Have you tried fasting or perhaps a ketogenic diet and felt horrible? If so, a possible reason for feeling bad might be how your body uses different fats.
People with inborn errors of metabolism may not be able to use fatty acids for energy as easily as most people do. Carrying mutations related to short-chain fatty acid metabolism may make you feel terrible when fasting or on a ketogenic diet. Mutations in two copies of these genes are usually identified in infancy due to the extreme reaction to being unable to go very long without eating. Members will see their genotype report below, plus additional solutions in the Lifehacks section. Join today.
Using Fat for Fuel: Short-chain fatty acids
The human body is wonderfully made and resilient enough to get energy from various food sources. Most people can survive and thrive using either carbs or fats. When our ancestors ran out of grain or potatoes, they could survive on fish or sheep. But certain genetic mutations can cause people not to burn fat for energy as efficiently.
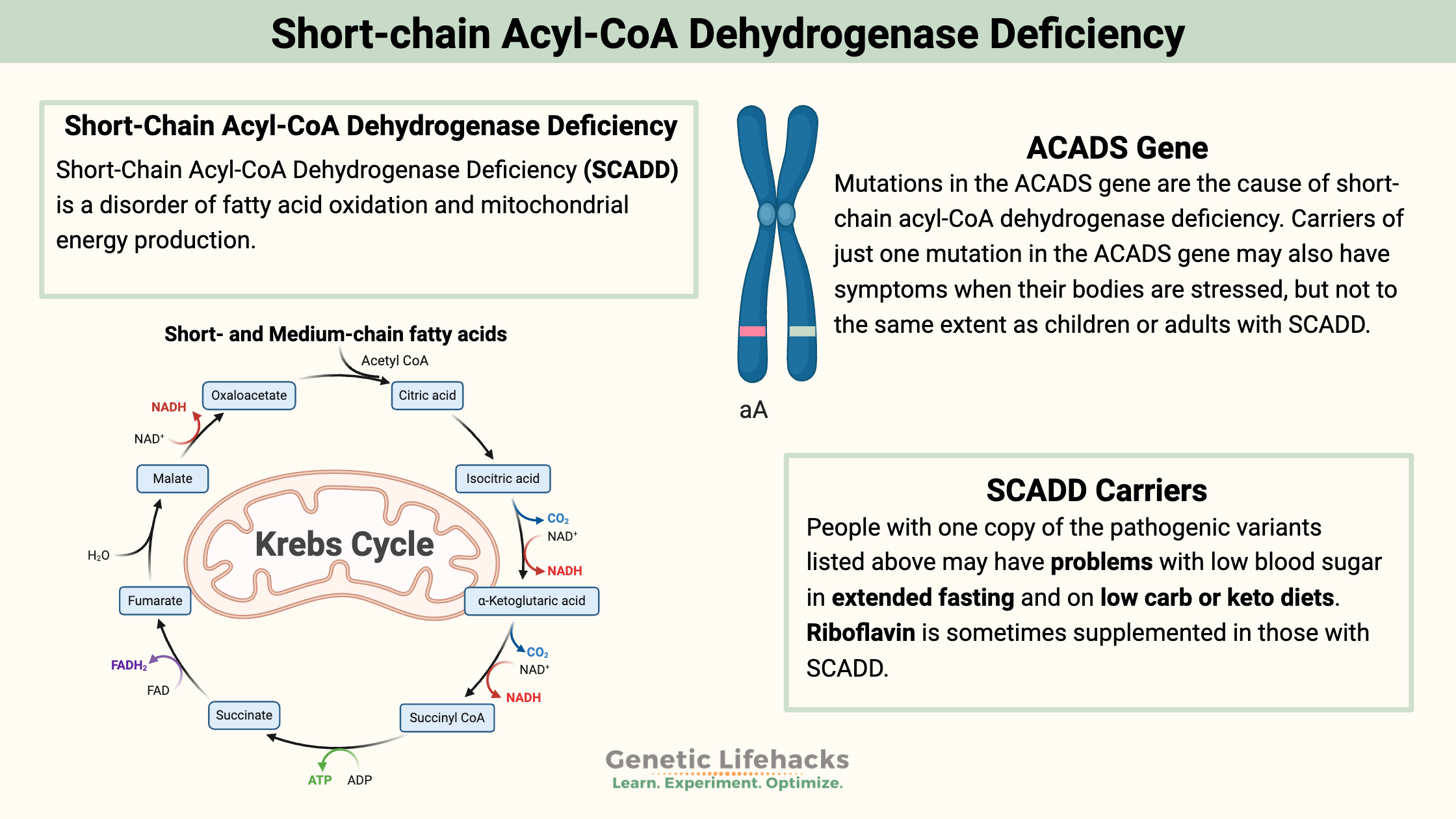
Short-Chain Acyl-CoA Dehydrogenase Deficiency (SCADD) is a disorder of fatty acid oxidation and mitochondrial energy production. Think back to high school biology class when you learned that the mitochondria are the cellular “powerhouse”, making ATP or energy for our body. The ATP production process in the mitochondria can begin with either glucose (a sugar) or fatty acids.
If you start with glucose, glycolysis breaks down the glucose into two pyruvate molecules, which transform into acetyl-CoA. Fatty acids can also create acetyl-CoA, which begins the production of ATP in the Krebs cycle and then the electron energy transport chain.
Short-Chain Acyl-CoA Dehydrogenase enzyme deficiency
Short-Chain Acyl-CoA Dehydrogenase is an enzyme that converts short-chain fatty acids for use in the mitochondria. A deficiency of the enzyme makes it harder for an individual to use certain fatty acids for fuel.
Mutations in the ACAD gene can cause short-chain acyl-CoA dehydrogenase deficiency (SCADD). SCADD is classified as an inborn error of metabolism, which means it is an inherited disorder that affects a person’s ability to metabolize a specific nutrient. It is a rare disorder usually detected in infancy. Two copies of the mutation are needed to have the disorder.
Symptoms in infants with SCADD include hypoglycemia, lack of energy, vomiting, poor feeding, seizures, poor muscle tone, developmental delays, and failure to grow/thrive. This deficiency can be deadly if not managed with regular feedings.
Some newborn screenings now look for SCADD. Early detection and treatment can mitigate developmental problems.[ref] Increased screening has led to research showing that not all people who carry the SCADD mutations have symptoms.
Affected individuals may only have symptoms during times of fasting, illness, or other physiologic stress. During fasting or stress, the body can shift from using carbohydrates for energy to burning fatty acids. A recommendation for children with SCADD is to ensure they eat regularly to prevent hypoglycemia. (More info on SCADD)
Carriers of just one mutation in the ACADS gene may also have symptoms when their bodies are stressed, but not to the same extent as children or adults with SCADD. Studies so far have been small and inconclusive.[ref]
Recent research points to the mutations in ACADS causing the protein to misfold. It is theorized that SCADD symptoms may be due to decreased cellular energy combined with a toxic accumulation of the enzyme.[ref]
ACADS: Genotype Report
Lifehacks
The following changes may help with managing short-chain acyl-CoA deficiency carriers.
Avoiding Long Fasts:
People with one copy of the pathogenic variants listed above may have problems with low blood sugar in extended fasting. It is something to be aware of and plan for during fasting or illness. It may be especially true for kids.
Additionally, hard exercise without eating or drinking a lot of alcohol without eating may cause a drop in blood sugar levels.
Related Articles and Topics:
Intermittent Fasting: Benefits from changing Gene Expression
The intermittent fasting concept has gained traction in health circles. Learn more about the importance of when you eat and its effects on gene expression.
Is intermittent fasting right for you?
Intermittent fasting and ketosis have a lot of benefits, but they may not be right for you. Your genes play a role in how you feel when fasting. Learn more about how this new trend might or might not be a good fit for you.
Genetic Superpowers Report
This Genetic Superpowers Report looks at the positive side of genetic variants. Everyone has some kind of genetic superpower, and hopefully, this report will highlight yours!
Mediterranean Diet and Your Genes
A study examined the interaction between a Mediterranean diet, genetics, and metabolic syndrome. Find out if a Mediterranean diet would work well for you.
References:
An, Se Jin, et al. “Compound Heterozygous Mutations of ACADS Gene in Newborn with Short Chain Acyl-CoA Dehydrogenase Deficiency: Case Report and Literatures Review.” Korean Journal of Pediatrics, vol. 59, no. Suppl 1, Nov. 2016, pp. S45–48. PubMed Central, https://doi.org/10.3345/kjp.2016.59.11.S45.
Edhager, Anders V., et al. “Proteomic Investigation of Cultivated Fibroblasts from Patients with Mitochondrial Short-Chain Acyl-CoA Dehydrogenase Deficiency.” Molecular Genetics and Metabolism, vol. 111, no. 3, Mar. 2014, pp. 360–68. PubMed, https://doi.org/10.1016/j.ymgme.2014.01.007.
Ghosh, Sujoy, et al. “Short Chain Acyl-CoA Dehydrogenase Deficiency and Short-Term High-Fat Diet Perturb Mitochondrial Energy Metabolism and Transcriptional Control of Lipid-Handling in Liver.” Nutrition & Metabolism, vol. 13, Mar. 2016, p. 17. PubMed Central, https://doi.org/10.1186/s12986-016-0075-0.
Kruger, Claudia, et al. “Brain Transcriptional Responses to High-Fat Diet in Acads-Deficient Mice Reveal Energy Sensing Pathways.” PLoS ONE, vol. 7, no. 8, Aug. 2012, p. e41709. PubMed Central, https://doi.org/10.1371/journal.pone.0041709.
Nochi, Zahra, et al. “Short-Chain Acyl-CoA Dehydrogenase Deficiency: From Gene to Cell Pathology and Possible Disease Mechanisms.” Journal of Inherited Metabolic Disease, vol. 40, no. 5, Sept. 2017, pp. 641–55. PubMed, https://doi.org/10.1007/s10545-017-0047-1.
Rs121908006 RefSNP Report – DbSNP – NCBI. https://www.ncbi.nlm.nih.gov/snp/rs121908006. Accessed 13 Sept. 2022.
Tonin, Rodolfo, et al. “Clinical Relevance of Short-Chain Acyl-CoA Dehydrogenase (SCAD) Deficiency: Exploring the Role of New Variants Including the First SCAD-Disease-Causing Allele Carrying a Synonymous Mutation.” BBA Clinical, vol. 5, Mar. 2016, pp. 114–19. PubMed Central, https://doi.org/10.1016/j.bbacli.2016.03.004.
van Maldegem, Bianca T., Marinus Duran, Ronald J. A. Wanders, Hans R. Waterham, Tom J. de Koning, et al. “Fasting and Fat-Loading Tests Provide Pathophysiological Insight into Short-Chain Acyl-Coenzyme a Dehydrogenase Deficiency.” The Journal of Pediatrics, vol. 156, no. 1, Jan. 2010, pp. 121–27. PubMed, https://doi.org/10.1016/j.jpeds.2009.07.008.
van Maldegem, Bianca T., Marinus Duran, Ronald J. A. Wanders, Hans R. Waterham, and Frits A. Wijburg. “Flavin Adenine Dinucleotide Status and the Effects of High-Dose Riboflavin Treatment in Short-Chain Acyl-CoA Dehydrogenase Deficiency.” Pediatric Research, vol. 67, no. 3, Mar. 2010, pp. 304–08. PubMed, https://doi.org/10.1203/PDR.0b013e3181cbd57b.
Wolfe, Lynne, et al. “Short-Chain Acyl-CoA Dehydrogenase Deficiency.” GeneReviews®, edited by Margaret P. Adam et al., University of Washington, Seattle, 1993. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK63582/.