Urge to move legs, sleep disruption |
| Narcolepsy | 1 in 2,000 | HLA-DRB11501, HLA-DQB10602 | Excessive daytime sleepiness |
| Circadian Rhythm Disorders | Variable | CLOCK, PER2, AANAT | Disrupted sleep timing |
Difficulties with sleep drive and circadian rhythm:
We feel the need to sleep each night due to two causes:
- changing levels of our circadian rhythm genes
– and – - increased homeostatic sleep drive
Feeling sleepy:
The homeostatic sleep drive is what researchers call the build-up over the course of the day for the need to sleep. This is mainly driven by a build-up of adenosine in the brain, which is then cleared out during sleep.
Adenosine is part of the ATP (adenosine triphosphate) molecule used for cellular energy. The ATP molecule stores energy in its bonds and releases energy as the bonds with phosphate are broken. As you use energy over the course of the day, you build up adenosine in the brain.[ref] Interestingly, caffeine makes you feel more awake by blocking the adenosine receptors, thus making your brain think that not as much adenosine has built up.
Not clearing out adenosine quickly enough overnight can cause a person to still feel groggy when they wake up in the morning. A variant of the ADA (adenosine deaminase) gene is associated with reduced activity, causing adenosine to be cleared away less quickly. Variants in the ADA gene are linked with more deep sleep, but the slower clearance of adenosine means that a short night’s sleep leaves the person feeling groggier than normal.
Neuropeptide S is a neuropeptide found mainly in the amygdala. Animal studies show that when neuropeptide S binds to its receptor, it induces wakefulness. At night, neuropeptide S reduces NREM sleep.[ref]
A gut peptide, CCHa1, was discovered a couple of years ago to be involved in sleep. Higher levels of CCHa1 make it harder to be aroused from sleep. Interestingly, for animals, higher amounts of protein in the diet increase the sleep-promoting peptide at night.[ref]
Circadian rhythm:
The body’s circadian rhythm is the 24-hour built-in molecular clock. Many different processes in the body occur at different times of the day based on the circadian clock. For example, the enzymes that you produce to break down food are driven by the timing of your normal eating patterns. You may notice that eating dinner several hours later than normal doesn’t always digest as well.
We (all of us humans) are diurnal, which means our circadian rhythm is set up for being up and active during the day and sleeping or inactive in the dark.
Yep, we are flexible, and people can change over to work the night shift. But that change can come with health consequences, more for some than others.
The genes that control the core circadian rhythm can affect sleep quality as well as mood and cognitive function.
Related article: Circadian rhythm genes and mood disorders
What causes insomnia?
Everyone, at some point, knows the pain of a sleepless night. For some, though, this is an all too frequent occurrence. About 10% of adults and 22% of the elderly are estimated to have an insomnia disorder.[ref]
Insomnia can be either a problem with initially falling asleep or with waking up in the early morning hours and not being able to fall back to sleep. There are several terms applied to different types of insomnia:
- Sleep onset insomnia – problems with falling asleep
- Early waking (terminal insomnia) – waking up too early and not falling back to sleep
- Sleep maintenance insomnia – waking up one or more times in the night and struggling to get back to sleep
Genetics and insomnia:
Heritability estimates from twin studies show that insomnia is around 50% genetic; genes lend susceptibility along with environmental factors. The biggest genetic influence is for sleep maintenance insomnia, where people have a hard time staying asleep rather than difficulty falling asleep. [ref][ref]
Problems sleeping go hand-in-hand with depression. 80-90% of people with major depression experience insomnia of some sort, with about half of them experiencing severe insomnia.[ref]
- GSK3B is a gene associated with both circadian rhythm and mood disorders. A variant of GSK3B has been shown to double the risk of severe insomnia in depressed patients. These patients also had a greater insomnia response to antidepressant therapy.[ref] Note that this gene is also affected by lithium, affecting bipolar disorder.
- PER2: One of the core circadian clock genes, PER2, has variants with strong links to insomnia.
- TPH2 gene: Waking up really early and not being able to fall back to sleep is a form of insomnia known as sleep maintenance insomnia. A variant in the TPH2 gene, which converts tryptophan into serotonin and then melatonin, has been associated with an increased risk of sleep maintenance insomnia.
- GABRA6 gene: A recent study found that low GABA transmission, associated with rs3219151 T allele, was linked to depression, suicide risk, and insomnia. It is thought that the T allele increases plasma cortisol and stress response, and carriers of the T allele who had a recent life stress event were more likely to have problems with stress-related depression and sleep problems.[ref] GABA acts within the suprachiasmatic nucleus (a region of the brain controlling circadian rhythm) as a key signal in the neuronal circuits. Experiments have shown that GABA can “shift the circadian rhythm of the master clock.”[ref]
Restless Leg Syndrome and Periodic Limb Movement Disorder
Restless Leg Syndrome (RLS) is a fairly common disorder affecting about 10% of the US population. Periodic Limb Movement Disorder -PLMD (also called Periodic Limb Movements In Sleep – PLMS) is often lumped together with RLS in studies. The two often go together, with about 80%-90% of RLS sufferers also having PLMD.[ref]
Related article: More on RLS and PLMD
About 40% – 60% of people with RLS have a family history of it, suggesting a strong genetic component. People with a family history of RLS tend to get it at a younger age.[ref] In general, RLS is more likely to be found in women, in older people, and in those with iron storage issues.[ref]
People with restless leg syndrome are at an increased risk of psychiatric disorders. One study showed that 37% of people with RLS met the criteria for a psychiatric disorder – compared to only 15% of people without RLS.[ref]
- MEIS1 gene: The MEIS1 gene has been studied for restless leg syndrome. There are several MEIS1 SNPs that have links to an increased risk of RLS and PLMD.
- GABA Receptors: A study of patients with restless leg found that GABA receptor variants may affect restless leg syndrome. GABA, the main inhibitory neurotransmitter, keeps the neurons from being overexcited.[ref]
Narcolepsy Genes:
Narcolepsy, or excessive daytime sleepiness, occurs in about 1 in every 2,000 people in the US. It affects the brain’s ability to control sleep and waking, causing people to feel sleepy often throughout the day. One cause of narcolepsy is autoimmune disease.
Genetic studies on narcolepsy show that susceptibility is strongly associated with HLA-DRB1*1501 and HLA-DQB1*0602.
- HLA-DRB1*1501 is highly correlated with rs3135388 and found to influence the risk of several autoimmune diseases, including MS, lupus, and narcolepsy.
- HLA-DQB1*0602 is found in 90% of people who have narcolepsy, but it can’t be determined by a single SNP that I have found.
Sleep Overview Genotype Report:
A recent genome-wide analysis of sleep duration, timing, and disturbances found an overlap between sleep quality and the genetic variants associated with sleep disorders. Essentially, people with genetic variants linked with sleep disorders (whether diagnosed or not) were likely to have poor sleep quality. The study used data from 5000+ people wearing sleep trackers, and then it was replicated with another group.[ref]
Morning Grogginess and the ADA gene:
ADA gene: encodes adenosine deaminase, which breaks down and eliminates adenosine as we sleep. When adenosine is metabolized more slowly, you’ll feel groggy if you haven’t slept long enough.
Check your genetic data for rs73598374 (23andMe v4, v5; AncestryDNA)::
- C/C: typical clearance of adenosine
- C/T: reduced clearance of adenosine, more deep sleep, but may feel sleepy when waking up[ref]
- T/T: reduce clearance of adenosine, more deep sleep, but may feel sleepy when waking up
Members: Your genotype for rs73598374 is —.
Insomnia Genes:
GSK3B gene: The GSK3B gene involves both circadian rhythm and glucose metabolism. This is one gene that is influenced by lithium.
Check your genetic data for rs334558 (23andMe v4, v5; AncestryDNA):
- G/G: increased risk for severe insomnia in depression[ref]
- A/G: increased risk for severe insomnia in depression
- A/A: typical
Members: Your genotype for rs334558 is —.
PER2 gene: One of the core circadian clock genes, PER2, has links with insomnia.
Check your genetic data for rs7602358 (23andMe v4, AncestryDNA):
- G/G: increased risk for insomnia (up to 5-fold), especially with stress[ref]
- G/T: increased risk for insomnia
- T/T: typical risk for insomnia
Members: Your genotype for rs7602358 is —.
TPH2 gene: converts tryptophan into serotonin and then melatonin, has been associated with an increased risk of sleep maintenance insomnia.
