Key takeaways:
~ Tick bites can cause some people to make IgE antibodies to galactose-alpha-1,3-galactose (alpha-gal).
~ Some people with alpha-gal IgE antibodies have gastrointestinal reactions, hives, or even anaphylaxis a few hours after eating meat.
~ The delayed allergic reaction can make it difficult to pinpoint the source of the reaction, leading to misdiagnosis and many frustrating allergic reactions.
The rest of this article is for Genetic Lifehacks members only. Consider joining today to see the rest of this article.
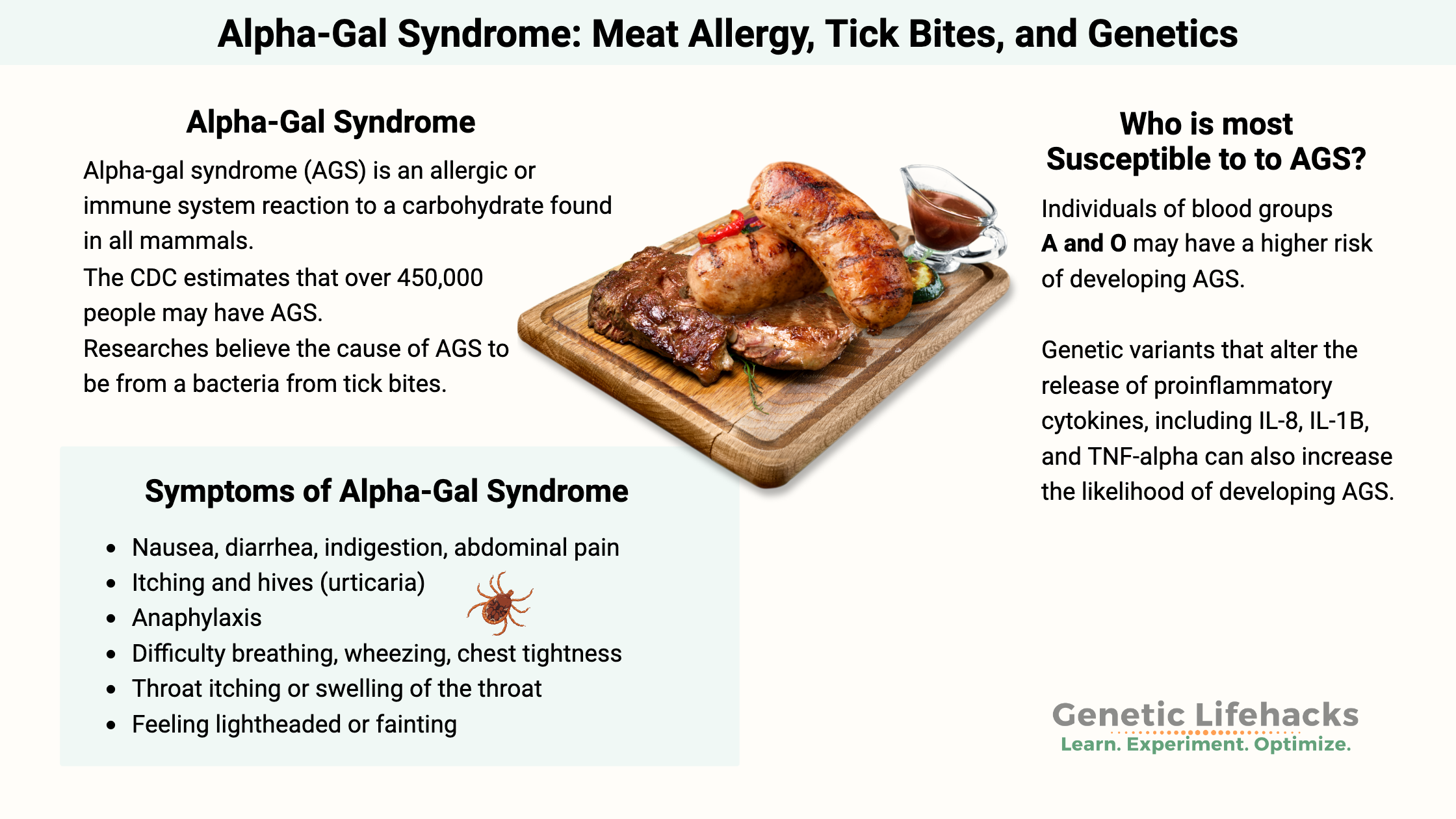
What is alpha-gal syndrome (AGS)?
Alpha-gal syndrome is an allergic or immune system reaction to galactose-alpha-1,3-galactose (called alpha-gal), which is a carbohydrate found in the tissues of all mammals except for humans and other primates. In alpha-gal syndrome, people produce IgE antibodies to alpha-gal (galactose-α-1,3-galactose), which can then cause a delayed allergic reaction when they eat meat.
Symptoms of alpha-gal syndrome can include:[ref]
- nausea, diarrhea, indigestion, abdominal pain
- itching and hives (urticaria)
- anaphylaxis
- difficulty breathing, wheezing, chest tightness
- throat itching or swelling of the throat
- feeling lightheaded or fainting
These delayed allergy symptoms appear several hours after eating beef, pork, lamb, venison, elk, or other mammalian meats.
Alpha-gal syndrome, or AGS, is most common in the southern US and Australia. In 2023, the CDC estimated that 450,000 people in the US may have alpha-gal syndrome.[ref] Misdiagnosis and delayed diagnosis are common because the reaction is delayed for hours after the meal.[ref]
Researchers believe that the cause of AGS is caused by tick bites that trigger the IgE antibodies to galactose-α-1,3-galactose (alpha-gal). When ticks bite, they secrete saliva and bacteria into the host. It is thought that this secretion activates antibodies against alpha-gal.[ref]
Let’s dive into the research on alpha-gal syndrome and see why some people may be more reactive than others.
What is galactose-α-1,3-galactose?
Galactose-α-1,3-galactose, or alpha-gal for short, is a carbohydrate molecule found in the cells of most mammals, except for humans and some primates. It is a type of oligosaccharide, which means it is made up of a few simple sugars linked together.
While we usually think of sugar as the white stuff you spoon into your coffee, in the chemical sense, sugar is a simple unit consisting of carbons, hydrogens, and oxygens that make up carbohydrates. In alpha-gal, the galactose sugars are linked by an α-1,3 glycosidic bond, making it an oligosaccharide.
While it may seem strange to think of a carbohydrate on the surface of your cells, one function of oligosaccharides in the body is as cell recognition molecules. An example that you’re probably familiar with is your ABO blood type. Your blood type (A, B, AB, or O) is determined by specific oligosaccharides on the surface of cells.
Alpha-gal (Galactose-α-1,3-galactose) is composed of two galactose monosaccharides linked by an α-1,3 glycosidic linkage. The α-1,3 linkage is not found in human cells because humans lack the enzyme α-1,3-galactosyltransferase, which is responsible for forming this linkage. α-Gal is abundant in red meat (e.g., beef, pork, lamb) and in some mammalian products such as gelatin and cow’s milk.
The absence of α-gal in humans is thought to be the result of an evolutionary adaptation, possibly due to selective pressure from pathogens that use α-gal to attach to host cells. Humans actually have most of the gene that encodes alpha-gal, but it is an inactive pseudogene for us.
Alpha-gal antibodies:
A quick overview of IgE vs IgG, IgA, and IgM antibodies:
The immune system produces antibodies so that it can respond to pathogens. Here’s a quick overview because I always have a hard time remembering which is which with the immunoglobulins (Ig):
- IgM: The first antibodies produced by B cells when a pathogen is present. IgM helps with the immune system’s initial defense.
- IgG: These are the most common antibodies, produced so that the immune system remembers a pathogen and can quickly mount a defense if the pathogen is seen again.
- IgA: These are the antibodies found in mucous membranes (nose, lungs, intestines), saliva, and breast milk to protect against pathogens.
- IgE: These are the antibodies that can bind to mast cells and cause allergic reactions — this is what we are talking about with alpha-gal syndrome, IgE antibodies to the alpha-gal oligosaccharide.
Since α-gal is not present in human tissues, the immune system recognizes it as a foreign substance and produces antibodies against it. Naturally occurring anti-α-gal IgG antibodies are the most abundant natural antibodies in humans, making up approximately 1% of all immunoglobulins in human serum. Humans can also produce IgA and IgM antibodies against alpha-gal. These are thought to be produced in response to exposure to bacteria in the gut microbiome.[ref][ref]
These antibodies are thought to play a role in immune defense against certain bacteria and parasites that express α-gal on their surface. For example, in areas with malaria, research shows that the IgM antibody response to alpha-gal likely helps to prevent Plasmodium infection and malaria. Similarly, alpha-gal antibodies are thought to protect against Chagas disease.[ref] Some research suggests that alpha-gal antibodies reduce symptoms of Covid, but not all research agrees.[ref]
Certain gut bacteria, including E. coli and Klebsiella strains, express alpha-gal, as do tick-borne bacteria such as Borrelia burgdorferi, which is the bacteria that causes Lyme disease.[ref]
One big reason for research on alpha-gal:
The reason humans can’t easily handle organ transplants from animals other than chimpanzees is that alpha-gal antibody reactions cause rejection of the organ. Researchers are working on pig organs that don’t have the alpha-gal oligosaccharide, and they are creating genetically modified pigs to provide meat for people with AGS. Research is also underway using bioprosthetic heart valves with most of the alpha-gal epitope inactivated[ref]
Alpha-gal meat allergy:
In individuals with alpha-gal allergy, exposure to α-gal, usually through tick bites, triggers the production of IgE antibodies specific to the carbohydrate. Researchers found that “The tick-borne pathogen Anaplasma phagocytophilum increases the level of tick α-Gal, which potentially increases the risk of developing AGS after a bite by a pathogen-infected tick.” Other pathogens and the tick saliva can also carry the alpha-gal oligosaccharide.[ref]
The lone star tick bite is most likely to cause Alpha-Gal Syndrome, but other ticks across the continents can also trigger the meat allergy.[ref] However, it is really important to note that not everyone with alpha-gal IgE has a meat allergy. In the southern United States, where the lone star tick is endemic, up to 32% of people show some degree of alpha-gal IgE sensitization[ref]
A study of meat allergy patients showed that they had overall higher IgE levels than a control group. Additionally, the meat allergy patients all had IgE antibodies to alpha-gal, while the control group did not. [ref]
Eating mammalian meat containing α-gal then leads to an allergic reaction, as the IgE antibodies bind to the α-gal in the meat and cause the release of histamine and other mediators from mast cells.
As a carbohydrate, alpha-gal is not denatured by high cooking temperatures. In people diagnosed with meat allergy, research shows that the anti-α-gal monoclonal antibody cross-reacts not only with alpha-gal, but also with a number of other beef proteins, including β-enolase and creatinine kinase.[ref]
However, not everyone with IgE antibodies to alpha-gal will have an allergic reaction to meat. And not everyone who is bitten by a lone star tick will develop IgE antibodies to alpha-gal.[ref]
Symptoms vary… a lot:
Many patients with AGS are initially misdiagnosed as having irritable bowel syndrome or chronic diarrhea, not realizing that the problem is meat.[ref]
Part of the frustration with alpha-gal syndrome is that the symptoms can vary greatly and aren’t consistently triggered. For example, someone may be fine eating lean beef most of the time, but then have symptoms the next time they eat a steak. This makes it really hard for someone to pinpoint what is causing the reaction – which of the ten things you ate that day caused your itchy hives or intestinal distress?
Research shows that anaphylactic reactions are most common after eating pork kidney (very high in alpha-gal). One study exposed people with AGS to meals containing different meats (beef, pork, lamb, and venison) and found that the delayed allergic reaction occurred 53% of the time with beef, 47% with pork, 9% with lamb, and 7% with venison.[ref][ref]
Part of the difference is that the amount of fat in the meat seems to play a role in whether the alpha-gal oligosaccharide enters the circulation. So it’s a combination of how fatty the meat is, how well a person digests, and whether there are problems with gut barrier function.[ref]
In a study looking at changes in alpha-gal patients for a wide range of cellular functions, the researchers found that fatty acid metabolites were altered. People with allergic symptoms to meat had delayed fat absorption and metabolism compared to healthy controls. They also had altered bile acid metabolism. Alpha-gal is found in both proteins and fats (glycolipids) from mammal meat. Altered fat absorption and transport would explain why the allergic symptoms are delayed for hours after eating meat.[ref]
More than just meat:
While the emphasis for AGS is on the reaction to eating beef, pork, lamb, etc., I want to point out that there are a couple of injectable medications that can cause anaphylaxis in people with alpha-gal IgE antibodies.
Cancer drug and Monoclonal Antibody reaction:
Cetuximab is a cancer drug that is grown in an animal (mouse) cell line that contains the alpha-gal carbohydrate on it. Recombinant monoclonal antibodies are being developed for a lot of conditions, including cancer treatment. Cetuximab is a monoclonal antibody that is a chimeric mouse-human IgG1 antibody. People with alpha-gal syndrome can have a hypersensitivity or even an anaphylactic reaction to cetuximab. It was a breakthrough when researchers in 2008 found that patients with hypersensitivity to cetuximab had antibodies that reacted to it even before exposure to the monoclonal antibody. The study showed not only the IgE antibodies to galactose-α-1,3-galactose (alpha-gal) but also that there was a geographic clustering of where the patients who had reactions lived. The geographic locations overlap with the prevalence of lone star ticks, which cause AGS.[ref]
Other engineered monoclonal antibodies may also be produced using mammalian cell lines. Most present very low levels of alpha-gal, but there are case reports of people reacting to a couple of other monoclonal antibodies.[ref]
Varicella vaccine reactions:
Case reports also show that the varicella (chickenpox) vaccine can cause anaphylaxis in children with alpha-gal IgE antibodies. Additionally, a patient study showed a positive pin-prick skin test with a similar allergic reaction to MMR and porcine gelatin in a child with an IgE reaction to the chickenpox vaccine.[ref] Similarly, reactions are possible to the shingles varicella vaccine.[ref][ref]
The theory on this is that vaccines produced using bovine calf serum can contain alpha-gal, and injecting this causes the reaction in someone with the IgE alpha-gal antibodies. There are several vaccines that may contain bovine serum, including certain hepatitis A vaccines, MMR, rotavirus, and varicella zoster. Not all manufacturers use bovine serum, so it is something to ask about if you have alpha-gal and are getting a vaccine. Here’s a Wikipedia list that shows which vaccines use bovine serum (I’m not sure how up-to-date it is…).
Genetic connections: Why some people get alpha-gal and others don’t
Many people are bitten by ticks every year, but only a small percentage end up with AGS.
Let’s take a look at the research so far, keeping in mind that this is a relatively newly discovered condition:
Blood type is linked to susceptibility to alpha-gal syndrome. People with blood type B or AB are less likely to get alpha-gal compared to people with blood type A or O. The blood type B antigen oligosaccharide is similar in molecular structure to the alpha-gal oligosaccharide, and researchers think this makes people with blood type B more resistant to developing antibodies against alpha-gal.[ref]
Patients with AGS have also been found to have higher basophil reactivity than asymptomatic alpha-gal-sensitized individuals.[ref] Basophils are a type of white blood cell that reacts to pathogens, parasites, and allergens. There are a number of reasons for higher basophil activity, including Hashimoto’s thyroiditis (antibodies against thyroid antigens). Additionally, higher basophil reactivity is found in people with spontaneous urticaria (itching, hives).[ref]
People who are prone to allergies are more likely to develop IgE antibodies to alpha-gal. Several studies show that people who are hypersensitive and prone to allergies (including dust mites, dander, and food allergies) are more likely to have elevated anti-α-Gal IgE levels.[ref]
People with mast cell disorders or a history of anaphylaxis are more likely to have IgE antibodies for alpha-gal.[ref]
There are also genetic differences in the way that people react to a tick bite (or other insect bites). The “host response” to a tick bite involves an innate immune response with blood clotting at the site of the bite and the release of proinflammatory cytokines, including IL-8, IL-1β B, and TNF-alpha. Certain types of ticks produce histamine-binding proteins in their saliva so that when you’re bitten by the tick, the normal histamine released by the bite doesn’t cause itchiness (so you don’t notice the bite). Tick saliva also downregulates the attraction of neutrophils, which would normally be the immune response that engulfs and destroys foreign bacteria injected with the bite.[ref]
Genotype report:
I didn’t find any studies that directly investigate polymorphisms in people who have alpha-gal syndrome. However, much of the research on the syndrome is very recent, so genetic studies may be in the works soon.
This genotype report section instead focuses on genetic connections to susceptibility factors involved in AGS susceptibility, such as blood type and IgE levels.
Lifehacks:
If you think you have alpha-gal syndrome, your doctor can help you with alpha-gal IgE testing and with good advice for your specific situation. For some people, an epi-pen or other rescue measures are needed. Your doctor can also help with prescribing oral antihistamines or cromolyn sodium.
Having had a recent tick bite is usually a prerequisite for developing AGS, but a lot of times you can have a tick bite and not know it. Seed ticks are the larvae of ticks that are about the size of a poppy seed and hard to spot. Sometimes what you think are chigger bites could be caused by seed ticks. [ref]
Testing for alpha-gal IgE:
Your doctor can order a test for alpha-gal IgE (>0.1 IU/mL). If you can’t get in to see your doctor, it’s possible to order the test on your own in most states in the US. Depending on your insurance, sometimes it is cheaper to order the test on your own and then take the results to your doctor. Here are some testing options to get you started: UltaLab ($149 for a panel including other meat allergens plus alpha-gal IgE), Walk in Lab ($198 alpha-gal IgE), RequestATest ($109 alpha-gal IgE).
Keep in mind that people can have alpha-gal IgE levels without symptoms. Talk to your doctor about whether further challenges, such as eating a meal high in fatty pork, are needed for diagnosis. Sometimes a history of reactions is enough for diagnosis, but others may need to do a challenge meal while in a medical setting to prevent anaphylaxis.[ref]
Related topics and articles:
Histamine Intolerance: Genetic Report, Supplements, and Real Solutions
MRGPRX2: Mast Cells, Itching, & Drug Hypersensitivity Reactions, Including Fluoroquinolones