Did you know that breast cancer is the second most common cancer, with 13% of women developing it by age 95? While most cases aren’t due to hereditary mutations, about 10% of women with breast cancer carry mutations in the BRCA1 or BRCA2 genes. This rises to 25% in women with triple-negative breast cancer.[ref][ref]
In this article, I’ll be explaining the interactions between the BRCA1/2 mutations and other genetic variants, as well as giving an overview of the research on diet and lifestyle interactions that can increase cancer risk in people with these mutations. However, I won’t be covering how to check your BRCA status in your raw genetic data… (more on why in just a bit).
Listen to the article:
BRCA1 and BRCA2 mutations:
Let’s dive into what the BRCA1 and BRCA2 mutations actually are.
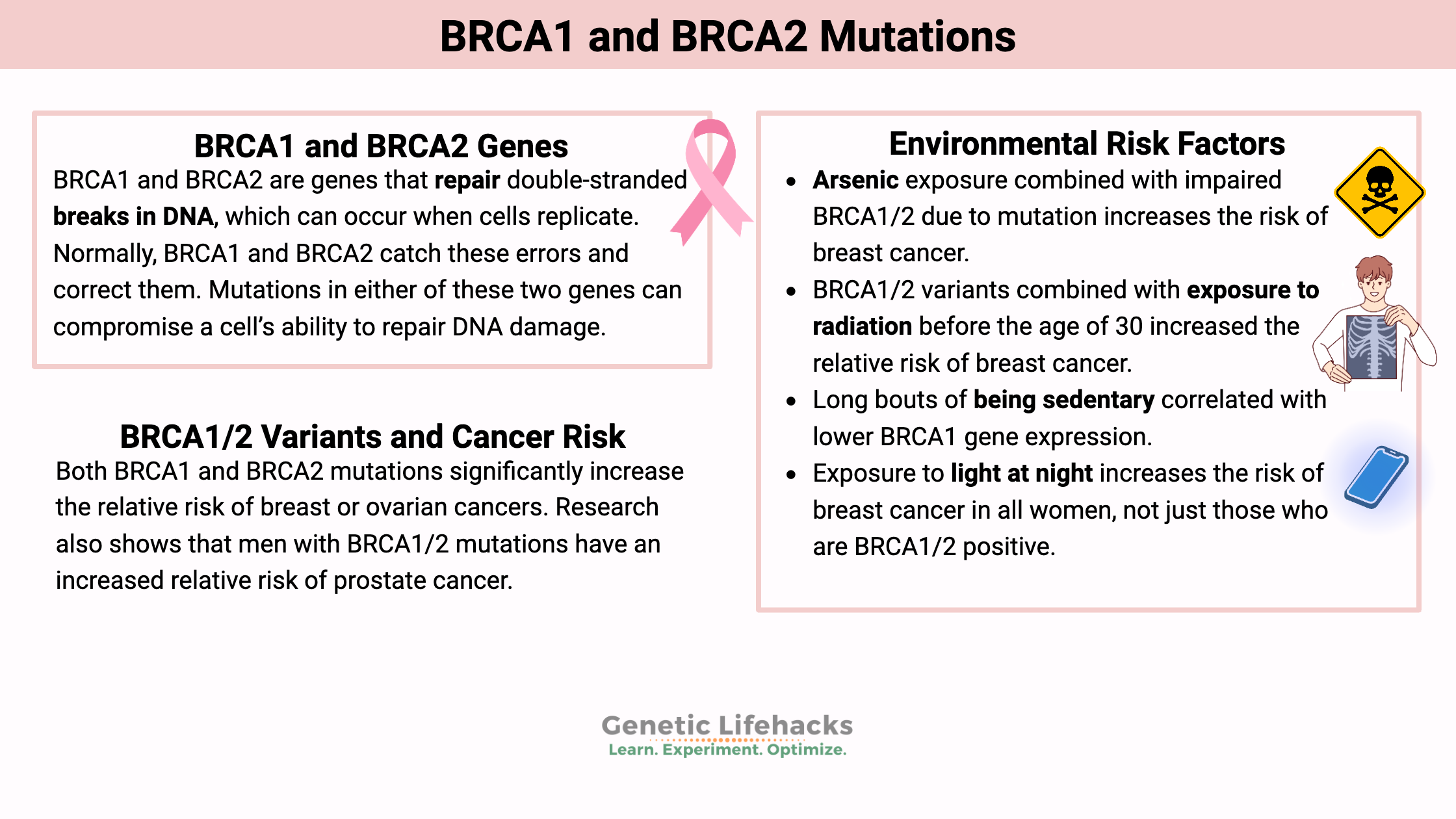
BRCA1 and BRCA2 are genes that repair double-stranded breaks in DNA, which can occur when cells replicate. Normally, BRCA1 and BRCA2 catch these errors and correct them. Mutations in either of these two genes can compromise a cell’s ability to repair DNA damage. Damage to DNA can lead to an accumulation of mutations that cause cancer to develop (e.g., a mutation in an oncogene that isn’t repaired).
Both BRCA1 and BRCA2 mutations significantly increase the relative risk of breast or ovarian cancers. Over 700 mutations have been identified in BRCA1, and 1800 mutations have been found in the BRCA2 gene. Only one copy of a mutation is needed to cause the increase in cancer risk, and 1 in 400 women carry the mutation on average across populations.[ref][ref]
While some BRCA1 and BRCA2 mutations can be found in 23andMe or AncestryDNA data, I don’t encourage people to use their raw data to look for these mutations for a couple of reasons. First, the raw data isn’t guaranteed to be clinically accurate, so false positives or false negatives are a real possibility when looking at rare mutations. Second, there are hundreds of BRCA1/2 mutations, and the raw data only covers a small percentage of them. Instead, I would encourage anyone with a strong family history of breast or ovarian cancer to talk with their doctor about getting a full test for hereditary cancer genes.
There are a number of companies now offering testing for BRCA1/2 mutations. Most require a physician’s approval and others allow people to order the test themselves – along with a telehealth provider. Please read reviews and do your due diligence — I have no first-hand experience here.
Here are just some of the options:
- LabCorp BRCAssure
- Color BRCA1/2
- Myriad BRCA1/2 Test
- Ambry Genetics BRCANext
- Natera Empower Hereditary Cancer Test
Your physician or a genetic counselor can help you understand the results of the testing and figure out the next steps to take.
Relative risk vs. absolute risk:
It’s important to understand the difference between relative risk and absolute risk when talking about cancer risk. Relative risk compares the increase in risk to the odds of getting the condition.
Let me give you an example: If the odds of getting an uncommon cancer is 1 in 1,000 (or 0.1%), then a mutation that increases the relative risk by four-fold will increase your absolute risk of the rare cancer to 4 in 1,000 (0.4%).
However, for a common cancer like breast cancer in women, the absolute risk is 1 in 8. Then a mutation that increases the risk of breast cancer by 4-fold would give you a 1 in 2 lifetime absolute risk (50%).
In men, though, the absolute lifetime risk of breast cancer is less than 1 in 1,000. So even though a man could be at the same 4-fold increase in relative risk from the BRCA mutation, it is still uncommon to get male breast cancer.
Therefore, it’s important to consider both relative and absolute risk when discussing the impact of any genetic variable or environmental factor on cancer likelihood.
Prostate cancer and other cancer risk:
While my focus in this article is on breast or ovarian cancer, I wanted to also point out that research shows that men with BRCA1/2 mutations have an increased relative risk of prostate cancer.[ref][ref]
The BRCA1/2 mutations are also linked to an increased relative risk of pancreatic, gallbladder, and stomach cancers. These are less common types of cancer, but it is important not to ignore signs of any of these cancers. [ref] Endometrial cancer risk is also increased in BRCA1/2 mutation carriers.[ref]
Interactions with BRCA1/2:
While BRCA1/2 mutations increase the risk of several types of cancer, not everyone with these mutations will go on to develop breast or ovarian cancers. Let’s explore some factors that can influence cancer risk in individuals with BRCA1/2 mutations.
Family history of breast or ovarian cancer:
While different BRCA mutations influence the absolute risk a little bit, studies over the past few decades showed, on average, that women with a BRCA1 mutation have a ~65% absolute risk of breast cancer and a ~39% chance of ovarian cancer by age 70. Those with a BRCA2 mutation have a 45% risk of breast cancer and an 11% risk of ovarian cancer by age 70.[ref] This also means that, on average, 35% of women with BRCA1 and 55% of women with BRCA2 mutations don’t get breast cancer by the age of 70.
However, those studies on the statistical risk are all done on women who most likely got tested for the BRCA mutations due to having a strong family history of breast cancer, adding in a bias that may overestimate the absolute risk for someone without a family history of breast cancer.
A 2023 study looked at the genetic data of ~250,000 UK Biobank women participants to see how BRCA1 and BRCA2 mutations affected cancer risk at the population level. The results showed that women with BRCA2 without a family history of breast cancer didn’t have as much of an increased risk of cancer.[ref] An article about the study explains the absolute risk by age 60 this way: “…simply carrying a disease-causing BRCA variant was linked to a breast cancer risk of 18% (for BRCA2) and 23% (for BRCA1) by age 60. Having a close relative who has had the condition elevated the risk to 24% (for BRCA2) and 45% (for BRCA1).”
Polygenic risk scores:
Large genetic studies have identified several hundred common genetic variants that increase or decrease the risk of breast cancer by a little bit. Everyone carries some of these variants, and for women who are BRCA1/2 positive, the addition of common risk variants can increase or decrease their relative risk a bit.[ref]
At some point, this type of testing may be widely available and able to help an individual BRCA1/2 mutation carrier with decision-making. However, at this point, knowing the cancer history from both sides of the family is going to tell you a lot, even without knowing your exact polygenic risk score.
I’ll get into the genetic studies, including studies showing no impact, in the genotype report section. Now let’s talk about some environmental risk factors that can influence cancer risk in individuals with BRCA1/2 mutations.
Environmental Risk Factors that interact with BRCA1/2:
One part of family history is genetics, but another part is an increase in exposure to the same environmental factors.
Research shows that some specific risk factors are more important with BRCA1 or BRCA2 mutations. It’s important to note that the impact of these environmental factors may vary depending on the specific mutation, the timing and duration of exposure, and potential interactions with other genetic and environmental factors.
Arsenic from food or water:
Arsenic causes oxidative stress and inhibits DNA repair pathways, resulting in DNA damage. Studies clearly show that arsenic exposure combined with impaired BRCA1/2 due to mutation increases the risk of breast cancer. In fact, one study found that BRCA1 mutation carriers with higher blood arsenic levels were at double the risk of breast cancer. The study divided women with BRCA1 mutations into two groups, based on whether their blood arsenic level was higher or lower than the median. The half with slightly higher blood arsenic levels were at double the risk of breast cancer.[ref][ref][ref][ref]
In the US, about 7% of water wells contain arsenic at 10 µg/L levels.[ref] Arsenic can also be found in foods grown in contaminated soil or water. Rice is particularly prone to absorbing arsenic, and in areas contaminated with pesticides containing arsenic, the content in rice can be quite high. For example, organic brown rice grown in Australia contains approximately the maximum recommended daily limit of arsenic. In comparison, rice grown in India had about a quarter of that amount.[ref]
Gluten-free diets may seem like a healthy choice, but most gluten-free bread and pasta replacements contain rice flour. A study showed that people eating a gluten-free diet had almost double the arsenic concentration in their urine.[ref]
Radiation exposure:
A study involving ~2,000 BRCA1/2 mutation carriers showed that exposure to diagnostic radiation before the age of 30 increased the relative risk of breast cancer (hazard ratio 1.9). This study started in 1993 and followed women with BRCA mutations for two decades. The conclusion of the study recommended that non-ionizing radiation, such as MRI, be used for breast cancer surveillance in younger women with BRCA1/2 mutations.[ref] This is something to discuss with your doctor.
Ionizing radiation causes double-stranded breaks, which the BRCA1/2 genes are responsible for fixing. Chest X-rays and mammograms both use ionizing radiation.
However, not all studies show that exposure to ionizing radiation is more of a problem with the BRCA mutations. A recent review paper summarizes the studies from the past two decades, with earlier studies involving older women showing no increase in cancer risk from radiation. In 2016, though, studies were done on BRCA mutation carriers using a new type of radiosensitivity indicator. These studies showed that women with BRCA1 and BRCA2 mutations were more sensitive to radiation. [ref]
Polycyclic aromatic hydrocarbons:
Polycyclic aromatic hydrocarbons, or PAHs, are another environmental factor to consider. PAHs are a class of chemicals found in diesel exhaust, cigarette smoke, and smog. Exposure to PAHs can cause DNA damage including double-strand breaks.[ref][ref] A study of occupations in male breast cancer patients with BRCA1/2 mutations showed that truck driving was the most frequent occupation. The researchers theorized that exposure to PAHs may have been the link.[ref] Another study found that women exposed to higher traffic emissions had a 2-fold higher risk of breast cancer. Note that this study was not specific to BRCA mutations.[ref]
Light at night:
Exposure to light at night increases the risk of breast cancer in all women, not just those who are BRCA1/2 positive. Epidemiological studies show an increase in breast cancer risk, and studies in animals explain multiple mechanisms of action.
Studying the effect of ambient light at night is difficult since it is so prevalent, but a 2023 meta-analysis looked at 21 studies on breast cancer risk from light at night. A few studies showed no increase in cancer risk from light at night, but others showed up to a 65% increase in risk. Combining all the data, the analysis came up with a 16% increase in breast cancer risk from light exposure at night.[ref][ref][ref][ref]
Melatonin levels are suppressed by light in the blue wavelengths after dark. In addition to its role in sleep, melatonin at a cellular level is an endogenous antioxidant. It also plays a role in tumor prevention and stopping metastasis.[ref]
Melatonin is only part of the picture here. The core circadian clock is controlled, in part, by exposure to light during the day and the absence of light at night. The circadian clock controls gene expression for many genes that vary over the course of a day, such as digestive enzymes, cellular repair genes, and immune response. BRCA1 and BRCA2 gene expression levels vary over the course of 24 hours, with a peak during midday and low levels by midnight. [ref]
Related article: Why light at night increases cancer risk
Breastfeeding reduces the risk:
Studies show that for BRCA1 mutation carriers, breastfeeding for at least a year reduces the risk of breast cancer. Breastfeeding causes changes in the breast tissue, and these changes are protective against breast cancers.[ref]
Physical activity reduces the risk:
A small study looked at the differences in BRCA1 gene expression due to activity level. The study showed that long bouts of being sedentary correlated with lower BRCA1 gene expression. While the study needs to be replicated, other studies show similar trends. For example, a study showed that BRCA1/2 mutation carriers who were more active during adolescence, such as playing sports, had a lower risk of premenopausal breast cancer and delayed age of onset.[ref][ref]
Oral contraceptive use:
A recent study on combined-type oral contraceptive use showed that it increased the risk of breast cancer cases in BRCA1 and BRCA2 mutation carriers by the age of 40. The results showed that there were about 10% more cancer cases in BRCA1 mutation-positive oral contraceptive users by age 35. However, the prior use of oral contraceptives seemed to decrease the risk of breast cancer in later years. [ref – open access study] This is one study that you may want to discuss with your gynecologist. I’m not clear as to whether the decreased cancer risk in later years was due to the women already having had cancer earlier.
A meta-analysis of studies on oral contraceptives included 20 studies on women with BRCA1 or BRCA2 mutations. The combined data showed that the use of oral contraceptives increased the relative risk of breast cancer by 24% but decreased the risk of ovarian cancer.[ref] Again – I don’t know that there is a clear overall answer for BRCA mutation carriers here, and advice from a good physician who knows your medical situation is advisable.
In addition to environmental factors, genetic variations in other genes can also influence cancer risk in individuals with BRCA1/2 mutations. Let’s take a closer look at some of these genetic interactions.
Genetic interactions:
Lifehacks:
I want to emphasize again that anyone with a BRCA1 or BRCA2 mutation needs good advice from a trusted physician. The information below is just for educational purposes – letting you know what some research shows so that you can talk with your doctor about it. I encourage you to read the referenced studies for yourself and keep up with new research. Please consult with your doctor before starting any type of supplement.
Avoiding arsenic:
As explained above, BRCA1-positive women in the upper half of arsenic exposure were at double the cancer risk.[ref] This is a huge, modifiable risk factor.
Rice grown in water that contains arsenic will be high in arsenic. Understanding where your rice is grown is essential (or alternatively, avoiding eating rice). Additionally, if you are on well water, have your water tested to know whether or not it is high in naturally occurring inorganic arsenic. Read the related article on arsenic for more details.
Related article: Arsenic and your genes
Sleeping well and avoiding light at night:
The studies on light at night and breast cancer risk are compelling. Here are a few practical ideas on how to decrease light exposure after dark:
- Turn off bright overhead lights after dark
- Shut off anything with LED screens (TV, phone, iPad) a couple of hours before bedtime
- Sleep in a dark room with blackout curtains
100% Blue-blocking glasses:
Blocking blue light at night with orange-lensed glasses can help if you are in a situation where you can’t easily decrease your exposure to light at night.
Sun exposure during the day, vitamin D:
Exposure to sunlight in the morning hours boosts melatonin production at night and helps circadian gene expression stay on track. Sun exposure can also increase vitamin D levels. Higher vitamin D levels may help protect against cancer in women with BRCA1 mutations. A study on BRCA1 carriers found that they have lower serum vitamin D levels and reduced vitamin D receptor expression in the ovaries and fallopian tube epithelium.[ref]
Cruciferous vegetables or supplements:
Many studies point to higher cruciferous vegetable intake being protective against breast cancer. For example, women who ate the highest amounts of cabbage and broccoli reduced their relative risk of breast cancer by around 25-30%. In looking at several different studies, cabbage seems to have the most impact on breast cancer prevention.[ref]
In BRCA1/2 mutation carriers, a Korean study found that higher isoflavone intake (found in cruciferous vegetables) reduced the risk of breast cancer.[ref]
Sulforaphane (from broccoli):
Available as a supplement or in high amounts in broccoli sprouts, sulforaphane has been studied specifically in BRCA1 mutation cell lines. The results showed that the effect of sulforaphane depended on the specific mutation. Many other studies on breast cancer cells (without taking into account BRCA mutations) strongly show that sulforaphane decreased tumor cell proliferation. [ref][ref]
Related article: Sulforaphane research studies
DIM (from cruciferous vegetables):
3,3′-diindolylmethane (DIM) is a phytochemical derived from cruciferous vegetables with possible breast cancer-preventative effects in some situations. Cell studies show that DIM upregulates BRCA1 and BRCA2 in breast cancer cells. In women with a BRCA1 mutation, taking 300 mg/day of a DIM supplement increased BRCA1 mRNA expression. However, this was a really small study (18 women) and needs to be replicated.[ref] Another small study on women with BRCA mutations looked at the effects of 100mg/day of DIM for one year of fibroglandular breast tissue. The results showed a decrease in fibroglandular tissue score in the women on DIM and no change in an age-matched control group not taking DIM.[ref]
Limiting alcohol:
A study in French-Canadian women with BRCA mutations showed that drinking 2 or more bottles of beer or more than 10 oz of wine per week increased the relative risk of cancer. [ref] However, another international study did not show a link between alcohol consumption, BRCA1/2 mutations, and cancer risk.[ref]
Recap of your genes:
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| GSTO1 | rs4925 | A | -- | increased DNA damage in BRCA1/BRCA2 mutation carriers |
| CYP1A2 | rs762551 | C | -- | a study showed coffee consumption before age 35 may reduce the risk of breast cancer in BRCA1 carriers. |
| VDR | rs1544410 | T | -- | possibly lower vitamin D, linked with a possible increase in the risk of breast cancer at a younger age in BRCA1/2 * |
| RIPOR2 | rs9393597 | G | -- | GWAS shows increased relative risk of breast cancer in BRCA2 mutation carriers in the UK biobank, replication study including other ancestry groups failed to find statistical significance. |
Remember, knowledge is power, and staying up-to-date on the latest research can help you make the best decisions for your health.
Related articles: