Key takeaways:
- The Epstein-Barr Virus (EBV) infects most people worldwide, remains in the body for life, and can reactivate under certain conditions.
- EBV is linked to mononucleosis, several cancers, and autoimmune diseases like MS, lupus, and Sjögren’s syndrome.
- Genetics plays a key role in who gets severe EBV symptoms and related diseases, with specific gene variants increasing risk.
- EBV reactivation is associated with chronic illnesses such as ME/CFS and Long Covid, especially after immune stress or infection. It is also implicated in COPD and chronic respiratory conditions in aging.
What is Epstein-Barr Virus?
The Epstein-Barr virus (EBV) is a type of human herpesvirus and is one of the most common viruses to which we are all exposed. It’s estimated that 90% of people are infected with the Epstein-Barr virus at some point in their lives. Once you’ve been infected, the virus sticks around for the rest of your life.
Mononucleosis, or mono, is caused by an EBV infection during the teenage or early adult years. When someone contracts EBV at other ages, such as during early childhood, the symptoms may be mild, resembling a brief cold, or the infection may be asymptomatic.
Dr. Anthony Epstein discovered EBV in a biopsy of Burkitt’s lymphoma cells in 1964. Over the next two decades, further studies established EBV as a cause of specific types of cancer, including lymphomas, throat cancer, and some stomach cancers[ref][ref]
More recently, researchers have found that EBV infection and reactivity are connected to several autoimmune diseases, ME/CFS (chronic fatigue syndrome), and possibly long Covid.
EBV Lifecycle: Sticking around forever?
The Epstein-Barr virus is a double-stranded DNA virus surrounded by a nucleocapsid and a lipid envelope. It primarily infects B cells (a type of white blood cell) and epithelial cells that line your throat, nose, stomach, and intestines.
Cell entry:
In epithelial cells, neuropilin 1 (NRP1) is important in how the virus gains entry to the cell. Decreased NRP1 suppresses infection, while increased NRP1 enhances it. For B cells, the virus enters through interaction with CD21 or CD35 receptors and HLA class II receptors on the cell surface.[ref]
Related Article: Neuropilins: Neurodevelopmental Disorders, Gut Barrier, & Covid Brain
Lytic phase:
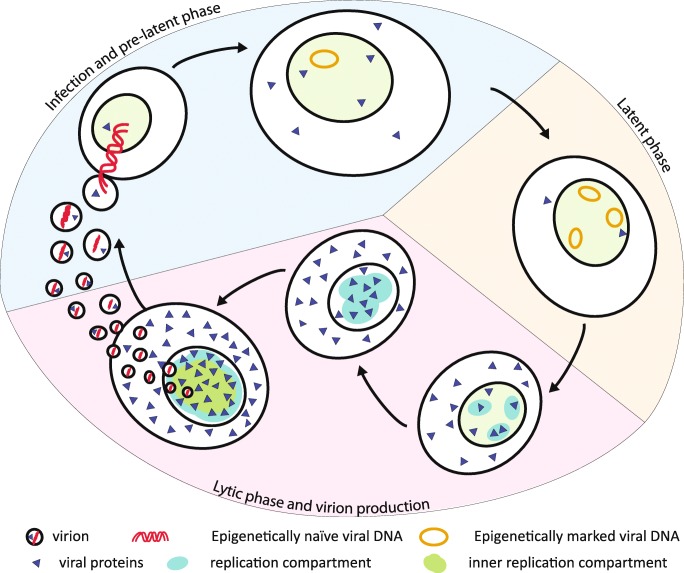
The lytic cycle is the primary infectious phase of viral reproduction. The Epstein-Barr virus enters epithelial cells, such as the lining of the throat and nose, and replicates rapidly. The replicated virus then buds off and leaves the epithelial cells. It is then taken up by B cells in the immune system.[ref]
Latency:
In the latent phase, the viral DNA becomes circular and isn’t actively replicating in the B cells. This creates a reservoir for the virus to remain in a latent, inactive form in B cells for life. The viral DNA remains in the nucleus of the B cells but is methylated, or turned off, so that it does not replicate.[ref]
Reactivation:
While EBV stays latent, or dormant, in B cells for most people, it can be reactivated in some people in specific circumstances. The lifelong persistence and then periodic reactivation in a small percentage of people explain why EBV is continuously present in the human population.[ref]
| Phase | Description | Key Cell Types | Key Proteins/Markers |
|---|---|---|---|
| Lytic | Active replication, virus spreads | Epithelial, B cells | Zta, Rta |
| Latency | Dormant, non-replicating viral DNA | B cells | Methylated DNA |
| Reactivation | Dormant virus becomes active again | B cells | Zta, Rta |
EBV-Associated Diseases:
In addition to causing certain types of lymphomas and nasopharyngeal cancers, Epstein-Barr virus infection and reactivation are associated with several diseases. The genetic variants that increase susceptibility will be covered in the Genotype Report section below.
Overview of EBV-Associated Diseases
| Disease | Main Symptoms | EBV Role/Notes | Genetic Factors |
|---|---|---|---|
| Mononucleosis | Fever, sore throat, fatigue, etc. | Primary infection in teens/adults | HLA, IL10 variants |
| Autoimmune – Sjögren’s Syndrome | Dry mouth, fatigue, joint pain | EBV in salivary glands | HLA-DR antigens |
| Autoimmune – Lupus | Autoimmune symptoms | IgAa levels for EBV proteins | CD40, IL10 |
| Autoimmune – Multiple Sclerosis (MS) | Neurological symptoms | Strong epidemiological link | HLA-DRB1*15:01, CD36 |
| ME/CFS, Long Covid | Chronic fatigue, brain fog, etc. | EBV reactivation found in subset | Various immune genes |
| COPD | Respiratory problems | EBV reactivation found during exacerbations | undetermined |
Let’s dive into the details on all of these conditions and how/why they are connected to the Epstein-Barr virus.
Mononucleosis (mono):
Although approximately 90% of adults carry antibodies to the Epstein-Barr virus, which causes mononucleosis, fewer than 30% of people actually experience symptoms. Your immune response and the age at which you encounter the virus greatly impact whether you get mono and how sick you get.
If you get the Epstein-Barr virus as a teenager or young adult, you are much more likely to develop mono from it. Symptoms of mono include fever, sore throat, fatigue, enlarged spleen, swollen lymph nodes, and sometimes a rash. Mono usually lasts for 2-4 weeks, but the fatigue can continue for a month or more.[ref]
Genetic susceptibility to mono:
Twin studies are one way to determine the heritability of a condition. They show that identical twins are twice as likely to both have mono compared to fraternal twin siblings, indicating a stronger role of genetic variants in the symptoms of mono.[ref]
One study found that certain HLA polymorphisms increase the risk of mononucleosis when exposed to the Epstein-Barr virus (EBV) during adolescence or adulthood. Interleukin 10 (IL-10) is produced during inflammation to regulate the immune response. A study showed that variants in the IL10 gene are protective against Epstein-Barr infection.
[ref][ref] (More on this in the Genotype Report section below.)
Reactivation of Epstein-Barr Virus:
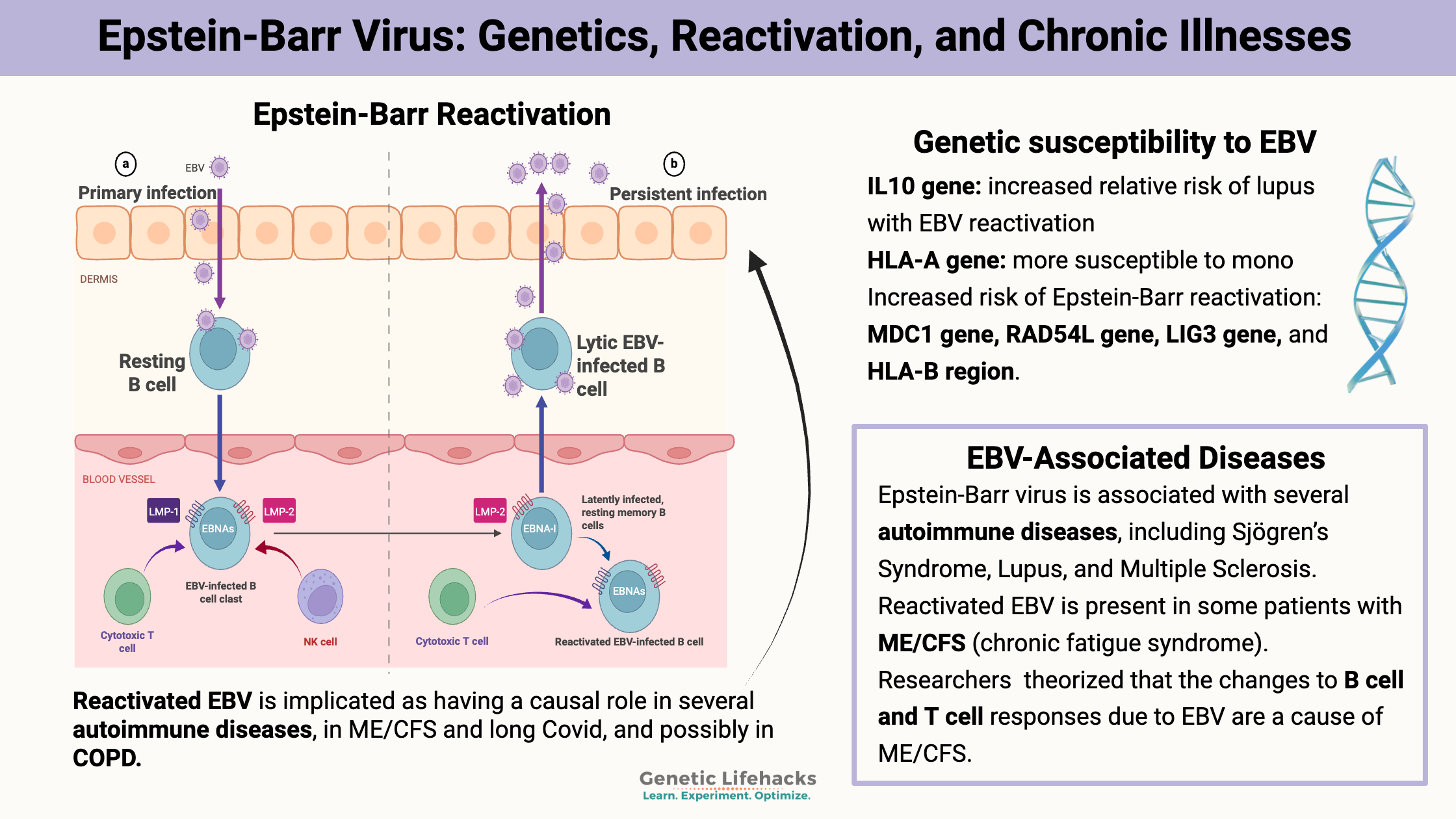
The reactivation of the Epstein-Barr virus moves it from a latent, or dormant, state to an actively replicating one. Reactivated EBV is implicated as having a causal role in several autoimmune diseases, a few types of uncommon cancers, ME/CFS, long Covid, and possibly in COPD.
Let’s take a look at how and why the virus can be reactivated, and then go into the connections with autoimmune diseases and ME/CFS.
Triggers of EBV reactivation:
The reactivation of EBV is regulated by different signalling pathways and can occur under certain conditions, such as hypoxia (lack of oxygen), B-cell receptor activation, reactive oxygen species (ROS) induction, and exposure to certain laboratory chemicals. Additionally, stress, immunosuppression, and certain medications can reactivate the virus. Certain bacteria, including Aggregatibacter actinomycetemcomitans (an oral bacterium associated with periodontitis) and H. pylori, can also trigger reactivation.[ref]
The reactivation cascade starts with the expression of two of the viral proteins: Zta and Rta. These two proteins then promote and boost the transcription of the other viral proteins for replicating the viral genome.
A lot of research focuses on the Zta and Rta proteins, examining how the human immune system keeps them from being activated and looking for ways to stop them once they are activated. Researchers are also studying how to target these proteins as a way of treating epithelial cancers.[ref]
The latent viral genome is methylated, meaning that a methyl group is attached to the DNA to keep it from being translated. The CAF-1 protein complex is involved in the methylation of EBV to keep it latent, and low levels of CAF-1 are associated with EBV reactivation in Burkitt lymphoma cells. Interferon-γ-inducible protein 16 (IFI16) is also involved in preventing EBV reactivation.[ref][ref] IFI16 is also involved in the body’s response to Covid. [ref]
Epstein-Barr and Autoimmune Diseases:
Autoimmune disorders are characterized by the body’s immune system attacking its own cells. Epstein-Barr virus is associated in epidemiological studies with several autoimmune diseases. Research points to multiple possible mechanisms through which EBV increases autoimmunity, including lytic reactivation, immune evasion, and molecular mimicry.[ref]
Sjögren’s Syndrome:
Sjögren’s Syndrome is an autoimmune disease that usually causes a dry mouth, but some people may also experience joint and muscle pain, severe fatigue, and skin issues. The Epstein-Barr virus (EBV) typically infects the salivary glands. For most people, the epithelial cells of the salivary glands serve as a reservoir for the latent virus. Salivary gland biopsies of patients with Sjögren’s often show increased levels of EBV and viral reactivation. These cells have also been shown to express high levels of HLA-DR antigens, suggesting that Sjögren’s may result from persistent EBV infection and an ineffective T-cell response to it[ref]
Related article: Sjögren’s Syndrome: Causes, Genes, Solution
Lupus:
There is also an increased risk of lupus with IgA levels for a specific viral protein in EBV. CD40 genetic variants affect susceptibility to lupus in conjunction with EBV.[ref] A 2025 study showed that EBV-infected B cells can activate helper T cells, which starts a cascade of events leading to the systemic autoimmune response.[ref]
Related article: Lupus: Genetics, Root Causes, and Possible Solutions
Multiple Sclerosis:
Multiple sclerosis (MS) involves inflammation and demyelination of neurons in the brain and spinal cord. A significant amount of research suggests that EBV likely plays a causal role in MS, particularly among most MS patients.
Patients with MS have an altered immunological response to EBV antigens.[ref] The strongest genetic risk factor for MS is having the HLA-DRB1*15:01 serotype, which interacts differently with EBV antibodies. Research also shows an altered anti-EBV T cell response in MS patients.[ref]
Multiple studies have been done on the link between having had mono and later developing MS. Research shows that those with the HLA-DRB1*1501 are at a higher risk of multiple sclerosis, especially if they have had mono.[ref]
A study involving US Army personnel found that the individuals who converted to Epstein-Barr seropositivity (showing they had been infected) were at a 32-fold higher risk of MS diagnosis than seronegative personnel.[ref]
Related article: Multiple Sclerosis: Genetic Factors and Susceptibility to MS
Primary Sclerosing Cholangitis:
A new study suggests that Epstein-Barr infection may be linked to PSC. The study found that patients with PSC were more likely to have Epstein-Barr antibodies in their sampled T and B cells. [ref]
Related article: Primary Sclerosing Cholangitis
Epstein-Barr reactivation in ME/CFS and Long Covid:
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a chronic, debilitating disease affecting approximately 1% of the general population. It is characterized by fatigue that does not improve with sleep and often worsens with physical or mental activity. For many with ME/CFS, the onset is preceded by a viral infection, but for some, the initiating event is a physical trauma.
The theory that chronic fatigue syndrome is due to Epstein-Barr infection first came about in the 1960s. Since then, other viral triggers have been investigated as well, such as cytomegalovirus and HHV. Studies show that some people with ME/CFS have elevated EBV antibodies or EBV reactivation. It is theorized that changes in B and T cell responses due to EBV cause ME/CFS. [ref][ref][ref]
Long Covid or PASC (post-acute sequelae of Covid) involves symptoms, such as fatigue, POTS, brain fog, post-exertional malaise, and shortness of breath, that continue for more than 4 weeks after a Covid infection. For a subset of long Covid patients, Epstein-Barr virus is reactivated, which may be a driving factor in the fatigue and other symptoms. In patients hospitalized for severe Covid, EBV reactivation was found in 82% of the patients. A review of 40 studies on viral reactivation in Covid patients showed that Epstein-Barr virus was the most common, along with cytomegalovirus and HHV-1. [ref][ref] [ref]
Related article: ME/CFS and Long Covid: Causes and Possible Solutions
Epstein-Barr virus and COPD:
COPD (chronic obstructive pulmonary disease) is a progressive lung disease that makes breathing difficult. The two primary conditions under the COPD umbrella are chronic bronchitis and emphysema.
Studies over the past two decades show that a portion of COPD patients have active Epstein-Barr virus. Patients with COPD have periods of stable disease interspersed with times of acute exacerbation, which are characterized by increased sputum production, coughing, and breathing difficulties. Studies on exacerbations show that active bacterial or viral infections are common and that EBV reactivation occurs in some cases. However, active EBV has also been found in the sputum of stable patients who are not experiencing exacerbation. For instance, one study examined sputum samples and detected EBV nucleic acid in approximately half of them (in both COPD exacerbations and stable patients). [ref][ref]
EBV belongs to the herpesvirus family. In lung tissue samples from people with COPD, areas of the small airways with changes and remodeling were associated with the presence of herpesvirus antigens. These localized areas also exhibited an impaired immune response and secretory IgA deficiency. The results showed the presence of EBV in the lung epithelial tissue of 84% of patients with severe COPD, compared to 6% of healthy controls. Cytomegalovirus, another virus in the same family, was found in 36%-54% of the lung samples.[ref]
A recent clinical trial in COPD patients examined the effects of valaciclovir, an antiviral drug used to treat herpes infections, such as cold sores, shingles, and genital herpes. The trial showed that 87% of patients taking valaciclovir experienced a reduction in sputum EBV titer compared to 40% of patients taking a placebo. The conclusion was that larger trials are needed.[ref]
Genetics and the Epstein-Barr Virus:
Genetic variants interact with EBV in a couple of ways. Rare mutations related to decreased immune responses, known as inborn errors of immunity, are associated with an elevated risk of severe mononucleosis. Common variants that alter the immune response or the recognition of viruses can increase or decrease the body’s response to EBV. Additionally, variants in genes related to suppressing DNA replication are linked to an increased risk of viral reactivation.
A 2024 study showed that a variant in the IL-27 receptor (IL27R gene) causes more severe symptoms of active EBV infection, but the same mutation also prevents the reactivation of the virus as a cause of lymphoma or other cancers.[ref]
As mentioned above, different HLA types interact with Epstein-Barr virus. HLA genes encode HLA antigens found on cell surfaces that signal to the immune system which cells are part of the body and which are foreign invaders. Genetic variants in HLA genes, especially HLA-A, are linked to the severity and susceptibility of mononucleosis, as well as the risk of autoimmune diseases resulting from EBV infection.[ref] In addition, a 2025 study found that the HLA-E*01:01 was associated with higher MS risk, but only in people who had had mono.[ref]
The CD36 gene encodes a protein found on the surface of B cells that influences the behavior of other immune cells, such as T cells, in response to pathogens. A genetic variant that alters CD36 increases susceptibility to MS in conjunction with EBV infection.[ref]
A very interesting 2026 study used whole-genome sequencing data to detect the presence of EBV. Looking at the whole-genome sequencing data of over 480,000 people in the UK Biobank, the researchers were able to find Epstein-Barr virus DNA data in almost 10% of the samples. They then looked at how the presence of EBV DNA in the whole genome sequencing data was connected to disease diagnoses in electronic health records. They found that the presence of EBV DNA increased the odds of having Hodgkin lymphoma, rheumatoid arthritis, chronic obstructive pulmonary disease (COPD), and systemic lupus erythematosus.[ref]
Genotype report: EBV
Access this content:
An active subscription is required to access this content.
Lifehacks:
The million-dollar question is, what can you do about EBV reactivation? Below are some possible ways to address it, but keep in mind that the research studies here are mostly in cells or animals and not placebo-controlled clinical trials.
Be sure to talk with your doctor if you need medical advice before starting any supplements.
Testing for reactivation:
Your doctor can order EBV testing for you, or you can order the blood tests on your own in many places. (How to order your own blood tests)
Here are some of the terms used in testing for EBV reactivation:[ref][ref]
EBV nuclear antigen (EBNA): A test for antibodies to EBNA. These antibodies are found 2-4 months after the initial, primary infection and then usually last for the rest of your life. It’s a marker for having had EBV at some point in your life.
Viral capsid antigen (VCA) IgM: The VCA IgM antibodies will show up early on in an EBV infection and may be present during reactivation.
Viral capsid antigen (VCA) IgG: The IgG antibodies present later after the acute infection and can be an indication of reactivation.[ref]
Early antigen (EA): The early antibodies appear in the first three to six months after you get infected with EBV. You may not need this test if you are looking for reactivation.
| Infection Stage | VCA IgM | VCA IgG | Early Antigen | EBNA |
|---|---|---|---|---|
| Acute | + | + | +/- | – |
| Past | – | + | – | + |
| Reactivation | +/- | + | + | + |
Supplements that may help:
Access this content:
An active subscription is required to access this content.
Related articles
Multiple Sclerosis: Genetic Factors and Susceptibility to MS
TNF-alpha: Inflammation, Chronic Diseases, and Genetic Susceptibility
References:
Nyeo, Sherry S., et al. “Population-Scale Sequencing Resolves Determinants of Persistent EBV DNA.” Nature, Jan. 2026, pp. 1–9. www.nature.com, https://doi.org/10.1038/s41586-025-10020-2.