Check your genetic data for rs4290270 (23andMe v4, AncestryDNA):
- T/T: increased risk of waking early, increased risk of depression[ref][ref]
- A/T: probably a slightly increased risk of waking early, depression (this is the most common genotype)
- A/A: typical
Members: Your genotype for rs4290270 is —.
GABRA6 gene: encodes a GABA-A receptor. Low GABA transmission is linked to insomnia.[ref]
Check your genetic data for rs3219151 (23andMe v4, v5; AncestryDNA):
- T/T: increased risk of depression, insomnia due to adverse life events
- C/T: increased risk of depression, insomnia due to adverse life events
- C/C: typical risk of insomnia
Members: Your genotype for rs3219151 is —.
NPSR1 gene: encodes the neuropeptide S receptor, which is activated by neuropeptide S and promotes wakefulness.
Check your genetic data for rs324981 (23andMe v4; AncestryDNA):
- A/A: increased relative risk of primary insomnia, prolonged sleep latency
- A/T: typical risk
- T/T: typical
Members: Your genotype for rs324981 is —.
Restless Leg Syndrome and Periodic Limb Movement Disorder
MEIS1 gene: encodes a homeobox protein. Homeobox genes are involved in forming organs and limbs in embryonic development, so the connection to RLS and PLMD is likely from altered development.
Check your genetic data for rs2300478 (23andMe v4, v5; AncestryDNA):
- G/G: greater than 1.7x risk of RLS, increased sympathovagal balance during N3 sleep stage[ref][ref]
- G/T: 1.7x risk of RLS
- T/T: typical risk of RLS
Members: Your genotype for rs2300478 is —.
BTBD9 gene:
Check your genetic data for rs3923809 (23andMe v4, v5; AncestryDNA):
- A/A: approx. 50% with this genotype will have RLS, 1.9x risk of PLMD without RLS, serum ferritin levels decreased 26%[ref]
- A/G: higher risk of RLS and PLMD, serum ferritin levels decreased 13%
- G/G: typcial risk of RLS
Members: Your genotype for rs3923809 is —.
Check your genetic data for rs9357271 (23andMe v4, v5; AncestryDNA):
- C/C: lower risk (<0.63) of RLS[ref]
- C/T: slightly lower risk of RLS
- T/T: typcial risk of RLS
Members: Your genotype for rs9357271 is —.
MAP2K5 gene:
Check your genetic data for rs6494696 (23andMe v4; AncestryDNA):
- G/G: increased risk of PLMD (most common allele)[ref]
- C/G: decreased risk of RLS
- C/C: decreased risk of RLS[ref]
Members: Your genotype for rs6494696 is —.
PTPRD gene:
Check your genetic data for rs1975197 (23andMe v4, v5; AncestryDNA):
- A/A: increased (1.8x) risk of RLS[ref]
- A/G: increased risk of RLS
- G/G: typcial risk of RLS
Members: Your genotype for rs1975197 is —.
GABRA4 gene: encodes a GABA Receptor. GABA is the primary inhibitory neurotransmitter that keeps the neurons from being overexcited.[ref]
Check your genetic data for rs2229940 (23andMe v4, v5; AncestryDNA):
- G/G: typical
- G/T: earlier age of onset for RLS
- T/T: earlier age of onset for RLS[ref], also, faster motor reaction times[ref]
Members: Your genotype for rs2229940 is —.
Narcolepsy Genes:
HLA-DRB1 gene:
Check your genetic data for rs3135388 (23andMe v4, v5; AncestryDNA):
- A/A: (HLA-DRB1*1501) increased risk of narcolepsy, MS[ref]
- A/G: (one copy of HLA-DRB1*1501) increased risk of narcolepsy
- G/G: typical risk
Members: Your genotype for rs3135388 is —.
Check your genetic data for rs1154155 (23andMe v4, v5; AncestryDNA):
- G/G: increased risk of narcolepsy (2.5x increased risk)[ref]
- G/T: increased risk of narcolepsy
- T/T: typical
Members: Your genotype for rs1154155 is —.
Circadian Rhythm Genes:
Our natural circadian clock is run by several core genes that rise and fall over a 24 hour period, setting the rhythm for all of our body’s functions. Sunlight hitting the retina in the morning resets the circadian clock.
Circadian rhythm disruptions have ties to obesity, difficulty in losing weight, diabetes, Parkinson’s, Alzheimer’s, heart disease, and ADHD symptoms.
CLOCK gene: The aptly named CLOCK gene is part of the core molecular circadian clock.
Check your genetic data for rs1801260 (23andMe v4, v5; AncestryDNA):
- G/G: higher activity levels in the evening, delayed sleep onset.[ref][ref]
- A/G: somewhat delayed sleep
- A/A: typical
Members: Your genotype for rs1801260 is —.
Check your genetic data for rs11932595 (23andMe v4, v5 AncestryDNA):
Members: Your genotype for rs11932595 is —.
PER2 gene: The PER2 (period 2) gene is part of your core circadian clock.
Check your genetic data for rs35333999 (23andMe v4, AncestryDNA):
- C/C: typical
- C/T: likely to stay up later, evening chronotype, longer circadian period
- T/T: likely to stay up later, evening chronotype, longer circadian period[ref]
Members: Your genotype for rs35333999 is —.
AANAT gene: AANAT (arylalkylamine N-acetyltransferase) controls the production of melatonin in the pineal gland. AANAT enzyme activity is high at night and tied to a person’s circadian rhythm. Polymorphisms in AANAT are more common in those with Delayed Sleep Phase Disorder (Japanese Study).
Check your genetic data for rs28936679 (23andMe v4 only):
- A/G: higher risk of Delayed Sleep Phase Disorder[ref], rare mutation found in less than 1% of the population.
- G/G: typical
Members: Your genotype for rs28936679 is —.
Lifehacks for improving sleep:
Eliminating Light at night:
One small thing that will make a HUGE difference in sleep and circadian rhythm function is to block blue light at night.
Our modern environment is full of light at night and especially in the blue wavelengths from LED bulbs, TVs, and phones. The blue wavelength (~480nm) is the exact wavelength that resets our circadian genes each morning. When you expose yourself to light in the blue wavelengths at night, it messes up your circadian rhythm and decreases your production of melatonin.
Your best bet for blocking the blue wavelengths at night is blue-blocking glasses. Look for ones that block 100% of blue light.
Alternatively, you could go with shifting the lighting color in your home after dark. There are color-changing bulbs as well as low-watt bulbs with a more yellow hue – often called candlelight bulbs or Edison bulbs.
You also want to decrease the overall brightness of your environment at night. So shutting off bright overhead lights and switching to lamps that contain the Edison bulbs will help. Make sure you also shut off your electronics (TV, laptop, cellphone, tablets) a couple of hours before bed as well.
Sleep in true dark: Make your bedroom as dark as possible for sleeping. Dim light from street lights can suppress melatonin production. Get some blackout curtains or shades for the windows, and cover up all the little glowing lights on any electronics.
Cooling off at bedtime:
Temperature is also important in sleep. Your body expects the temperature to drop when the sun goes down. Keep your bedroom as cool as you comfortably can at night.[ref]
There are also new options on the market for cooling your whole bed with a water-cooled mattress topper.
Supplements:
Melatonin (if needed):
Melatonin decreases significantly as we age, and older individuals may find that a low-dose supplement is beneficial for sleep quality and for promoting circadian rhythm.
Supplemental melatonin is available over the counter in most countries. If you aren’t used to taking melatonin, look for a supplement that is low-dose (1mg or less) and timed-release. Read more about supplemental melatonin.
Saffron Extract:
A six-week-long placebo-controlled trial found that saffron extract (15.5 mg/day) was effective for sleep. The study participants taking saffron had increased sleep time, improved ease in falling asleep, and improved sleep quality. [ref]
Restless leg syndrome:
There are several new studies that point to the role of adenosine in causing restless legs.[ref][ref] Reducing caffeine or stopping caffeine at lunch time may help.
- Hops extract and valerian root combined can block the effects of caffeine on the adenosine receptors. Both are known for their sleep-promoting effects, and both can be found in OTC herbal remedies for sleep and restless leg.[ref][ref]
Therapy devices are also studied for RLS:
- Near-infrared light therapy has been shown in a small study to help with restless leg syndrome.[ref]
- A medical device that puts pressure on the abductor hallucis and flexor hallucis brevis muscles has been shown in a clinical trial to reduce sleep disturbances due to RLS.[ref]
- Transcutaneous spinal direct current stimulation has been shown to decrease RLS.[ref]
A study showed that acupuncture plus gabapentin (prescription med for RLS) was more effective than gabapentin alone.[ref]
Vitamin B6:
A 2022 study found that 40 mg of vitamin B6 helped to reduce the severity of RLS and improve sleep quality.[ref]
Beating Morning Grogginess: ADA gene
The ADA gene variant that causes morning grogginess (along with increased deep sleep) may indicate that you simply need to make sure that you get enough sleep. Most adults need between 7 and 8.5 hours of sleep per night. Try adding in an extra half hour of sleep time and see if it cures your morning grogginess. You may just need a little extra time each night to adequately clear adenosine.
And yes, caffeine is an adenosine receptor antagonist and will probably make you feel much better in the mornings when you haven’t gotten adequate sleep.
Book recommendations:
For many, laying down to go to sleep causes their mind to race with all the worries and thoughts of the day. In addition to supplements and lifestyle hacks, behavioral therapy may help for long-term insomnia patients.
If you can’t find a therapist nearby, check out the book and workbook: Quiet Your Mind and Get to Sleep, written by two psychologists who specialize in sleep.
Another option – reading a nice, slightly boring non-fiction book can also help to calm the mind.
Music for sleep:
Check out Jason Stephenson’s deep sleep music:
Recap of your genes:
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| ADA | rs73598374 | T | -- | Decreased adenosine deaminase; more slow-wave sleep; groggy in the morning. |
| MEIS1 | rs2300478 | G | -- | Increased risk of restless leg syndrome and/or periodic limb movement disorder |
| GABRA | rs2229940 | T | -- | Increased risk of restless leg syndrome and/or periodic limb movement disorder |
| BTBD9 | rs3923809 | A | -- | Increased risk of restless leg syndrome and/or periodic limb movement disorder |
| BTBD9 | rs9357271 | C | -- | Lower risk (<0.63) of RLS |
| MAP2K5 | rs6494696 | G | -- | Increased risk of restless leg syndrome and/or periodic limb movement disorder |
| PTPRD | rs1975197 | A | -- | Increased risk of restless leg syndrome and/or periodic limb movement disorder |
| HLA-DRB | rs3135388 | A | -- | HLA-DRB1*1501; Increased risk of narcolepsy |
| HLA-DRB | rs1154155 | G | -- | Increased risk of narcolepsy |
| CLOCK | rs1801260 | G | -- | Higher activity level in the evening; often leading to delayed sleep |
| CLOCK | rs11932595 | G | -- | Increased risk of sleep difficulty or sleep disturbances |
| PER2 | rs35333999 | T | -- | Likely to stay up later with evening chronotype; this variant is linked to a longer circadian period |
| AANAT | rs28936679 | A | -- | Increased risk of Delayed Sleep Phase Disorder (rare) |
| GSK3B | rs334558 | G | -- | Increased risk of insomnia in depression |
| PER2 | rs7602358 | G | -- | Increased risk of insomnia; especially when stressed |
| GABRA6 | rs3219151 | T | -- | Increased risk of insomnia with adverse life events; increase risk of panic disorder |
| TPH2 | rs4290270 | T | -- | Increased risk of waking early, increased risk of depression |
| NPSR1 | rs324981 | A | -- | A/A: increased relative risk of primary insomnia |
[/mepr-show]
Related Articles and Genes:
Circadian Rhythms: Genes at the Core of Our Internal Clocks
Circadian rhythms are the natural biological rhythms that shape our biology. Most people know about the master clock in our brain that keeps us on a wake-sleep cycle over 24 hours. This is driven by our master ‘clock’ genes.
Restless Leg and Periodic Limb Movement Disorder: Genetics and Solutions
Twitchy legs, restless sleep… That urge to move your legs at night or being woken up with your leg moving rhythmically — both take a toll on sleep quality. And good sleep is foundational for overall health and wellbeing.
Genetics and Teeth Grinding (Bruxism)
Bruxism is a condition where you unconsciously clench or grind your teeth. This can occur when sleeping (sleep bruxism) or while you are awake. Bruxism can cause wear on the enamel of the teeth and even cause teeth to crack. Additionally, people with bruxism may have jaw pain, headaches, migraines, or sleep disorders.
How to log in to 23andMe and download raw data
Step-by-step instructions on how to download your raw data from 23andMe