Key takeaways:
~ Selective IgA deficiency is found in approximately 1% of the population
~ The majority of people with IgA deficiency have no symptoms, but it can increase the risk of intestinal or respiratory infections, as well as allergies.
~ IgA deficiency can be (partly) genetic, or it can be due to other causes such as medications or autoimmunity.
Members will see their genotype report below, plus additional solutions in the Lifehacks section. Consider joining today.
What is IgA deficiency?
Selective IgA deficiency (SIgAD) is the most common immunodeficiency worldwide, with an estimated prevalence of 1:400. However, the prevalence varies considerably by ethnicity, being more common in Caucasian populations (about 1%)).[ref]
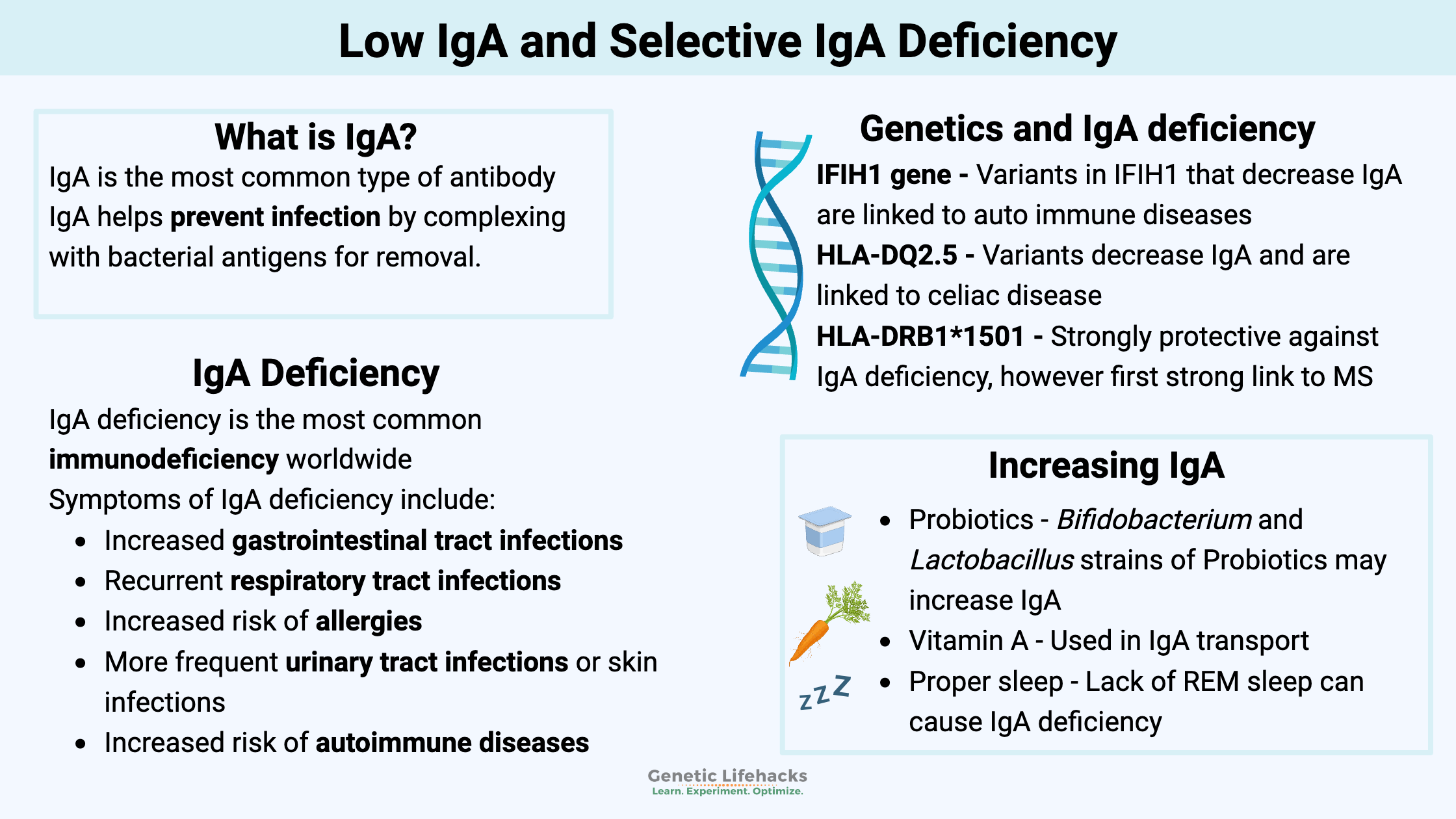
IgA deficiency is a genetic immunodeficiency disorder characterized by the absence or very low levels of immunoglobulin A (IgA). An essential antibody, IgA plays a critical role in protecting mucosal surfaces in the body, such as the respiratory and gastrointestinal tracts, from infection.
IgA is the most common type of antibody in the body. On mucosal surfaces, it helps prevent the penetration of intestinal bacteria through the intestinal or lung mucosa. IgA helps prevent infection by complexing with bacterial antigens for removal.[ref][ref]
Additionally, IgA plays a role in how the body tolerates food antigens and other antigens, making it important in allergies.[ref]
Serum IgA levels are influenced by age. At birth, IgA is virtually nonexistent, but it gradually increases throughout childhood and adolescence to reach adult levels. Normal adult levels range from 61 to 365 mg/dl.[ref]
Partial IgA deficiency is usually defined as serum IgA levels >7 mg/dl, but below the lower limit of the normal range for the age (e.g. 7 – 60 mg/dl for adults). Total IgA deficiency is usually defined as serum IgA levels < 7 mg/dl.[ref]
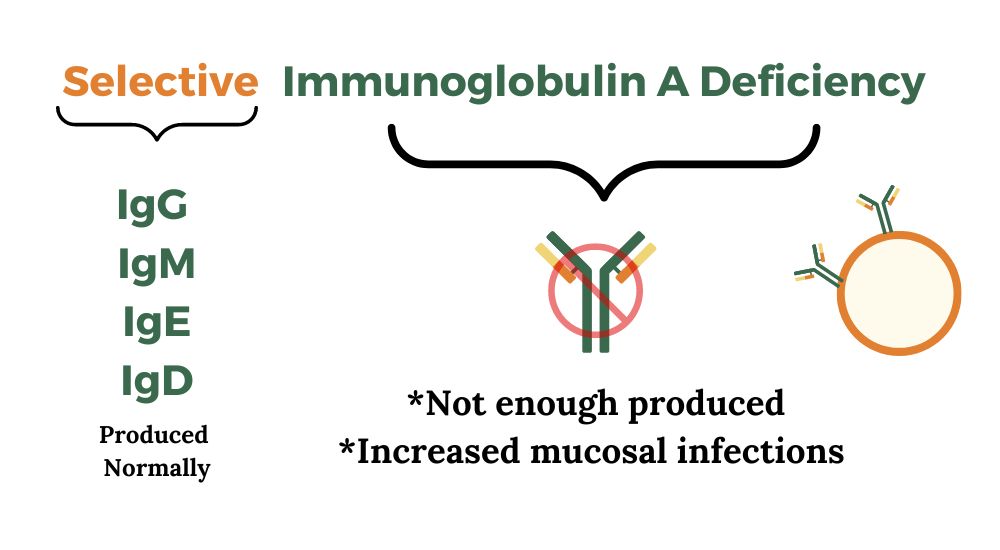
Selective IgA deficiency is the term used for low IgA levels but normal IgG, IgM, and IgE levels.
Symptoms of partial IgA deficiency:
Most people with IgA deficiency don’t have any noticable symptoms, but they may be prone to getting certain types of infections more often.
Symptoms of IgA deficiency include:[ref][ref][ref]
- Increased gastrointestinal tract infections
- Recurrent respiratory tract infections
- Increased risk of allergies
- More frequent urinary tract infections or skin infections
- Increased risk of autoimmune diseases
IgA deficiency is often diagnosed when testing for autoimmune diseases.
Celiac disease is much more common in people with IgA deficiency. In one study, 6.7% of celiac disease patients had IgA deficiency compared to 0.2% of healthy controls. Type 1 diabetes is also much more common in people with IgA deficiency.[ref]
What causes IgA Deficiency?
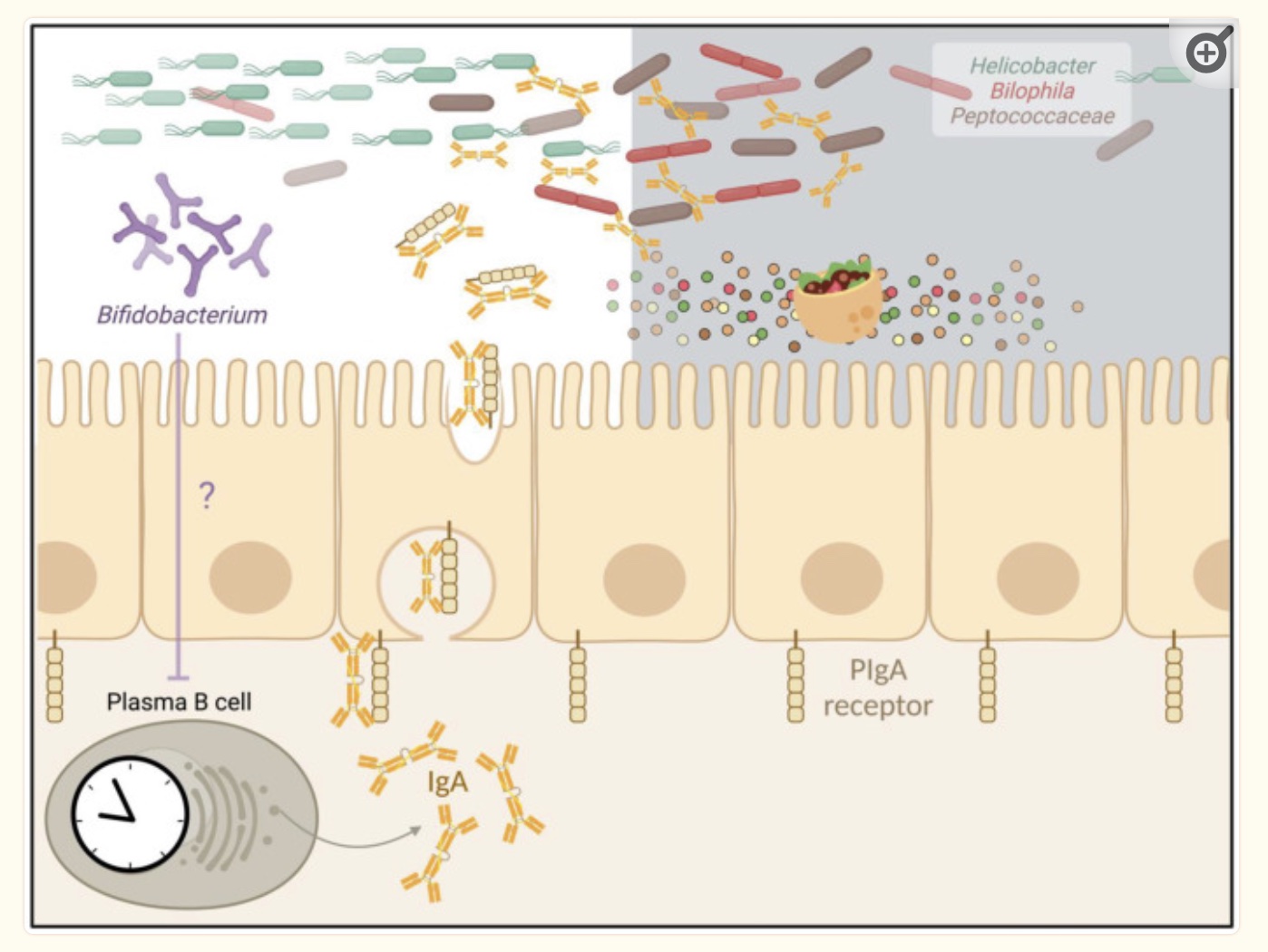
B ceB cells are a type of immune cell that produces antibodies. The IgA antibody can be released or secreted by the B cells into the mucosa. T cells and B cells interact, and this interaction causes the B cells to “class-switch” to produce IgA. IgA deficiency can be caused by problems with the B cells, with the T cells, or with the signaling molecules produced by the T cells to cause the B cell class switching.[ref]
Researchers are still figuring out all the mechanisms that cause low IgA levels. One reason for low IgA is depletion of CD4+CD25+ Treg cells. Another is the inability of B cells to switch classes. Yet another mechanism is reduced proliferative activity of CD4+ T cells.[ref][ref]
Genetics and IgA deficiency:
IgA deficiency can be inherited, and there is a genetic component to it for most people. For example, if your mother or father has IgA deficiency you have a 50-fold increased risk of having it. [ref]
However, there are several ways that someone can inherit IgA deficiency, and environmental factors likely also play a role.
Certain HLA types are associated with an increased susceptibility to IgA deficiency, and mutations related to common variable immunodeficiency can also cause IgA deficiency. Variants in TNFSF13 and IFIH1 also increase the relative risk of IgA deficiency.[ref][ref]
In addition, rare genetic diseases linked to a single mutation may also cause IgA deficiency, such as in people with ataxia-telangiectasia, Wiskott-Aldrich syndrome, and trisomy 22.[ref]
Other causes of IgA deficiency:
Certain bacteria and viruses can secrete an enzyme that destroys IgA, resulting in an IgA deficiency during infection. A type of pneumonia bacteria and a type of influenza virus can decrease IgA. The bacteria that cause gonorrhea also decrease IgA.
IgA deficiency may also be autoimmune or caused by certain medications.
Circadian rhythm, gut bacteria, and IgA:
Circadian rhythm refers to your built-in 24-hour molecular clock. The expression of many genes, including immune system genes, varies throughout the course of a day. For example, you won’t produce many of the enzymes needed to break down food while you’re asleep.
Interestingly, your gut microbiome also is impacted by your circadian rhythm, with fluctuating microbe levels over the course of a day. Changes in circadian rhythm can impact your gut microbiome. Jet lag, for example, throws off the oscillations of your gut bacteria.[ref]
Research on the gut microbiome, circadian rhythm, and the host (you!) immune system is fairly new. A recent study showed that secretory IgA levels are highest during the daytime – around mid-day – and lowest at night.[ref] This is something to keep in mind if you are getting your IgA levels tested, with tests at mid-day likely showing the highest levels compared to evening or early morning tests.
Research on the gut microbiome and IgA levels also shows that there is an interaction. Antibiotics decrease gut microbe levels, which is associated with lower IgA levels. Probiotics can also increase IgA levels.[ref]
IgA Deficiency Genotype Report
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Lifehacks for increasing IgA levels
Testing your IgA levels:
You may be wondering if your frequent respiratory infections mean that you have a partial IgA deficiency? The only way to know is to have an IgA blood test done. Talk with your doctor about ordering the test, or you can order it yourself in the U.S. through an online lab company.
Research Studies on Probiotics that Increase IgA:
The rest of this article is for Genetic Lifehacks members only. Consider joining today to see the rest of this article.
Related Articles and Topics:
Mannose Binding Lectin:
An important part of our innate defense against bacterial pathogens, low mannose binding lectin can leave you vulnerable to illnesses.
Celiac Genes:
People with celiac disease have certain HLA genotypes. You can check your genetic data to see if you are susceptible to celiac disease.