Key takeaways:
~ Nickel allergy is very common and causes a rash after contact.
~ Systemic reactions can occur with foods higher in nickel, causing gastrointestinal issues, headaches, and eczema.
~ Genes play a role in susceptibility to nickel allergy.
~ A couple of natural supplements may help with reactions.
Members will see their genotype report below, plus additional solutions in the Lifehacks section. Consider joining today.
Nickel Allergies: Genetics, Symptoms, Foods
Nickel allergy is a common cause of allergic contact dermatitis (rash). It is estimated that 8 – 20% of people are sensitive to nickel.[ref][ref]
However, nickel allergies can go beyond just getting a rash from your watch or bracelet. A systemic or internal response to certain foods that contain nickel is also possible.
What is a nickel allergy?
While genetic susceptibility plays a role (covered in the genotype report below), nickel allergy is caused by exposure to nickel, often for a long period of time.
Nickel can be found in:[ref]
- fashion jewelry
- watches or fitness trackers
- piercings
- clothing decorations or fasteners
- eyeglasses
- medical devices, such as orthopedics
- orthodontics
- cosmetics
- tools
- bathroom fixtures
- mobile phones
- keys, coins
Non-workplace contacts like piercing the ear with a regular needle and wearing fashion jewelry are more likely to cause sensitization in women.[ref]
Sweat can leach the nickel from metal alloys, such as stainless steel. Skin piercings and other nickel-containing exposures can cause those who are vulnerable to develop nickel sensitivity.[ref]
Additionally, nickel is a common component in many orthodontic materials, and nickel allergy is common in people with tongue or lip piercings.[ref]
Symptoms of nickel allergies: Skin Rash
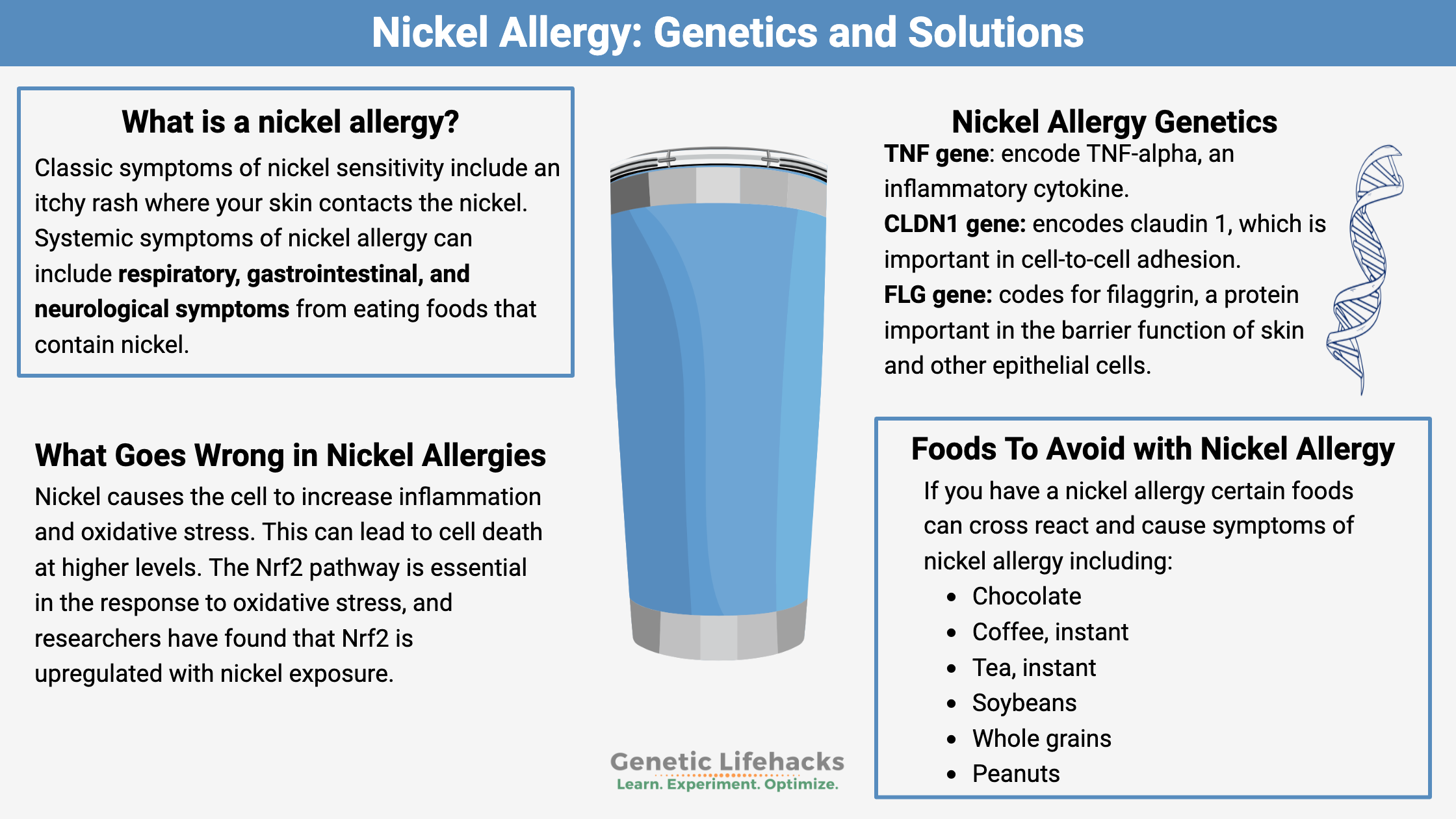
Classic symptoms of nickel sensitivity include an itchy rash where your skin contacts the nickel. This can be termed eczema or contact dermatitis. Other skin reactions can include vitiligo-like lesions, small raised bumps that form a ring, small blister clusters, cracked skin, and even vasculitis (inflammation of the blood vessels).[ref]
Systemic nickel allergy syndrome (SNAS):
Systemic symptoms of nickel allergy can include respiratory, gastrointestinal, and neurological symptoms from eating foods that contain nickel (or an implanted device that contains nickel).[ref]
For example, someone with a nickel allergy may end up with nausea, diarrhea, vomiting, and fatigue. Neurological symptoms include headaches and brain fog.[ref]
A mouth sore called oral lichenoid lesions is linked to higher-than-normal concentrations of nickel.[ref]
Foods to avoid because they cross-react with Nickel Allergies
Nickel is found in trace amounts in the soils, and plants can take up nickel through their roots. This means that plants can contain nickel, which can then cause systemic nickel allergy syndrome symptoms.
On average, we consume 300-600 μg of nickel per day. For someone very sensitive to nickel, the top end of this range could cause symptoms such as eczema.[ref]
If you have a nickel allergy, you may also be sensitive to certain foods that contain nickel or other metals that cross-react with nickel.[ref][ref] Some of the foods that can cross-react with nickel allergies include:[ref][ref]
- Chocolate
- Coffee, instant
- Tea, instant
- Soybeans
- Whole grains
- Peanuts
- Almonds
- Hazelnuts
- Lentils
These foods contain varying levels of nickel, and some people with nickel allergies may not experience any symptoms from eating them. However, for some people, consuming these foods can trigger a reaction similar to nickel allergy symptoms, such as a rash or itching in the mouth, throat, or skin.
Response to nickel:
So what happens when soluble nickel is taken into a cell? Nickel causes the cell to increase inflammation and oxidative stress. This can lead to cell death at higher levels. The Nrf2 pathway is essential in the response to oxidative stress, and researchers have found that Nrf2 is upregulated with nickel exposure.[ref]
Another study looked at inflammation over the course of three days after exposure using skin biopsies in nickel allergy patients. The researchers found that natural killer cells are upregulated, and memory T cells are activated. The response was not immediate and built over a couple of days.[ref]
Nickel Allergy Genotype Report:
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Lifehacks: Natural Treatments for Nickel Allergy
First and foremost – avoid contact with nickel-containing items such as earrings, piercings, watches, and jewelry.
If you wear glasses, make sure they don’t contain nickel in any parts against your skin. If your phone is metal, use a plastic or silicone case.
Nickel test kits are available to see if your cookware or jewelry contains nickel.
The rest of this article is for Genetic Lifehacks members only. Consider joining today to see the rest of this article.
Related Articles and Topics:
Genetics and Food Allergies
Do you have a food allergy? Discover how environmental factors and genetic susceptibility can shape individual reactions.
Histamine Intolerance: Understanding Your Genetics and Managing Symptoms
Genetics plays a big role in how well your body breaks down histamine. You can use your genetic data to figure out if your genes are part of the reason why you have histamine intolerance.
Mast cells: Mast cell activation syndrome, genetics, and solutions
Mast cells are essential to your innate immune system, defending against pathogens and allergens. For some people, mast cells can be triggered too easily, giving allergy-like responses to lots of different substances.
Nrf2 Pathway: Increasing the body’s ability to get rid of toxins
The Nrf2 (Nuclear factor erythroid 2–related factor) signaling pathway regulates the expression of antioxidants and phase II detoxification enzymes. It is a fundamental pathway important in how well your body functions. Your genetic variants in the NFE2L2 gene impact this NRF2 pathway.
References:
Blunder, Stefan, et al. “Alterations in Epidermal Eicosanoid Metabolism Contribute to Inflammation and Impaired Late Differentiation in FLG-Mutated Atopic Dermatitis.” The Journal of Investigative Dermatology, vol. 137, no. 3, Mar. 2017, pp. 706–15. PubMed Central, https://doi.org/10.1016/j.jid.2016.09.034.
Brown, Sara J., et al. “Loss-of-Function Variants in the Filaggrin Gene Are a Significant Risk Factor for Peanut Allergy.” The Journal of Allergy and Clinical Immunology, vol. 127, no. 3, Mar. 2011, pp. 661–67. PubMed, https://doi.org/10.1016/j.jaci.2011.01.031.
Colagiovanni, A., et al. “Role of TNF-Alpha Polymorphism in Patients with Nickel Allergy: A Marker of Susceptibility to Contact Polysensitization.” European Review for Medical and Pharmacological Sciences, vol. 20, no. 12, June 2016, pp. 2663–66.
Das, Swastika, et al. “Nickel and Oxidative Stress: Cell Signaling Mechanisms and Protective Role of Vitamin C.” Endocrine, Metabolic & Immune Disorders Drug Targets, vol. 20, no. 7, 2020, pp. 1024–31. PubMed, https://doi.org/10.2174/1871530319666191205122249.
Di Gioacchino, Mario, et al. “Nickel Oral Hyposensitization in Patients with Systemic Nickel Allergy Syndrome.” Annals of Medicine, vol. 46, no. 1, Feb. 2014, pp. 31–37. PubMed Central, https://doi.org/10.3109/07853890.2013.861158.
Jacob, Sharon E., et al. “Nickel Allergy and Our Children’s Health: A Review of Indexed Cases and a View of Future Prevention.” Pediatric Dermatology, vol. 32, no. 6, 2015, pp. 779–85. PubMed, https://doi.org/10.1111/pde.12639.
Jiménez-Vidal, Luisa, et al. “Nuclear Factor Erythroid 2 – Related Factor 2 and Its Relationship with Cellular Response in Nickel Exposure: A Systems Biology Analysis.” BMC Pharmacology & Toxicology, vol. 20, no. Suppl 1, Dec. 2019, p. 78. PubMed Central, https://doi.org/10.1186/s40360-019-0360-4.
Ju, Hye Min, et al. “Correlation between Metal Ions and Cytokines in the Saliva of Patients with Oral Lichenoid Lesions.” Yonsei Medical Journal, vol. 62, no. 8, Aug. 2021, pp. 767–75. PubMed, https://doi.org/10.3349/ymj.2021.62.8.767.
Kim, Dae Suk, et al. “A Genome-Wide Association Study in Koreans Identifies Susceptibility Loci for Allergic Nickel Dermatitis.” International Archives of Allergy and Immunology, vol. 162, no. 2, 2013, pp. 184–86. www.karger.com, https://doi.org/10.1159/000353235.
Kuroishi, Toshinobu, et al. “Biotin Status Affects Nickel Allergy via Regulation of Interleukin-1beta Production in Mice.” The Journal of Nutrition, vol. 139, no. 5, May 2009, pp. 1031–36. PubMed, https://doi.org/10.3945/jn.108.097543.
Lombardi, Francesca, et al. “The Effects of Low-Nickel Diet Combined with Oral Administration of Selected Probiotics on Patients with Systemic Nickel Allergy Syndrome (SNAS) and Gut Dysbiosis.” Nutrients, vol. 12, no. 4, Apr. 2020, p. 1040. PubMed, https://doi.org/10.3390/nu12041040.
Margolis, David J., et al. “Uncommon Filaggrin Variants Are Associated with Persistent Atopic Dermatitis in African Americans.” The Journal of Investigative Dermatology, vol. 138, no. 7, July 2018, pp. 1501–06. PubMed, https://doi.org/10.1016/j.jid.2018.01.029.
“Nickel Allergies Symptoms, Tests, and Treatment.” Healthline, 7 May 2012, https://www.healthline.com/health/allergies/nickel.
“Nickel Allergy: Symptoms & Treatments.” Cleveland Clinic, https://my.clevelandclinic.org/health/diseases/17842-nickel-allergy. Accessed 28 Feb. 2023.
Noble, J., et al. “Nickel Allergy and Orthodontics, a Review and Report of Two Cases.” British Dental Journal, vol. 204, no. 6, Mar. 2008, pp. 297–300. PubMed, https://doi.org/10.1038/bdj.2008.198.
Novak, Natalija, et al. “Loss-of-Function Mutations in the Filaggrin Gene and Allergic Contact Sensitization to Nickel.” The Journal of Investigative Dermatology, vol. 128, no. 6, June 2008, pp. 1430–35. PubMed, https://doi.org/10.1038/sj.jid.5701190.
Randazzo, C. L., et al. “Probiotic Supplementation in Systemic Nickel Allergy Syndrome Patients: Study of Its Effects on Lactic Acid Bacteria Population and on Clinical Symptoms.” Journal of Applied Microbiology, vol. 118, no. 1, Jan. 2015, pp. 202–11. PubMed, https://doi.org/10.1111/jam.12685.
Ricciardi, L., et al. “Systemic Nickel Allergy Syndrome: Epidemiological Data from Four Italian Allergy Units.” International Journal of Immunopathology and Pharmacology, vol. 27, no. 1, 2014, pp. 131–36. PubMed, https://doi.org/10.1177/039463201402700118.
Riedel, Franziska, et al. “Immunological Mechanisms of Metal Allergies and the Nickel-Specific TCR-PMHC Interface.” International Journal of Environmental Research and Public Health, vol. 18, no. 20, Oct. 2021, p. 10867. PubMed Central, https://doi.org/10.3390/ijerph182010867.
Rishor-Olney, Colton R., and David M. Gnugnoli. “Nickel Allergy.” StatPearls, StatPearls Publishing, 2022. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK557638/.
Sharma, Ashimav D. “Low Nickel Diet in Dermatology.” Indian Journal of Dermatology, vol. 58, no. 3, 2013, p. 240. PubMed Central, https://doi.org/10.4103/0019-5154.110846.
Smieszek, S. P., et al. “Correlation of Age-of-Onset of Atopic Dermatitis with Filaggrin Loss-of-Function Variant Status.” Scientific Reports, vol. 10, no. 1, Feb. 2020, p. 2721. PubMed, https://doi.org/10.1038/s41598-020-59627-7.
Torres, Fernanda, et al. “Management of Contact Dermatitis Due to Nickel Allergy: An Update.” Clinical, Cosmetic and Investigational Dermatology : CCID, vol. 2, Apr. 2009, pp. 39–48. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3047925/.
Tramontana, Marta, et al. “Nickel Allergy: Epidemiology, Pathomechanism, Clinical Patterns, Treatment and Prevention Programs.” Endocrine, Metabolic & Immune Disorders Drug Targets, vol. 20, no. 7, 2020, pp. 992–1002. PubMed, https://doi.org/10.2174/1871530320666200128141900.
Wisgrill, Lukas, et al. “Integrative Transcriptome Analysis Deciphers Mechanisms of Nickel Contact Dermatitis.” Allergy, vol. 76, no. 3, Mar. 2021, pp. 804–15. PubMed Central, https://doi.org/10.1111/all.14519.