Key takeaways:
~ Up to 80% of women will experience hot flashes, or vasomotor symptoms (VMS), during menopause.
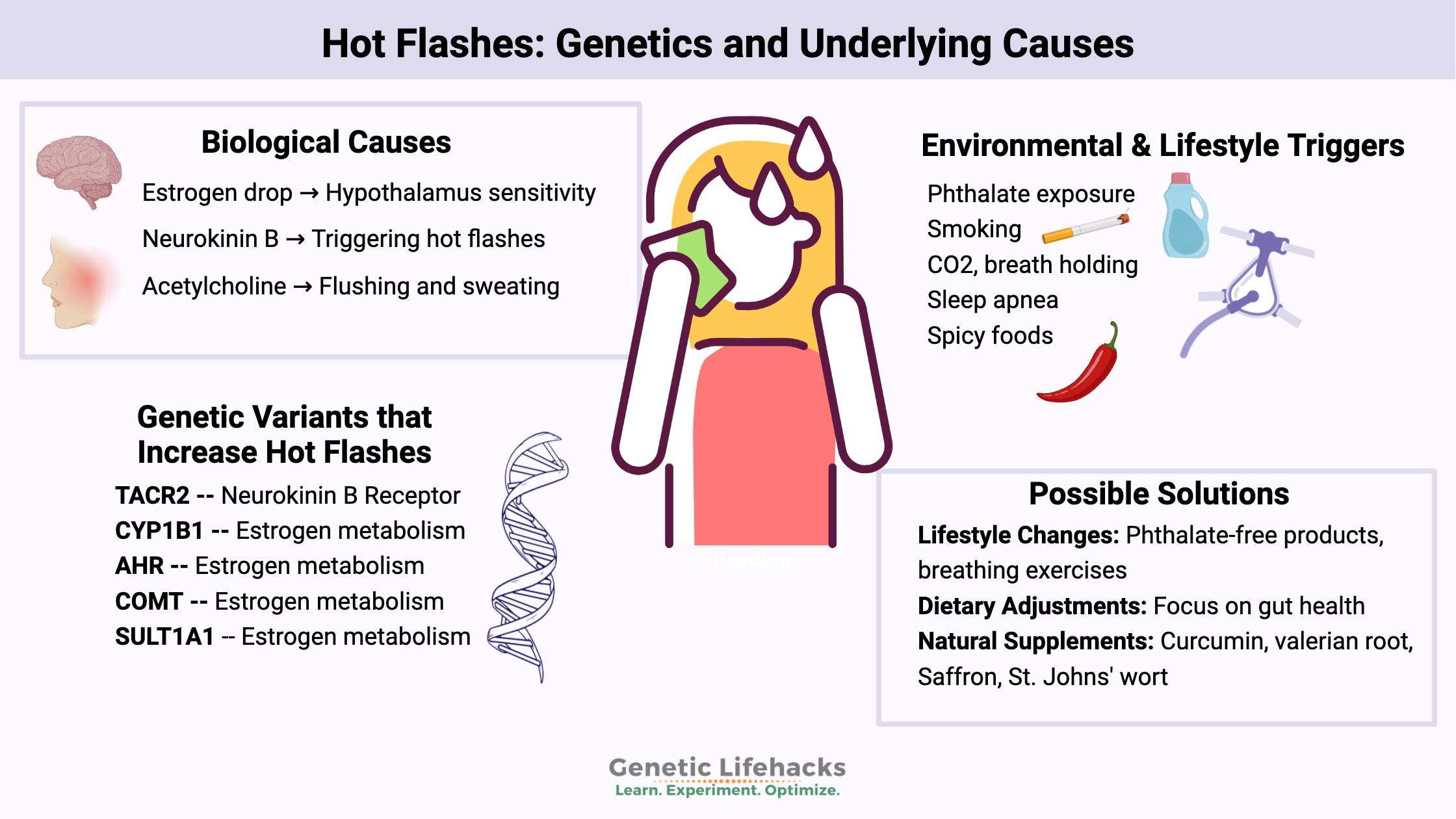
~ Research shows that changes in estrogen levels and activation of neurokinin 3 receptors in the hypothalamus are involved in triggering hot flashes.
~ Natural supplements and key lifestyle changes may help to reduce the intensity and duration of hot flashes.
What causes hot flashes?
Have you ever experienced a sudden wave of heat during menopause? You’re not alone. About 53-80% of women experience hot flashes around the time of menopause.[ref]
Hot flashes, or vasomotor symptoms, are a hallmark of the menopausal journey for many women. Hot flashes cause a sudden feeling of warmth, often accompanied by sweating and a flushed face. Some people also feel irritable and anxious during a hot flash. At night, hot flashes can cause night sweats and disrupt sleep.[ref]
What causes hot flashes? Why does the body’s temperature system seem to suddenly go haywire? Let’s dive into the science:
Biological causes of hot flashes:
While the exact cause of hot flashes is still not fully understood, several biological factors are thought to play a role.
Declining estrogen levels:
Women are born with a finite number of egg cells. As the number of eggs or follicles in the ovaries dwindles, estrogen levels will decline and the cyclical rise and fall of FSH (follicle-stimulating hormone) changes. This is called the menopausal transition or perimenopause.[ref]
The brain’s temperature control is sensitive:
The hypothalamus, a part of the brain, acts as the body’s thermostat. When estrogen levels drop, it can cause the body’s thermostat (the hypothalamus) to become more sensitive to slight changes in body temperature.
As estrogen levels decline during menopause, the hypothalamus may mistakenly sense that the body is overheating. In response, it triggers a series of events to cool the body down, resulting in the symptoms of a hot flash.
Cooling off by flushing:
To dissipate the perceived heat, blood vessels near the skin’s surface dilate. This causes flushing and sweating as the body tries to cool down.
Physiologically, what triggers the perceived temperature changes?
For years, doctors and researchers have known that the drop in estrogen is linked to hot flashes, but they didn’t know the exact mechanism. One known link was that hot flashes could be stopped by increasing estradiol, a form of estrogen. Therefore, it was thought that a lack of estrogen caused hot flashes.
New research in the last decade helps explain why changes in estrogen levels cause the brain to think the body is too hot, and what other neuropeptides are involved in triggering hot flashes.
Estrogen in the brain is part of the picture:
The hypothalamus is the region of the brain responsible for maintaining a stable body temperature through a series of feedback systems. This region receives sensory information from the periphery (the arms, legs, etc.) and also regulates the temperature of the brain. The hypothalamus also controls the circadian changes in body temperature throughout the day and night.[ref]
Estrogens are steroid hormones that act on receptors in the nucleus of cells to cause the transcription of a number of different genes. Estradiol (E2) is the major circulating estrogen in women prior to menopause, and it is synthesized primarily in the ovaries.[ref] Thermosensitive neurons have estradiol receptors and can suppress heat production and increase heat loss. But it’s not as simple as estrogen=heat. Instead, there are both inhibitory and excitatory effects of estrogen in the hypothalamus.[ref]
For example, higher estrogen levels in women are associated with sweating more easily when exercising. Core body temperature also fluctuates in response to changing estrogen levels during the menstrual cycle (e.g. warmer during ovulation).[ref]
In menopause, the overall decrease in estrogen is associated with hot flashes. Estrogen-sensitive neurons are involved, but estrogen isn’t the only cause of hot flashes.[ref]
Neurokinin B plays an important role:
In the hypothalamus, neurokinin B (NKB) signals to its receptor during hot flashes. This is an adaptation in response to sex steroid deficiency (decreased estrogen).
Neurokinin B is a neuropeptide involved in the release of gonadotropin-releasing hormone (GnRH) in the hypothalamus. It is important during pregnancy and puberty.
GnRH secretion is what drives the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) in the menstrual cycle.[ref] In addition to estrogen declining, FSH and LH levels are also altered during menopause.
Here’s what researchers have learned recently about neurokinin B and hot flashes:
- Neurokinin B was identified in a genome-wide association study as the only gene that plays a significant role in hot flashes (vasomotor symptoms).[ref]
- Another strong indication that neurokinin B is integral to hot flashes is that when neurokinin B is given to young women by IV, it triggers hot flashes in 80% of the women.[ref]
- A placebo-controlled clinical trial of an NK3R (neurokinin B receptor) antagonist drug, which blocks the neurokinin B receptor, showed that it quickly reduced hot flash frequency by more than half compared to a placebo.[ref][ref]
The emerging picture is that hot flashes involve body temperature mechanisms in the hypothalamus that are affected by estrogen and neurokinin B, which in turn affect FSH and LH levels.
Acetylcholine and vasodilation:
In addition to what is going on in the brain with temperature control, women with hot flashes are likely to have an enhanced response to acetylcholine in small blood vessels. This means that the blood vessels are more likely to dilate rapidly due to the release of acetylcholine, causing the sweating and flushing associated with hot flashes.[ref]
A clinical trial of an anticholinergic drug found that it was superior to placebo in reducing hot flashes. Anticholinergic drugs block acetylcholine.[ref]
Environmental factors that increase hot flashes:
Phthalates: endocrine disruptors and increased hot flashes
Phthalates are a class of chemicals used in cosmetics, shampoos, vinyl products, artificial fragrances, nail polish, deodorants, and lotions. They are ubiquitous, meaning that pretty much everyone is exposed to them these days. Phstalates can act as endocrine disruptors or estrogen mimics. A recent study showed that women who had higher phthalate levels in their system were about 45% more likely to have hot flashes. [ref] Multiple studies replicate this association of phthalates with hot flashes.[ref][ref]
High CO2 levels:
When you hold your breath, CO2 levels rise, and an increase in CO2 levels can trigger hot flashes in menopausal women.
A study in healthy menopausal women used a brief CO2 exposure of a single inhalation of 20% or 35% CO2. This mimics the increase in CO2 seen during panic attacks, anxiety, or breath-holding. The majority of the menopausal women experienced a hot flash within minutes of inhaling 20% CO2.[ref]
Sleep apnea:
Along the same lines of breath holding and CO2 rising, sleep apnea is also associated with increased hot flashes.[ref]
Chronic inflammation and more intense hot flashes:
Researchers have found that the intensity of hot flashes is associated with higher levels of inflammatory cytokines (IL-8 and TNF-alpha). According to the authors: “These results suggest that hot flashes are linked to low-grade systemic inflammation in postmenopausal women.”[ref]
Leaky gut and hot flashes:
Another study found that hot flush intensity may be related to increased intestinal barrier permeability (also known as leaky gut). Estrogen levels affect the gut microbiome and may cause higher levels of gut permeability. This, in turn, causes low-grade systemic inflammation.[ref]
Spicy foods, hot rooms:
While not a direct biological cause, certain external factors can trigger or worsen hot flashes. These include alcohol, caffeine, spicy foods, tight clothing, heat, and stress.
Smoking:
Cigarette smoking increases the odds of hot flashes by 6-fold.[ref] This may be through the interaction with the aryl hydrocarbon receptor and estrogen metabolism as well as increased inflammatory cytokines.
What isn’t linked to hot flashes?
- Research shows that a higher BMI is not associated with an increased risk of hot flashes.[ref]
- Cortisol and the cortisol awakening response are likely not involved in hot flashes, according to researchers.[ref]
What about men? Can they get hot flashes?
While hot flashes are commonly associated with menopause in women, men can also experience them, especially those undergoing certain medical treatments, such as hormone therapy for prostate cancer. The biological mechanisms in men may be similar, involving changes in hormone levels and the body’s temperature regulation system.
Genotype Report
Lifehacks: Natural hot flash relief
Natural lifestyle, diet, and herbal supplement options can help reduce hot flashes, and here are some of the research-backed solutions. While research studies don’t cover every natural treatment, they give us a good starting point for knowing what’s more likely to work.
Talk with your doctor about prescription medications and hormone replacement therapy (HRT) options for hot flashes. There are several options, but medications come with some risks and aren’t right for everyone.
Lifestyle changes to reduce hot flashes
Avoid phthalates as much as possible:
A number of studies show a strong link between higher levels of phthalates in the body and increased numbers of hot flashes.
Phthalates are found in many products, but a big source for women is personal care products. Look for lotions, shampoos, conditioners, and cosmetics that are phthalate-free. Another big source is artificial fragrances, such as those found in laundry products or air fresheners. Look for fragrance-free options.
Women who have lower levels of phthalates in their urine have fewer hot flashes on average.[ref] Read more about phthalates, genetics, and how they are metabolized.
Breathe:
The study on CO2 triggering hot flashes provides insight into how stressful situations can cause a hot flash, as many people naturally hold their breath when stressed. Breathing exercises can help you avoid instinctively holding your breath in a stressful situation. Look into box breathing, physiological sighing, or yoga breathing to help control your breathing.
Some research suggests that wearing a mask increases hot flashes. Wearing an N95 mask also increases CO2, but not as much as holding your breath. It may be that masking increases hot flashes due to the increase in heat on the face from the mask or due to increased CO2 levels.[ref]
Related article: Anxiety and Genetics (read the part about the CO2 sensing gene)
Dietary interventions:
A recent study found that a low-fat, plant-based diet with minimal oils helped reduce moderate to severe hot flashes. The intervention also included the daily consumption of cooked, non-GMO soybeans. Looking at the details of the dietary changes, fat intake decreased by about 50%, and fiber intake increased by 12g/day.[ref] There were several changes taking place in the study (eating soy, increasing fiber, and decreasing fat), which makes it difficult to know which component was effective(e.g. avoiding nuts, eating soy, or avoiding animal-derived foods).[ref]
Gut healthy diet:
The link between changing estrogen levels and the gut microbiome makes gut health a priority. What does a gut health diet look like? There are dozens of different types of diets that are promoted as healthy – from Mediterranean to DASH to Paleo. One thing they all have in common is that they cut out processed, packaged foods and focus on eating whole foods. Microbiome studies show that cutting out processed foods can help with gut health.[ref]
Related article: Emulsifiers, IL-10, and Leaky Gut
Research on natural supplements and drugs for hot flashes:
Below are some of the research studies on solutions for reducing hot flashes. Key here is that there are multiple options for reducing hot flashes, both natural supplements and prescription medications. Talk with your doctor for medical advice about what may work best for you, and if you’re taking supplements, be sure to ask about any drug interactions with what you’re taking.
Related Articles: