Key takeaways:
~ Seasonal Affective Disorder (SAD) affects 5-10% of the population in higher latitudes.
~ Genetic variants in circadian rhythm and light detection genes are linked to increased susceptibility to SAD.
~ Changing your lighting may help you beat the winter blues.
This article dives into the science of why seasonal affective disorder occurs, which genetic variants increase susceptibility, and the personalized solutions that may work for specific genetic variants. Members will see their genotype report below, plus additional solutions in the Lifehacks section. Join today.
What is Seasonal Affective Disorder?
The Winter Blues… It’s often described as feeling low, generally apathetic, blah, usually accompanied by changes in sleep.
Officially called Seasonal Affective Disorder, the change in mood when the days grow short is a fairly common phenomenon in higher latitudes. It affects 5-10% of some populations.[ref]
Seasonal Affective Disorder (SAD) is characterized by recurrent depression with a change in the season, usually in fall/winter for most people.
Scientists think SAD is due to an aberrant or altered response to light. It could be due to not enough brightness from sunlight or simply not enough hours of light.
SAD is considered to be highly heritable, and studies in twins show that about 50% of the risk is genetic.[ref] What is the other half of the equation here? Daylight exposure is a big one. Chronic inflammation may also increase the risk.
Researchers can determine what causes a problem – the root cause – by finding out which genes enhance the likelihood of a disease or disorder.
Knowing the genes involved can help us understand which biological pathways are involved.
For seasonal affective disorder, research pinpoints many genes that encode circadian rhythm proteins.[ref]
Circadian rhythm and SAD:
Our circadian rhythm is controlled by genes triggered by light hitting the retina of our eyes.
During the daytime, light in the blue spectrum hits specific receptors in the retina and shuts off melatonin production from the pineal gland. This process occurs when blue light hits a specific receptor (OPN4), triggering a signal to the brain to stop melatonin from being produced.[ref]
At night, the lack of light in the blue wavelengths allows melatonin levels to rise again.
Both the suppression of melatonin during daylight via exposure to bright light and the rise of melatonin at night due to darkness are integral to mental and physical health.
The lack of light during the daytime may affect seasonal depression by not shutting off melatonin production enough during the day.[ref]
Interestingly, some genes associated with SAD also overlap with genetic variants that increase susceptibility to bipolar disorder and schizophrenia but not other depressive disorders.[ref] For many, bipolar disorder is linked to circadian rhythm disruption.
Related article: Circadian rhythm genes and bipolar disorder
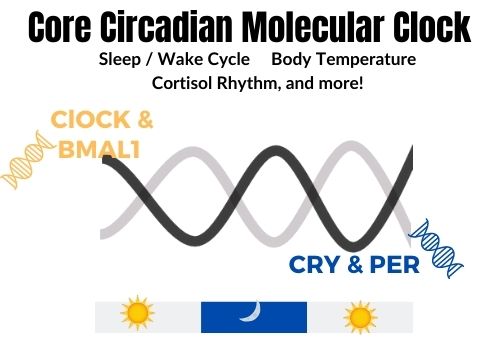
The core circadian clock genes include a pair of genes (CLOCK and BMAL1) active together during the daytime and another pair of genes (PER and CRY) active during the nighttime.
The rise and fall of these genes create a 24-hour molecular clock that governs many cellular functions throughout the body.
Messing up your circadian rhythm makes you feel bad…
If you have ever traveled across several time zones, you know that jetlag can make you feel a bit wretched for a day or two. For me, jetlag makes me feel disoriented, grumpy, and unable to think clearly.
The feelings of jetlag are due to your circadian clock being out of sync with your environment. Your body thinks it is midnight, but your eyes know that the sun is up and shining brightly.
When your circadian rhythm is disrupted — whether from travel or staying up late, or changing light — the result can cause physiological changes in how your body feels and your mind works.
Serotonin and SAD:
You may be wondering, but what about serotonin? Everyone thinks of serotonin for depression due to the popularity of SSRIs as antidepressant drugs.
Several studies for seasonal affective disorder have looked into the link to serotonin. While most of the studies didn’t find a significant link to serotonin genes, the way serotonin is used in the brain may play a role in SAD.[ref][ref][ref] For example, certain behaviors linked with seasonal depression, such as overeating, may be related to serotonin.[ref]
Interestingly, a couple of studies have found that a serotonin receptor, HTR2A, is significantly associated with seasonal depression in both winter and summer. This receptor involves memory, mood, cognition, appetite, anxiety, perception, sleep, thermoregulation, and vasoconstriction. It is activated by serotonin, LSD, psilocybin, and DMT.
Related article: Serotonin receptor 2A genetic variants
Is there a SAD gene?
While genes do play a major role in increasing the risk of SAD, there is not one specific gene mutation that causes seasonal affective disorder.
Instead, multiple genetic variants add to the risk, along with latitude, length of daylight, and possibly dietary factors.
Additionally, seasonal changes occur in most mammals to neurotransmitter levels.
Monoamine Oxidase (MAO-A) Levels change seasonally
MAO-A is an enzyme that breaks down neurotransmitters, and changes in MAO-A levels are linked to depressive disorders.
Recently, researchers discovered that most people normally have a seasonal change in MAO-A levels in the fall and winter. But people with SAD don’t have that normal, seasonal rhythm to MAO-A levels. Important here, the researchers also found that bright light therapy restored the normal MAO-A seasonal dynamics.[ref]
Seasonal Affective Disorder Genotype Report
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Lifehacks for Seasonal Affective Disorder
First and foremost: going outside first thing in the morning may help if you live at a middle latitude. The morning sun is powerful in resetting your circadian rhythm.
Both light and dark are important:
Light Boxes for Full Spectrum Light:
If you can’t get outside for enough sunlight during the daylight hours for whatever reason (working, living too far north, etc.), there are full-spectrum lights made specifically for SAD. Studies have found 30 minutes of 10000 lux in the early morning effective.
New studies show that narrow-spectrum blue light (100 lux) may be as effective as bright full-wavelength light (10,000 lux).[ref][ref]
Putting a blue light in your ear may sound a bit ‘out there’, but there are a few studies that indicate this might just be something worth trying. A clinical trial of transcranial blue light through the ear canal reduced depression by half in more than 75% of participants.[ref] (I’m not sure how great this clinical trial is, though, since there is no sham or control group, just comparisons of different light strengths.) Transcranial light isn’t as crazy as it seems. Animal studies have shown that extra-ocular light (i.e., through the ear canal) has an effect on the brain. Birds are known to have photoreceptors in their brains that regulate seasonal reproduction.[ref] Sunlight through the skull induces GABA release in rats.[ref]
Sleep in the dark:
A mouse study looking at the effect of dim light at night found that for mice lacking in PER3 (similar to the above genetic variants), dim light at night caused an anhedonia-like effect.[ref]
Anhedonia is the loss of pleasure or interest in things, feeling blah. Nighttime light exposure has become an enormous problem worldwide, with far-reaching health effects on people and animals. If you have PER3 genetic variants (or even if you don’t!), blocking light at night is essential for healthy sleep.
Blackout curtains are not that expensive, and you can block all the little LED lights from chargers, etc., by just putting a piece of dark tape over them.
One huge change we all face in our modern times is large amounts of blue light at night from TVs, tablets, and cell phones. Turning off electronics an hour before bedtime is helpful for naturally increasing melatonin production at night. Alternatively, blue-light-blocking glasses that eliminate 100% of light in the blue wavelengths may also help improve sleep.
Dietary links to seasonal affective disorder:
Related Articles and Topics:
Serotonin: Genetic variants that impact serotonin levels and serotonin receptors
Serotonin is a neurotransmitter that is important in depression, sleep, and many other aspects of health. Learn how your genetic variants in the serotonin receptor genes impact their function.
COMT Gene: Neurotransmitters, estrogen metabolism, and more
Wondering why your neurotransmitters are out of balance? It could be due to your COMT genetic variants. The COMT gene codes for the enzyme catechol-O-methyltransferase, which breaks down (metabolizes) the neurotransmitters dopamine, epinephrine, and norepinephrine.
References:
Benedetti, Francesco, et al. “Actimetric Evidence That CLOCK 3111 T/C SNP Influences Sleep and Activity Patterns in Patients Affected by Bipolar Depression.” American Journal of Medical Genetics. Part B, Neuropsychiatric Genetics: The Official Publication of the International Society of Psychiatric Genetics, vol. 144B, no. 5, July 2007, pp. 631–35. PubMed, https://doi.org/10.1002/ajmg.b.30475.
Blume, Christine, et al. “Effects of Light on Human Circadian Rhythms, Sleep and Mood.” Somnologie, vol. 23, no. 3, 2019, pp. 147–56. PubMed Central, https://doi.org/10.1007/s11818-019-00215-x.
De Crescenzo, F., et al. “Melatonin as a Treatment for Mood Disorders: A Systematic Review.” Acta Psychiatrica Scandinavica, vol. 136, no. 6, Dec. 2017, pp. 549–58. PubMed, https://doi.org/10.1111/acps.12755.
Hida, Akiko, et al. “Screening of Clock Gene Polymorphisms Demonstrates Association of a PER3 Polymorphism with Morningness-Eveningness Preference and Circadian Rhythm Sleep Disorder.” Scientific Reports, vol. 4, Sept. 2014, p. 6309. PubMed, https://doi.org/10.1038/srep06309.
Jang, K. L., et al. “Gender Differences in the Heritability of Seasonal Mood Change.” Psychiatry Research, vol. 70, no. 3, May 1997, pp. 145–54. PubMed, https://doi.org/10.1016/s0165-1781(97)00030-9.
Johansson, C., et al. “The Serotonin Transporter Promoter Repeat Length Polymorphism, Seasonal Affective Disorder and Seasonality.” Psychological Medicine, vol. 33, no. 5, July 2003, pp. 785–92. PubMed, https://doi.org/10.1017/s0033291703007372.
Johansson, Carolina, et al. “Circadian Clock-Related Polymorphisms in Seasonal Affective Disorder and Their Relevance to Diurnal Preference.” Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology, vol. 28, no. 4, Apr. 2003, pp. 734–39. PubMed, https://doi.org/10.1038/sj.npp.1300121.
Jones, Samuel E., et al. “Genome-Wide Association Analyses of Chronotype in 697,828 Individuals Provides Insights into Circadian Rhythms.” Nature Communications, vol. 10, no. 1, Jan. 2019, p. 343. PubMed, https://doi.org/10.1038/s41467-018-08259-7.
Kalbitzer, Jan, et al. “Seasonal Changes in Brain Serotonin Transporter Binding in Short Serotonin Transporter Linked Polymorphic Region-Allele Carriers but Not in Long-Allele Homozygotes.” Biological Psychiatry, vol. 67, no. 11, June 2010, pp. 1033–39. PubMed, https://doi.org/10.1016/j.biopsych.2009.11.027.
Kim, Hae-In, et al. “Association of CLOCK, ARNTL, and NPAS2 Gene Polymorphisms and Seasonal Variations in Mood and Behavior.” Chronobiology International, vol. 32, no. 6, 2015, pp. 785–91. PubMed, https://doi.org/10.3109/07420528.2015.1049613.
Kripke, Daniel F., et al. “Circadian Polymorphisms Associated with Affective Disorders.” Journal of Circadian Rhythms, vol. 7, Jan. 2009, p. 2. PubMed Central, https://doi.org/10.1186/1740-3391-7-2.
Lee, Sang-il, et al. “Association between Melanopsin Gene Polymorphism (I394T) and Pupillary Light Reflex Is Dependent on Light Wavelength.” Journal of Physiological Anthropology, vol. 32, no. 1, Oct. 2013, p. 16. PubMed Central, https://doi.org/10.1186/1880-6805-32-16.
Lee, Sang-Il, et al. “Association between the Melanopsin Gene Polymorphism OPN4*Ile394Thr and Sleep/Wake Timing in Japanese University Students.” Journal of Physiological Anthropology, vol. 33, May 2014, p. 9. PubMed, https://doi.org/10.1186/1880-6805-33-9.
Liberman, Amanda R., et al. “Circadian Clock Model Supports Molecular Link Between PER3 and Human Anxiety.” Scientific Reports, vol. 7, Aug. 2017, p. 9893. PubMed Central, https://doi.org/10.1038/s41598-017-07957-4.
Martynhak, Bruno Jacson, et al. “Transient Anhedonia Phenotype and Altered Circadian Timing of Behaviour during Night-Time Dim Light Exposure in Per3−/− Mice, but Not Wildtype Mice.” Scientific Reports, vol. 7, Jan. 2017, p. 40399. PubMed Central, https://doi.org/10.1038/srep40399.
McClung, Colleen A. “Circadian Rhythms and Mood Regulation: Insights from Pre-Clinical Models.” European Neuropsychopharmacology : The Journal of the European College of Neuropsychopharmacology, vol. 21, no. Suppl 4, Sept. 2011, pp. S683–93. PubMed Central, https://doi.org/10.1016/j.euroneuro.2011.07.008.
Meesters, Alie N. R., et al. “Is There a Relationship between Vegetarianism and Seasonal Affective Disorder? A Pilot Study.” Neuropsychobiology, vol. 74, no. 4, 2016, pp. 202–06. PubMed, https://doi.org/10.1159/000477247.
Meesters, Ybe, et al. “The Effects of Low-Intensity Narrow-Band Blue-Light Treatment Compared to Bright White-Light Treatment in Seasonal Affective Disorder.” Journal of Affective Disorders, vol. 232, May 2018, pp. 48–51. PubMed, https://doi.org/10.1016/j.jad.2018.01.024.
Nakane, Yusuke, et al. “A Mammalian Neural Tissue Opsin (Opsin 5) Is a Deep Brain Photoreceptor in Birds.” Proceedings of the National Academy of Sciences of the United States of America, vol. 107, no. 34, Aug. 2010, pp. 15264–68. PubMed, https://doi.org/10.1073/pnas.1006393107.
Partonen, Timo, et al. “Three Circadian Clock Genes Per2, Arntl, and Npas2 Contribute to Winter Depression.” Annals of Medicine, vol. 39, no. 3, 2007, pp. 229–38. PubMed, https://doi.org/10.1080/07853890701278795.
Pjrek, Edda, et al. “Serum Lipid Levels in Seasonal Affective Disorder.” European Archives of Psychiatry and Clinical Neuroscience, vol. 257, no. 4, June 2007, pp. 197–202. PubMed, https://doi.org/10.1007/s00406-006-0706-y.
Praschak-Rieder, Nicole, et al. “A Cys 23-Ser 23 Substitution in the 5-HT(2C) Receptor Gene Influences Body Weight Regulation in Females with Seasonal Affective Disorder: An Austrian-Canadian Collaborative Study.” Journal of Psychiatric Research, vol. 39, no. 6, Nov. 2005, pp. 561–67. PubMed, https://doi.org/10.1016/j.jpsychires.2005.01.007.
Roecklein, Kathryn, et al. “The Post Illumination Pupil Response Is Reduced in Seasonal Affective Disorder.” Psychiatry Research, vol. 210, no. 1, Nov. 2013, pp. 150–58. PubMed, https://doi.org/10.1016/j.psychres.2013.05.023.
Roecklein, Kathryn A., Kelly J. Rohan, et al. “A Missense Variant (P10L) of the Melanopsin (OPN4) Gene in Seasonal Affective Disorder.” Journal of Affective Disorders, vol. 114, no. 1–3, Apr. 2009, pp. 279–85. PubMed, https://doi.org/10.1016/j.jad.2008.08.005.
Roecklein, Kathryn A., Patricia M. Wong, et al. “Melanopsin Gene Variations Interact With Season to Predict Sleep Onset and Chronotype.” Chronobiology International, vol. 29, no. 8, Oct. 2012, pp. 1036–47. PubMed Central, https://doi.org/10.3109/07420528.2012.706766.
Spies, Marie, et al. “Brain Monoamine Oxidase A in Seasonal Affective Disorder and Treatment with Bright Light Therapy.” Translational Psychiatry, vol. 8, Sept. 2018, p. 198. PubMed Central, https://doi.org/10.1038/s41398-018-0227-2.
Turco, M., et al. “Diurnal Preference, Mood and the Response to Morning Light in Relation to Polymorphisms in the Human Clock Gene PER3.” Scientific Reports, vol. 7, no. 1, July 2017, p. 6967. PubMed, https://doi.org/10.1038/s41598-017-06769-w.
van Strater, A. C. P., and P. F. Bouvy. “[Omega-3 fatty acids in the treatment of affective disorders: an overview of the literature].” Tijdschrift Voor Psychiatrie, vol. 49, no. 2, 2007, pp. 85–94.
Wade, P. D., et al. “Mammalian Cerebral Cortical Tissue Responds to Low-Intensity Visible Light.” Proceedings of the National Academy of Sciences of the United States of America, vol. 85, no. 23, Dec. 1988, pp. 9322–26. PubMed, https://doi.org/10.1073/pnas.85.23.9322.
Wescott, Delainey L., et al. “Sleep in Seasonal Affective Disorder.” Current Opinion in Psychology, vol. 34, Aug. 2020, pp. 7–11. PubMed Central, https://doi.org/10.1016/j.copsyc.2019.08.023.
Willeit, Matthäus, et al. “Enhanced Serotonin Transporter Function during Depression in Seasonal Affective Disorder.” Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology, vol. 33, no. 7, June 2008, pp. 1503–13. PubMed, https://doi.org/10.1038/sj.npp.1301560.
Yang, C., et al. “The Effects of Illuminance and Correlated Colour Temperature on Daytime Melatonin Levels in Undergraduates with Sub-Syndromal SAD.” Lighting Research & Technology, vol. 52, no. 6, Oct. 2020, pp. 722–35. DOI.org (Crossref), https://doi.org/10.1177/1477153519884097.
Zhang, Luoying, et al. “A PERIOD3 Variant Causes a Circadian Phenotype and Is Associated with a Seasonal Mood Trait.” Proceedings of the National Academy of Sciences of the United States of America, vol. 113, no. 11, Mar. 2016, pp. E1536–44. PubMed Central, https://doi.org/10.1073/pnas.1600039113.