Key takeaways:
~ Vitamin K is an essential cofactor for reactions that turn on vitamin K-dependent (VKD) proteins.
~ VKD proteins are important in blood clotting, bone health, and calcium regulation.
~ Low vitamin K levels can increase the risk of osteoporosis, vascular calcification, heart valve calcification, and vascular dementia.
~ Genetic variants related to vitamin K can impact your need for more vitamin K and your response to warfarin.
Vitamin K Genes: Clotting, Bone Health, and Calcium Regulation
Vitamin K is one of those vitamins that doesn’t get a lot of press. You may have heard of it in the context of preventing osteoporosis, but it turns out that this lesser-known vitamin can have a big impact on your overall health as you age.
There are a couple of forms of Vitamin K:
Vitamin K1
Vitamin K1, also known as phylloquinone, is a fat-soluble vitamin that the body needs in order to synthesize the proteins responsible for blood coagulation.
Vitamin K2
Vitamin K2, also known as menaquinone, is found in in several different forms (MK-4, MK-7, MK-8, MK-10). It helps maintain bone strength. Additionally, higher levels of K2 help regulate calcium. Vitamin K2 has been shown to reduce calcification in the arteries[ref], as well as possibly play a role in mitochondrial function.[ref]
All of these different forms of vitamin K share a common structure at their core, 2-methyl-1,4-naphthoquinone, and cells can convert K1 to K2.
What does vitamin K do?
Vitamin K is an essential cofactor for reactions involving the enzyme gamma-glutamyl carboxylase, which is also called vitamin K carboxylase.
These enzyme-catalyzed reactions activate VKD (vitamin K-dependent) proteins.[ref]
Vitamin K-dependent proteins include:[ref][ref]
| Coagulation: Factors II, VII, IX, and X Prothrombin |
| Anticoagulation: Proteins C, S, and Z |
| Others: |
| Matrix Gla protein (extracellular matrix, inhibits calcification of tissue) |
| Osteocalcin (bone hormone) |
| GAS6 protein (growth factor) |
| TGF‐β–inducible protein |
| Periostin (osteoblastic-specific factor 2, growth and repair of connective tissues) |
| Proline‐rich Gla proteins 1–4 (receptors involved in signaling pathways) |
| Inter-alpha-trypsin inhibitor heavy chain H2 (ITIH2) |
| Transmembrane Gla proteins 3 and 4 |
| Gla-rich protein (modulator of tissue calcification, anti-inflammatory) |
| Nephrocalcin (inhibits calcium kidney stones) |
Vitamin K is essential for many different biological processes, but we only get small amounts from food and it’s not stored for long in the body. Instead, vitamin K is recycled and reused multiple times in reactions.
Symptoms of vitamin K deficiency:[ref]
- Easy bruising
- Nose bleeds, bleeding gums
- Extremely heavy menstrual bleeding
Let’s take a look at the roles of vitamin K in processes throughout the body and in long-term health.
Bone Health:
Low vitamin K levels have long been associated with a higher risk of osteoporosis.[ref] A study that followed 72,000 women for 10 years found that women whose phylloquinone (K1) intake was less than 109 mcg/day had a 30% higher risk of hip fracture. Another study of older adults found that those with the highest quartile of vitamin K intake (254 mcg/day) had a 65% lower risk of hip fracture.[ref]
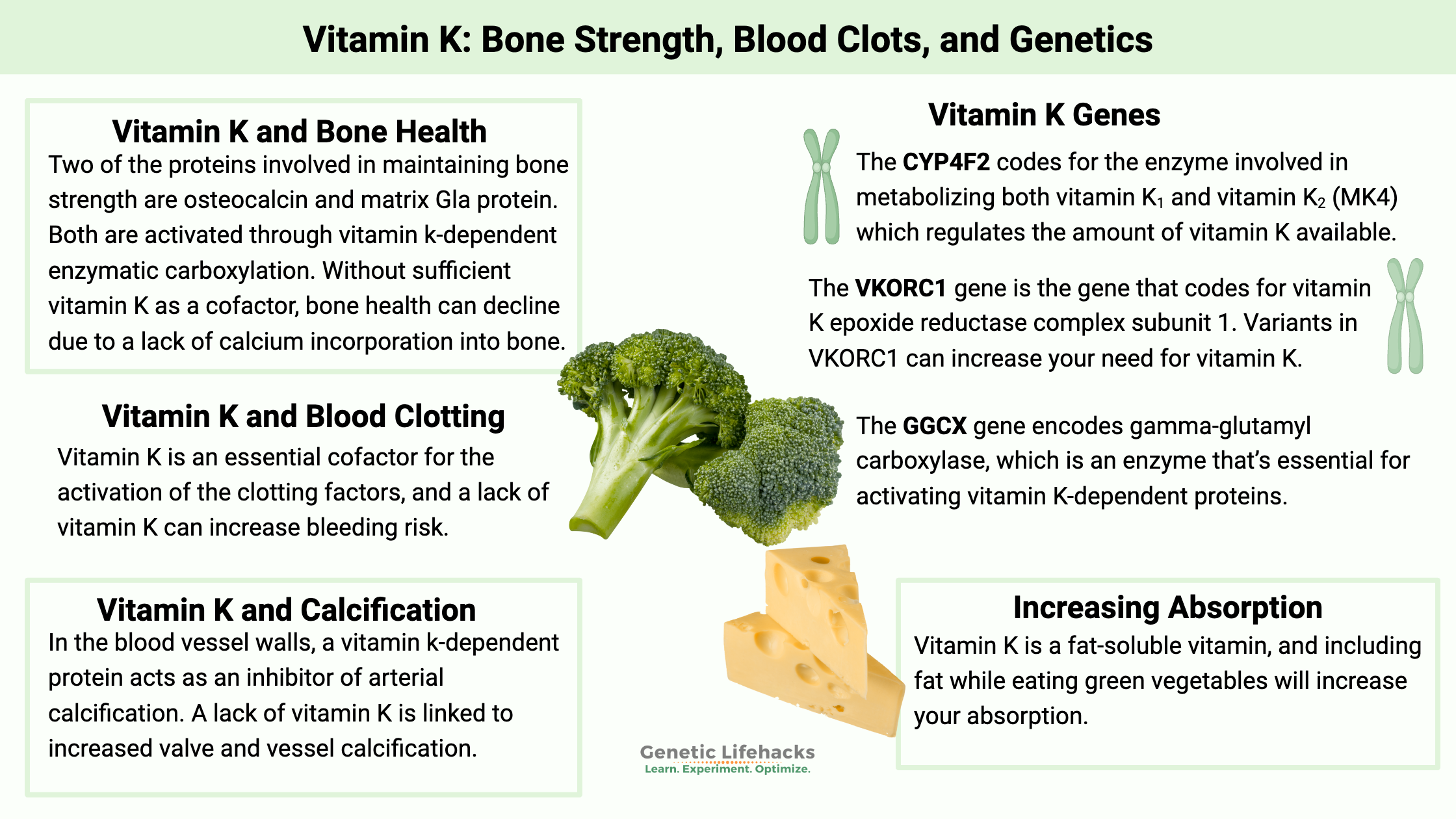
Two of the proteins involved in maintaining bone strength are osteocalcin and matrix Gla protein. Both are activated through vitamin k-dependent enzymatic carboxylation. Without sufficient vitamin K as a cofactor, bone health can decline due to a lack of calcium incorporation into bone. In addition, vitamin K can also inhibit osteoclasts, which break down bone. Thus, vitamin K has two important roles in long-term bone health.[ref][ref]
Blood Clotting:
Blood clots are formed by what is called the coagulation cascade, which is a series of steps or reactions in response to an injury that results in a blood clot. Vitamin K is involved in the post-translational modification of 7 different proteins involved in the clotting cascade.[ref]
The coagulation cascade involves both clotting factors, such as Factor II and Factor VIII, as well as natural anti-clotting agents that control the amount of clotting. Vitamin K is an essential cofactor for the activation of the clotting factors, and a lack of vitamin K can increase the risk of bleeding.[ref]
Related article: Genetic variants that increase blood clot risks
Calcification of the arteries and heart:
While the best-known VKD proteins are involved in blood clotting, recent research has shed a lot of light on VKD proteins and the importance of vitamin K in preventing vascular calcification and apoptosis.[ref] The elasticity of the walls of the arteries is extremely important for expanding and contracting with each heartbeat. If the artery is stiff, more pressure is required, raising blood pressure.
As mentioned above with bone health, matrix Gla protein is dependent on vitamin K for activation. In the blood vessel walls, activated matrix Gla protein acts as an inhibitor of arterial calcification.[ref] Animal studies show how important matrix Gla protein is in the arteries. When there is a deficiency of active matrix Gla protein, animals die within weeks of birth due to arterial calcification.[ref]
A meta-analysis looked at the connection between vitamin K and vascular health. They included 13 controlled clinical trials using K1 at 500–2000 μg/day or MK7 at 90–180 μg/day as supplementation for 6-36 months. The results showed that vitamin K supplementation reduced vascular calcification by 9% by affecting matrix Gla protein.[ref] However, a recent clinical trial showed that MK-4 supplementation (45 mg/day) was not able to reverse coronary artery calcification after 12 months.[ref] More studies are needed to know which type of vitamin K is best for reversing calcification.
Long-term warfarin use causes calcification:
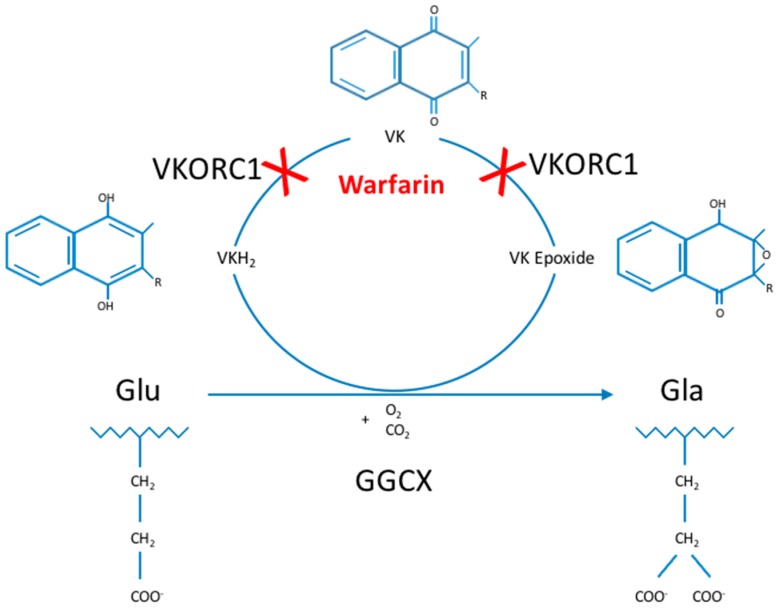
As a VKOR1 inhibitor, warfarin not only reduces blood clots, but it also affects the activation of matrix Gla protein, which inhibits tissue calcification. Animal studies show that either a lack of matrix Gla protein or the use of warfarin can cause cardiovascular calcification, suggesting that the lack of activation of matrix Gla protein by vitamin K is the cause of calcification. Of note, the addition of vitamin D increased calcification in the animal studies.
Human studies show that long-term warfarin therapy increases coronary calcium scores and also causes calcification of the heart valves. For example, warfarin treatment is associated with a 71% increased relative risk of mitral valve calcification.[ref][ref]
For someone not on warfarin, the effect seems to be similar to a long-term vitamin K insufficiency. For example, people with chronic kidney disease often have vitamin K deficiency due to impaired absorption and dietary restrictions. Similar to long-term warfarin use, chronic kidney disease is also associated with a high risk of atherosclerosis and heart valve calcification.[ref]
Cognitive function in aging and risk of dementia:
Higher levels of vitamin K (MK4) in the brain are associated with better cognitive function in aging individuals. Similarly, higher plasma vitamin K1 levels are also associated with better cognitive function and a slower rate of cognitive decline in the elderly. A lower vitamin K level in the brain increases the relative risk of dementia by about 20%.[ref]
Another study looked at biomarkers of vitamin K levels and found that older adults (average age of 75) with the lowest quartile of the vitamin K biomarker had a 65% increased risk of impaired cognitive function.[ref]
Long-term warfarin use and dementia:
Again, the warfarin studies can give us a picture of what decreased vitamin K levels can cause. Looking at people with atrial fibrillation and comparing those on vitamin K antagonists (e.g. warfarin) to other types of anticoagulants, researchers found that those taking vitamin K antagonists had a 10% higher rate of dementia.[ref]
Mitochondrial function, antioxidant:
The role of K2 in mitochondrial function is still being determined, but it acts as an intercellular antioxidant by reducing the production of superoxide, which is a mitochondrial reactive oxygen species. Under certain circumstances, vitamin K along with vitamin C can also act as an electron carrier in the electron transport chain that produces ATP in the mitochondria.[ref][ref][ref]
Male infertility:
Calcium signaling is also essential for sperm maturation. A genetic variant in the GGCX gene, which recycles vitamin K, is associated with an increased risk of male infertility.[ref] A study involving an antioxidant supplement that contained vitamin K along with other vitamins showed that it improved sperm parameters and sperm function.[ref]
Vitamin K Genes:
There are several genes that affect vitamin K – from the conversion of different forms to the recycling of vitamin K back to the active form. Genetic variants in these genes can affect your body’s natural levels of vitamin K, and these variants are also very important for getting the right dose of warfarin, an anticoagulant that works by blocking vitamin K recycling.
CYP4F2 gene:
The CYP4F2 codes for the enzyme involved in converting both vitamin K1 and vitamin K2 (MK-4) to oxidized forms that can be excreted. This is one way the body regulates the amount of vitamin K available.[ref]
Genetic variation in the CYP4F2 gene causes people to naturally have higher or lower levels of vitamin K available, which can affect blood clotting. CYP4F2 regulates the amount of vitamin K in the body, and genetic variants that slow down the CYP4F2 enzyme can cause higher circulating levels of vitamin K (depending on dietary intake).[ref] CYP4F2 also helps break down certain omega-6 fatty acids and vitamin E, so it also plays an important role in regulating the body’s inflammatory response.
VKORC1 Gene:
VKORC1 is the gene that codes for vitamin K epoxide reductase complex subunit 1 – VKORC1 enzyme. VKORC1 is responsible for reducing (in the redox sense) vitamin K from food. The reduced form is then used in vitamin K-dependent reactions. The enzyme also is needed for a second reduction into hydroquinone. All of this then forms a cycle where vitamin K is able to be recycled and reused. [ref][ref][ref]
The anticoagulant warfarin acts on VKORC1, preventing it from recycling vitamin K and thus reducing the amount of vitamin K available for the clotting cascade and reducing the risk of a blood clot. Variants in the VKORC1 gene play a role in the amount of Warfarin that is needed.
GGCX gene:
The GGCX gene encodes gamma-glutamyl carboxylase, which is an enzyme that’s essential for activating vitamin K-dependent proteins. Essentially, this enzyme activates VKD proteins through a process called carboxylation.
INR (internal normalized ratio) is a measure of how long it takes blood to clot, and an elevated INR means that you don’t clot as quickly. This is something that is measured regularly for people on warfarin. Genetic variants that reduce the GGCX gene function have elevated INRs even when they aren’t on warfarin or another vitamin K antagonist.[ref] GGCX knockout mice (no GGCX function) usually die at birth from internal hemorrhaging.[ref]
Rare genetic variants that cause significant changes to GGCX cause a genetic disease called vitamin K-dependent coagulation factor deficiency (VKCFD1). Depending on the mutation, individuals can have mild to moderate bleeding problems, skeletal changes, or cardiac abnormalities. Other GGCX mutations can also cause elastic fiber mineralization which leads to loss of skin elasticity.[ref]
UBIAD1 gene:
Identified in 2010, the UBIAD1 gene encodes an enzyme involved in the biosynthesis of MK-4 as well as CoQ10, and vitamin E. Rare mutations in UBIAD1 are linked to Schnyder crystalline corneal dystrophy which causes clouding of the cornea. [ref][ref]
Vitamin K Genotype Report
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Lifehacks:
The recommended adequate intake for vitamin K is 120 mcg/day for adult males and 90 mcg/day for adult females.[ref] Of note here, a large study in women showed that a daily intake of less than 109 mcg/day increased hip fracture risk.[ref] So 90 mcg/day may be “adequate” to prevent bleeding but not enough to have optimal bone health for women as they age.
Getting vitamin K from foods:
Phylloquinone, or K1, is a part of the photosynthesis process in plants. This makes green plants a good source of vitamin K1.[ref]
Vitamin K2 in the diet is found in the MK4, MK9, MK8, and MK-7 forms. About 10% of dietary vitamin K is in this form in Western diets from aged cheese, pasture-raised eggs, grass-fed dairy, and organ meat. The traditional Japanese fermented soy product, natto, contains the highest amount of vitamin K2. [ref]
In addition, we can convert a small amount of K1 to vitamin K2 in the body. Plus, our gut microbiome produces some K2 for us.
Include fat for better absorption:
Vitamin K is a fat-soluble vitamin, and including fat while eating green vegetables will increase your absorption.
Medications that block vitamin K absorption and conversion:
The absorption in the intestines uses several different receptors, including NPC1L1, which also transports cholesterol and vitamin E. If you’re taking ezetimibe (Zetia) for reducing cholesterol, the drug works by blocking NPC1L1-mediated cholesterol uptake. The drug also also inhibits vitamin K uptake.[ref]
Statins block the pathway for cholesterol synthesis. That same pathway is involved in the conversion of vitamin K1 to the MK4 version of vitamin K2. Animal studies show that atorvastatin reduces MK4 formation in the kidneys by 45%.[ref]
Antibiotics may decrease conversion:
Conversion of vitamin K2 in the gut microbiome depends on having a good gut microbiome — so if you have been on a broad-spectrum antibiotic recently, your vitamin K conversion may be impaired.
Vitamin K content in foods:
| Food | Micrograms | Percent |
| (mcg) per serving | DV* | |
| Natto, 3 ounces (as MK-7) | 850 | 708 |
| Collards, frozen, boiled, ½ cup | 530 | 442 |
| Turnip greens, frozen, boiled ½ cup | 426 | 355 |
| Spinach, raw, 1 cup | 145 | 121 |
| Kale, raw, 1 cup | 113 | 94 |
| Broccoli, chopped, boiled, ½ cup | 110 | 92 |
| Soybeans, roasted, ½ cup | 43 | 36 |
| Carrot juice, ¾ cup | 28 | 23 |
| Soybean oil, 1 tablespoon | 25 | 21 |
| Edamame, frozen, prepared, ½ cup | 21 | 18 |
| Pumpkin, canned, ½ cup | 20 | 17 |
| Pomegranate juice, ¾ cup | 19 | 16 |
| Okra, raw, ½ cup | 16 | 13 |
| Salad dressing, Caesar, 1 tablespoon | 15 | 13 |
| Pine nuts, dried, 1 ounce | 15 | 13 |
| Blueberries, raw, ½ cup | 14 | 12 |
| Iceberg lettuce, raw, 1 cup | 14 | 12 |
(Adapted from NIH Fact Sheet Vitamin K)
In addition, a new study on organ meat from beef shows that heart, kidney, and oxtail are excellent sources of vitamin K.[ref]
You can track your vitamin K intake using cronometer.com, which is a free web app for determining micronutrients and macronutrients based on what you eat.
Related Articles and Topics:
References:
Berkner, Kathleen L. “The Vitamin K-Dependent Carboxylase.” Annual Review of Nutrition, vol. 25, 2005, pp. 127–49. PubMed, https://doi.org/10.1146/annurev.nutr.25.050304.092713.
Borgiani, Paola, et al. “CYP4F2 Genetic Variant (Rs2108622) Significantly Contributes to Warfarin Dosing Variability in the Italian Population.” Pharmacogenomics, vol. 10, no. 2, Feb. 2009, pp. 261–66. PubMed, https://doi.org/10.2217/14622416.10.2.261.
Chiba, Tsuyoshi, et al. “Trans-Resveratrol Enhances the Anticoagulant Activity of Warfarin in a Mouse Model.” Journal of Atherosclerosis and Thrombosis, vol. 23, no. 9, Sept. 2016, pp. 1099–110. PubMed Central, https://doi.org/10.5551/jat.31765.
Danziger, John. “Vitamin K-Dependent Proteins, Warfarin, and Vascular Calcification.” Clinical Journal of the American Society of Nephrology : CJASN, vol. 3, no. 5, Sept. 2008, pp. 1504–10. PubMed Central, https://doi.org/10.2215/CJN.00770208.
Dubovyk, Yevhen I., et al. “G-1639A but Not C1173T VKORC1 Gene Polymorphism Is Related to Ischemic Stroke and Its Various Risk Factors in Ukrainian Population.” BioMed Research International, vol. 2016, 2016, p. 1298198. PubMed Central, https://doi.org/10.1155/2016/1298198.
Edson, Katheryne Z., et al. “Cytochrome P450-Dependent Catabolism of Vitamin K: ω-Hydroxylation Catalyzed by Human CYP4F2 and CYP4F11.” Biochemistry, vol. 52, no. 46, Nov. 2013, pp. 8276–85. DOI.org (Crossref), https://doi.org/10.1021/bi401208m.
Geng, Huixia, et al. “Association Between the CYP4F2 Gene Rs1558139 and Rs2108622 Polymorphisms and Hypertension: A Meta-Analysis.” Genetic Testing and Molecular Biomarkers, vol. 23, no. 5, May 2019, pp. 342–47. PubMed, https://doi.org/10.1089/gtmb.2018.0202.
Halder, Maurice, et al. “Vitamin K: Double Bonds beyond Coagulation Insights into Differences between Vitamin K1 and K2 in Health and Disease.” International Journal of Molecular Sciences, vol. 20, no. 4, Feb. 2019, p. 896. PubMed Central, https://doi.org/10.3390/ijms20040896.
Iwamoto, Jun. “Vitamin K2 Therapy for Postmenopausal Osteoporosis.” Nutrients, vol. 6, no. 5, May 2014, pp. 1971–80. PubMed Central, https://doi.org/10.3390/nu6051971.
Kaiser, Rachel, et al. “SNPs in VKORC1 Are Risk Factors for Systemic Lupus Erythematosus in Asians.” Arthritis and Rheumatism, vol. 65, no. 1, Jan. 2013, pp. 211–15. PubMed Central, https://doi.org/10.1002/art.37751.
Knapen, M. H. J., et al. “Vitamin K2 Supplementation Improves Hip Bone Geometry and Bone Strength Indices in Postmenopausal Women.” Osteoporosis International, vol. 18, no. 7, July 2007, pp. 963–72. PubMed Central, https://doi.org/10.1007/s00198-007-0337-9.
Kurnatowska, Ilona, et al. “Effect of Vitamin K2 on Progression of Atherosclerosis and Vascular Calcification in Nondialyzed Patients with Chronic Kidney Disease Stages 3-5.” Polskie Archiwum Medycyny Wewnetrznej, vol. 125, no. 9, 2015, pp. 631–40. PubMed, https://doi.org/10.20452/pamw.3041.
Liao, Duanxiu, et al. “Interaction Between CYP4F2 Rs2108622 and CPY4A11 Rs9333025 Variants Is Significantly Correlated with Susceptibility to Ischemic Stroke and 20-Hydroxyeicosatetraenoic Acid Level.” Genetic Testing and Molecular Biomarkers, vol. 20, no. 5, May 2016, pp. 223–28. PubMed, https://doi.org/10.1089/gtmb.2015.0205.
Meng, Chong, et al. “Correlation between CYP4F2 Gene Rs2108622 Polymorphism and Susceptibility to Ischemic Stroke.” International Journal of Clinical and Experimental Medicine, vol. 8, no. 9, 2015, pp. 16122–26.
Nimptsch, Katharina, et al. “The Association between Dietary Vitamin K Intake and Serum Undercarboxylated Osteocalcin Is Modulated by Vitamin K Epoxide Reductase Genotype.” The British Journal of Nutrition, vol. 101, no. 12, June 2009, pp. 1812–20. PubMed, https://doi.org/10.1017/S0007114508131750.
Patillon, Blandine, et al. “Positive Selection in the Chromosome 16 VKORC1 Genomic Region Has Contributed to the Variability of Anticoagulant Response in Humans.” PLoS ONE, vol. 7, no. 12, Dec. 2012, p. e53049. PubMed Central, https://doi.org/10.1371/journal.pone.0053049.
Schelleman, Hedi, et al. “Dosing Algorithms to Predict Warfarin Maintenance Dose in Caucasians and African Americans.” Clinical Pharmacology and Therapeutics, vol. 84, no. 3, Sept. 2008, pp. 332–39. PubMed Central, https://doi.org/10.1038/clpt.2008.101.
Simes, Dina C., et al. “Vitamin K as a Powerful Micronutrient in Aging and Age-Related Diseases: Pros and Cons from Clinical Studies.” International Journal of Molecular Sciences, vol. 20, no. 17, Aug. 2019, p. 4150. PubMed Central, https://doi.org/10.3390/ijms20174150.
Singh, Onkar, et al. “Influence of CYP4F2 Rs2108622 (V433M) on Warfarin Dose Requirement in Asian Patients.” Drug Metabolism and Pharmacokinetics, vol. 26, no. 2, 2011, pp. 130–36. PubMed, https://doi.org/10.2133/dmpk.dmpk-10-rg-080.
Sun, Xue, et al. “Impact of the CYP4F2 Gene Polymorphisms on the Warfarin Maintenance Dose: A Systematic Review and Meta-Analysis.” Biomedical Reports, vol. 4, no. 4, Apr. 2016, pp. 498–506. PubMed, https://doi.org/10.3892/br.2016.599.
Teichert, M., et al. “Vitamin K Epoxide Reductase Complex Subunit 1 (VKORC1) Polymorphism and Aortic Calcification: The Rotterdam Study.” Arteriosclerosis, Thrombosis, and Vascular Biology, vol. 28, no. 4, Apr. 2008, pp. 771–76. PubMed, https://doi.org/10.1161/ATVBAHA.107.159913.
Vitamin K: MedlinePlus Medical Encyclopedia. https://medlineplus.gov/ency/article/002407.htm. Accessed 1 July 2022.
VKORC1 Gene: MedlinePlus Genetics. https://medlineplus.gov/genetics/gene/vkorc1/. Accessed 1 July 2022.
Vos, Melissa, et al. “Vitamin K2 Is a Mitochondrial Electron Carrier That Rescues Pink1 Deficiency.” Science (New York, N.Y.), vol. 336, no. 6086, June 2012, pp. 1306–10. PubMed, https://doi.org/10.1126/science.1218632.