Key takeaways:
~ PMS and PMDD impact the quality of life for about a third of women.
~ Genetic studies show that the heritability, or genetic component, of PMS is around 95%.
~ Importantly, there are research-backed, natural supplements and diet options to help mitigate PMS.
Premenstrual syndrome and premenstrual dysphoric disorder:
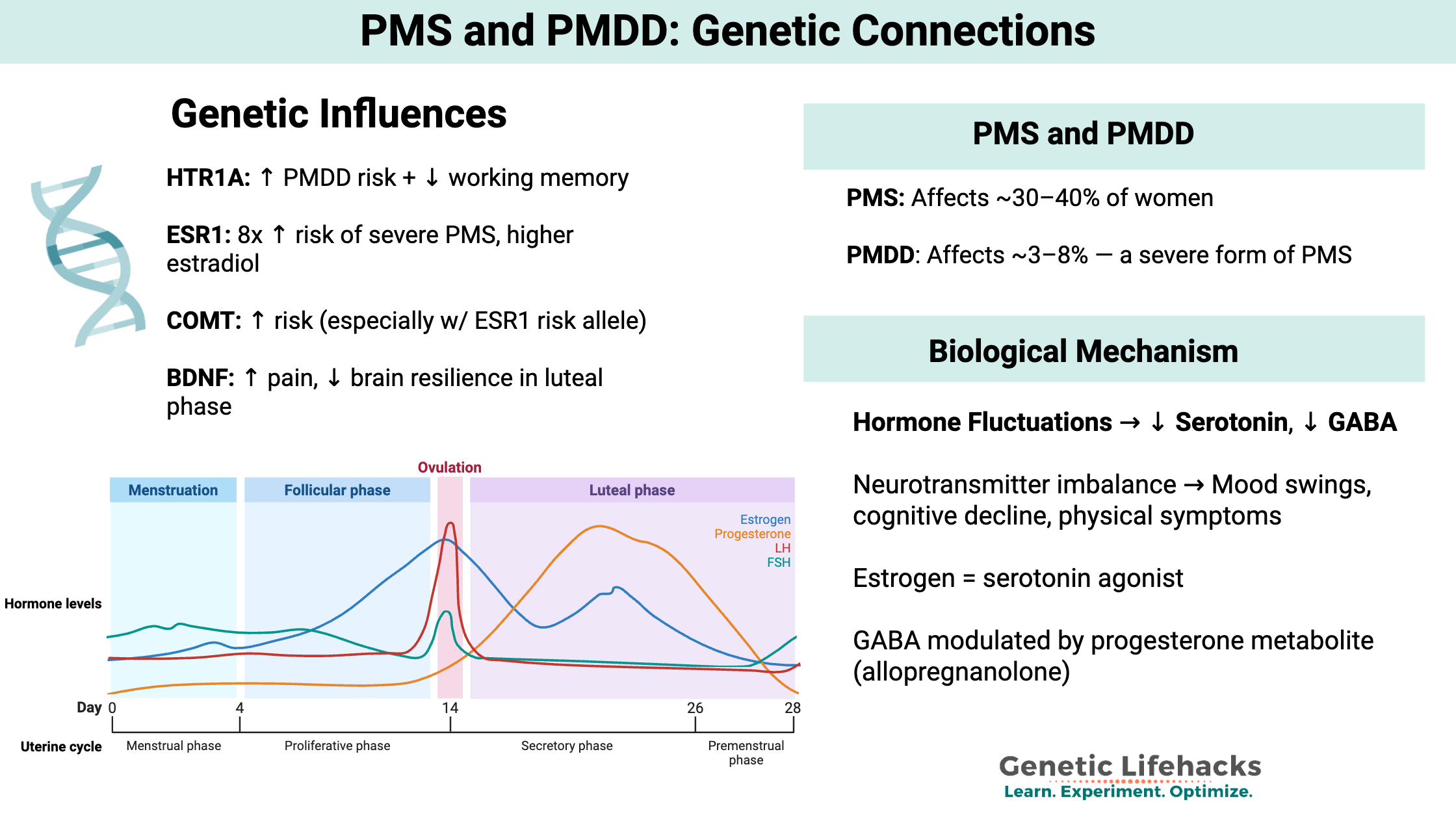
Premenstrual syndrome (PMS) is defined clinically as a condition occurring during the luteal phase of the menstrual cycle (before your period), causing physical and mood symptoms. Experts believe that PMS is caused by hormonal fluctuations during this phase of the menstrual cycle, possibly in combination with nutrient deficiencies.[ref]
Premenstrual dysphoric disorder (PMDD) is also called late luteal dysphoric disorder. It is a severe form of PMS that severely impacts quality of life.
PMS affects about 30-40% of women, while the rarer PMDD affects only 3-8%.[ref]
What role do genes play in PMS?
Research shows that there is a very strong genetic component to PMS, especially for a severe form of PMS called premenstrual dysphoric disorder (PMDD).
A 2011 study of twins estimated the heritability of PMS to be around 95%.[ref]
Serotonin Receptor Gene: HTR1A
The HTR1A gene codes for a serotonin receptor found mainly in the brain. Variants in the gene are linked to reduced serotonin neurotransmission. One study found that an HTR1A variant was “associated with impaired WM [working memory] in the premenstrual phase and premenstrual decline of cognitive function.” The variant is also associated with an increased risk of PMDD. [ref][ref]
Estrogen Receptor 1 gene: ESR1
ESR1 mediates estrogen activity in the brain. This estrogen receptor is the key to how changing estrogen levels cause changes in the transcription of many other genes. In the brain, ESR1 is involved in cognitive function, emotions, and memory. Variants in ESR1 are associated with severe PMS, breast cancer, osteoporosis, and endometriosis. ESR1 has also been studied in relation to cognitive impairment and Alzheimer’s Disease.[ref][ref]
BDNF gene:
Brain-derived neurotrophic factor (BDNF) is a protein that promotes nerve function and interacts with serotonin and dopamine in the brain. A common BDNF variant that decreases BDNF levels is linked to increased pain in PMS.[ref] Another study showed the same variant led to lower fronto-cingulate cortex activation in the luteal phase in women with PMDD.[ref]
Is it all in your head?
In a literal way… It turns out that neurotransmitters directly cause some of the symptoms of PMS and PMDD. Both conditions are linked to physically altered neurotransmitter levels.
- Serotonin is an important neurotransmitter involved in mood stability. Estrogen is a serotonin agonist, and fluctuations in estrogen levels therefore affect serotonin levels.
- GABA, another neurotransmitter, is also involved in PMS symptoms for some.[ref]
Increased susceptibility to PMS and PMDD is linked to genetic variants in these neurotransmitter genes — and these genes may hold the clues to what to do about PMS symptoms.
PMS and PMDD Genotype Report:
Lifehacks: Natural solutions for PMS and PMDD
Genetics seems to play a bigger role in PMDD. For many of us, though, we may need to look further for solutions to PMS woes.
Research on Dietary Interventions:
Watch for overeating:
Unsurprisingly, a study found that women with PMDD tend to eat more right before their period.[ref]
Eat healthy the week before your period:
Studies on different dietary patterns show that a standard Western diet with fast food, deli meats, and soda increases the symptoms of PMS considerably. If you eat a lot of fast food or junk food, cleaning up your diet and eating more whole foods, especially in the week before your period, may help considerably.[ref] Plan ahead on this so that you are prepared for cooking meals at home and have healthy options on hand.
Intermittent fasting or time-restricted eating:
Intermittent fasting or simply having a longer overnight fasting period may help with luteal phase cortisol levels.[ref] An example of this could be eating dinner earlier (by 6 pm) and not eating again until 9 am. This would give you an overnight fast of 15 hours.
Histamine intolerance and a low histamine diet:
PMS, especially for menstrual cramps, is closely linked to a high histamine burden. If the symptoms of histamine intolerance seem to fit you, a diet lower in histamines may help your PMS. Foods high in histamines (avoid for a low histamine diet) include anything fermented (soy sauce, vinegar, wine, kombucha), lunch meats, tomatoes, oranges, strawberries, chocolate, and fish that is not completely fresh. You may find that eating a lower histamine diet in the week prior to your period may be enough to help with your symptoms.
Related article: Genetics and Histamine Intolerance
6 Natural Supplements backed by research for PMS:
Related Article and Topics: