Key takeaways:
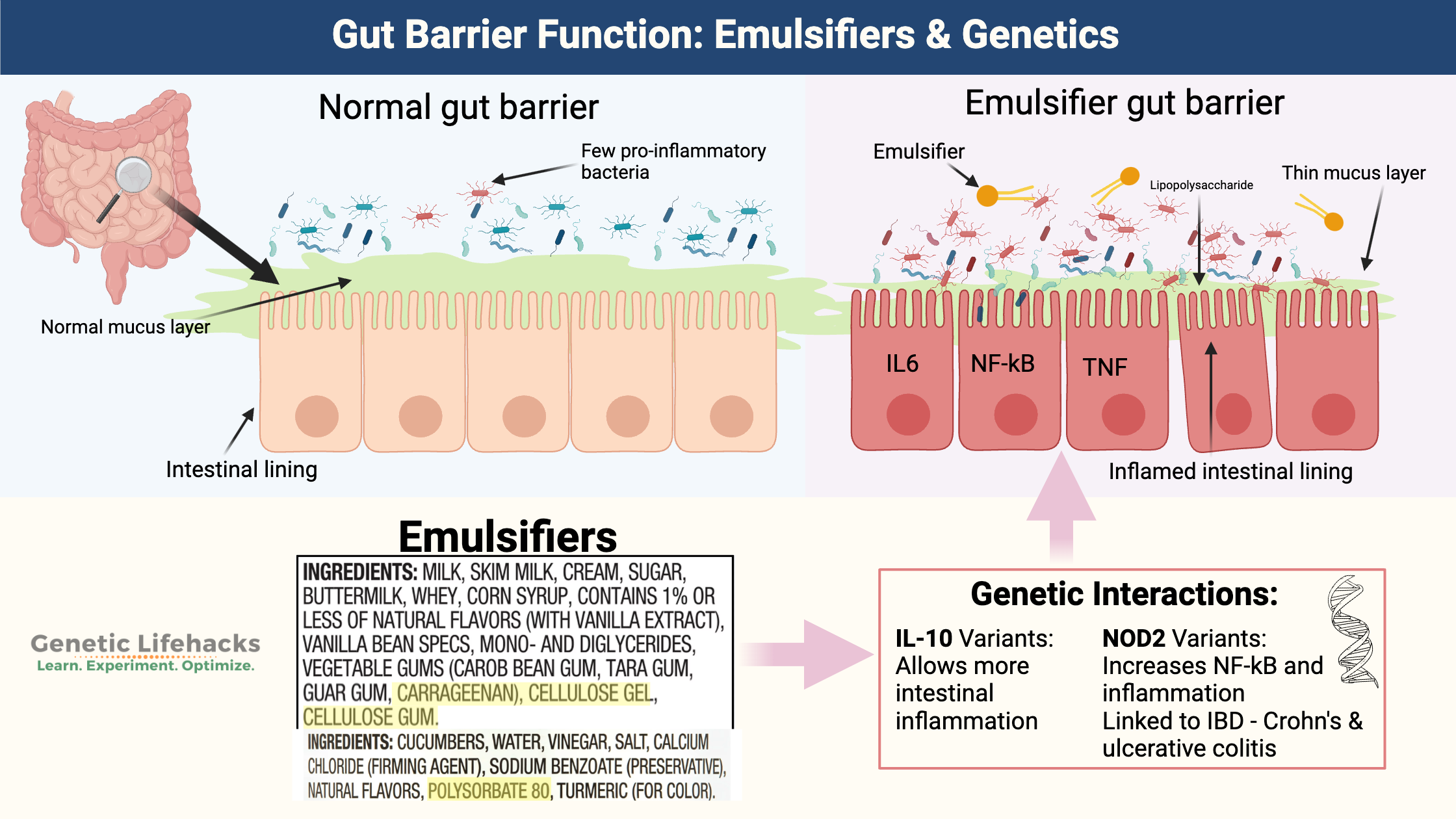
~ Your gut microbiome interacts with your intestinal barrier – the mucosa and cells lining your intestines.
~ Your genes play a role in how your body reacts to gut microbes and which microbes can flourish in your body.
~ Emulsifiers and surfactants in processed foods and medications can decrease the mucosal barrier, allowing gut bacteria to move closer to the intestinal cells and trigger an immune response.
~ Genetic variants in IL-10 and NOD2 significantly impact your body’s resilience to eating processed foods containing emulsifiers and surfactants.
Members will see their genotype report below, plus additional solutions in the Lifehacks section. Consider joining today.
Leaky Gut, Intestinal Barrier Function, and Emulsifiers
Your intestines do a miraculous job of allowing the absorption of nutrients from foods while keeping your gut microbes at bay.
The intestinal wall is lined with epithelial cells along with a mucosal barrier to keep out microbes and to protect against digestive enzymes. This mucosal barrier keeps microbes away from the epithelial cells and, thus, out of the body’s circulation.
The microbes in our guts are important and perform a variety of functions for us, including making some vitamins and short-chain fatty acids. But they have to stay in the right spot in the gut…
The mucosal barrier is really two layers – an inner layer that is firmly attached and an outer layer that is thicker and looser. The inner layer has few bacteria in it and contains secreted peptides that are antibacterial. The outer mucosal layer contains many different types of gut bacteria.[ref]
When the intestinal mucosal barrier is disrupted, your immune system gets activated by microbes in the gut, causing an inflammatory response. This can lead to autoimmune and inflammatory conditions such as food intolerances, IBD, and metabolic syndrome.
So, if a dysfunctional mucosal barrier can cause intestinal and autoimmune disorders, what does a thinner-than-normal barrier do? According to a bunch of new research, it causes low-level inflammation due to the translocation of bacteria, which drives weight gain and metabolic syndrome.[ref]
Emulsifiers, Packaged Foods, Inflammation
Research over the past decade shows that emulsifiers in common food products can lead to low-grade inflammation in the gut, especially when combined with certain genetic variations.[ref][ref]
Let’s dive into what these food additives do in the gut and how the alterations caused by gums and emulsifiers increase intestinal inflammation.
What are emulsifiers?
Emulsifiers help solve the age-old problem of getting water and oil to mix. Consisting of a water-loving and oil-loving end, emulsifiers are molecules that are attracted to both oil and water. Egg yolks are an example of a natural emulsifier.
Some of the first emulsifiers patented for use in foods were a derivative of fatty acids called mono- and diglycerides. Several patents from the 1930s show mono- and diglycerides being used for shortening – you know, like the Crisco your mom used to use in cookies. Cottonseed oil was cheap and abundant and became the oil of choice in shortening, used instead of lard in baking bread, cakes, and cookies.
These days, food manufacturers use emulsifiers to make food shelf-stable with a good texture. You’ll find emulsifiers on the ingredients labels for:
- most baked goods
- ice cream
- some deli meats
- pickled products
- salad dressings
- sauces
- coffee creamer, and more!
Emulsifiers can also act as surfactants, which reduce surface tension. Surfactants are commonly found in detergents – think of how a drop of dish detergent breaks up the grease in a pan.
Commonly used added emulsifiers:
Let’s define what has been specifically studied in regard to the gut mucosa.
The following emulsifiers/surfactants are common ingredients in processed foods that are linked to reducing intestinal mucosa thickness.[ref]
Carboxymethylcellulose (CMC):
Carboxymethylcellulose is a very common ingredient in foods, especially reduced-fat and gluten-free foods. It is also commonly found in ice cream as a stabilizer.[ref][ref]
- also known as CMC or cellulose gum,
- GRAS (generally regarded as safe) by the FDA and in Europe
- allowed to be included at up to 2% of the volume in various foods
- made from wood pulp or cotton processing
Polysorbate-80:
Polysorbate 80 is a surfactant and emulsifier used in foods and cosmetics. Ice cream often includes polysorbate 80 (up to 0.5%) to help it stay smooth. It is also found in most pickles and pickled products.
- also known as P80 or Tween 80
- allowed at levels up to 1% in certain foods
The acceptable daily intake (World Health Organization) is 25 mg/kg body weight/day, acute toxicity is low, and it is not considered cancer-causing.[ref]
Carrageenan:
Another common food additive is carrageenan, which is derived from red seaweed. As a natural product, it is used even in organic foods as a food additive, thickener, and emulsifier. It is classified as GRAS by the FDA.
Animal studies show that carrageenan increases intestinal inflammation by increasing IL-8 (inflammatory cytokine) expression from exposure to bacteria.[ref] One study explains that carrageenan “degrades the mucous barrier and breaks down the mucous barrier, causing an inflammatory reaction.”[ref]
Other emulsifiers:
A 2021 study by Naimi, et. al. investigated 20 more emulsifiers to see their impact on the gut microbiome. The results showed a couple of important considerations:[ref]
- Lecithin and mono- and diglycerides have little to no impact on the gut microbiome. (Lecithin is the natural emulsifier found in egg yolks)
- The impact on the gut microbiome from gum arabic, iota carrageenan, locust bean gum, guar gum, and agar-agar is reversible — meaning that once the gums are removed from the diet, the gut microbiome goes back to normal.
- Carboxymethyl cellulose’s impact on the composition of the gut microbiome may be non-reversible.
- Finally, “xantham gum, sorbitan monostearate, glyceryl stearate, maltodextrin, and P80 impacted various microbiota parameters, both compositionally and/or functionally, in a non-reversible manner”.
Emulsifiers in medications and supplements:
Drug manufacturers take advantage of the surfactant properties that decrease mucosal thickness. If the drug can get past the mucosal barrier, it is better absorbed. So some medications deliberately include polysorbate 80, polysorbate 20, or carboxymethylcellulose to help with absorption. [ref][ref]
More on emulsifiers in medications in the Lifehacks section below – including drugs that contain surfactants.
What do emulsifiers do in the gut?
First, I want to make clear that emulsifiers aren’t something that is going to hurt you immediately. They are all ‘safe for human consumption’. Decades ago, researchers investigated the toxicity and cancer-causing properties of carboxymethyl cellulose, hydroxypropyl methylcellulose, and polysorbate 80.[ref][ref][ref] These emulsifiers were found to be acceptable for use as food additives.[ref][ref][ref] They have been identified as safe for human consumption by the FDA.
However, new studies are showing the chronic, low-dose impact of emulsifiers on the intestinal mucosal barrier. These studies paint a new picture of the health effects of emulsifiers.
The gut mucosa interacts with the bacteria in your gut, keeping them at the right distance from your gut lining to prevent activation of the immune system. Multiple studies over the past two decades show that there is a link between dietary emulsifiers and a reduction or thinning of the mucosal layer that protects your intestinal cells. This allows bacteria to translocate and come in contact with the epithelial cells lining the intestines. Your immune system then reacts by producing inflammatory cytokines. The inflamed gut lining can allow bacteria into the bloodstream as well as being linked to chronic diseases including metabolic syndrome.[ref]
Studies on chronic effects of emulsifiers/surfactants in ultra-processed foods:
Low grade inflammation, metabolic syndrome:
Researchers from Georgia State University (Chassaing, et. al.) examined whether emulsifiers (specifically Carboxymethylcellulose and Polysorbate 80) increased low-grade inflammation, resulting in metabolic syndrome in mice. The results showed:[ref]
- Carboxymethylcellulose in low levels (0.1 – 0.5% of their food) increased body weight and caused low-grade inflammation.
- Polysorbate 80 in low levels (0.1 – 0.5% of their food) also increased body weight and caused low-grade inflammation. At the 0.5% level, polysorbate 80 caused dysglycemia.
- Most importantly, the “Emulsifier-induced metabolic syndrome was also observed in older mice…and persisted for at least 6 weeks after stopping emulsifier consumption”.
To sum up, the emulsifiers used in this study caused bacteria to be located closer to the epithelial cells of the intestine. For mice that were genetically susceptible to colitis, this caused colitis. For normal mice, this caused low-grade inflammation, fat gain, and mild blood sugar level issues.
Reduced intestinal mucosa thickness:
Researchers found emulsifiers, specifically polysorbate 80, caused impaired glycemic tolerance, increased gall bladder size, and reduced intestinal mucosa thickness. The reduced mucosal thickness causes intestinal bacteria to be closer to the epithelial cells and increases inflammation.[ref]
Increased intestinal permeability (leaky gut):
Food additives such as emulsifiers, organic solvents, gluten, and nanoparticles used in processed food increase intestinal permeability. Essentially – they cause leaky gut, which may explain the rise in autoimmune diseases.[ref]
Moves E. coli to touch the intestinal cells:
Researchers looked at the effect of non-starch polysaccharides vs. food emulsifiers on the ability of E. coli to the mucosa in the intestinal tract. They showed that natural plant fibers, such as broccoli and plantain, reduced E. coli moving into the intestinal cells. However, the addition of polysorbate 80 at 0.01% increased E. coli translocation by 59-fold
Shifts the microbiome:
In a recent animal study, both carboxyl methylcellulose and polysorbate 80 altered the intestinal mucosa, impacting barrier and structural properties. This changed the way that bacteria, such as E. coli, interacted with intestinal tissue.[ref] Another recent study showed CMC, polysorbate 80, and soy lecithin shifted the gut microbiome away from the ‘good’ bacteria that produce short-chain fatty acids. [ref]
Abdominal discomfort, gut inflammation (humans):
A double-blind controlled-feeding study of carboxymethylcellulose in healthy adults was compared to a volunteer group eating an emulsifier-free diet. The adults randomized to eat 15g/day of CMC had modestly increased abdominal discomfort after eating. More importantly, it shifted their gut microbiome to reduce the production of short-chain fatty acids. About 20% of the participants had gut inflammation due to microbiota encroachment into their inner mucus layer.[ref]
Genetic interactions with emulsifiers and leaky gut:
Studies clearly show that emulsifiers are causing changes in the mucosal lining and causing inflammation, but not everyone is going to be affected the same way. The studies that link emulsifiers to decreased mucosal barrier and inflammation in the gut associate the changes to specific genetic variants in the IL10 and NOD2 genes. These two genes, in humans, increase the risk of inflammatory bowel disease.[ref]
The key to whether emulsifiers cause intestinal barrier inflammation and leakiness in people may on genetics. Some (perhaps most) people can eat foods containing emulsifiers without a lot of issues, but for people with IL-10 or NOD2 genetic variants, there may be an exacerbated inflammatory response to the thinned mucosal barrier.
Emulsifiers and Gut Barrier Genotype Report:
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Lifehacks:
If you have problems related to chronic inflammation, leaky gut, or metabolic syndrome, you may want to seriously consider how much processed food containing emulsifiers you eat on a regular basis.
The genetic variants in IL-10 and NOD2 are additive factors to consider here. Switching to a whole foods diet that avoids emulsifiers and surfactants is not easy, but it may bring considerable long-term benefits for your intestinal barrier function.
Avoiding emulsifiers: Is it possible?
Reading labels:
To be honest, avoiding emulsifiers in processed foods is labor-intensive and inconvenient. Eating out becomes nearly impossible, and a trip to the grocery store means time spent reading all the labels. Is it worth it? For some people with a genetic susceptibility to intestinal inflammation, the answer is likely yes. For others, just avoiding pre-packaged foods when possible may be enough.
Natural supplements contain emulsifiers:
One big source of methylcellulose for people eating a whole-foods diet is supplements. Many supplement manufacturers have switched to capsules made of cellulose instead of gelatin to be vegetarian-friendly. The capsules are usually labeled as vegetable capsules and made from plant cellulose. Quite a few tablet forms of vitamins and supplements include either CMC or polysorbate 80, as well.
Hydroxypropyl methylcellulose is the most common form of methylcellulose that you’ll find in capsules, bu there are different thicknesses and structures to these capsules that cause them to degrade at different rates in your stomach or intestines.[ref]
I don’t have all the answers here in regard to which methylcellulose capsules are more likely to cause mucosal thinning. My suggestion: Read the labels on your supplements and look for brands that offer gelatin for the capsules. Another alternative is to buy bulk powder supplements and either create your own capsules with empty gelatin capsules or take the powdered form.
Pharmaceuticals that use emulsifiers and surfactants:
Related Articles and Topics:
Genetic reasons why Low FODMAPs isn’t working for you (SI Gene)
Histamine Intolerance: Understanding Your Genetics and Managing Symptoms