Key Takeaways:
~ Symptoms of Meniere’s disease include vertigo, constant ringing (tinnitus), and nausea.
~ Meniere’s can also cause pressure in the ear and possible hearing loss, most often striking people in their 40s and 50s.
~Tinnitus, or ringing in your ears, can be a problem, even without Meniere’s.
~ Research-backed solutions exist for Meniere’s and tinnitus — and these can be personalized based on your genes.
Meniere’s, tinnitus, and how the ear works:
Many health websites claim Meniere’s is a chronic condition with no cure and without an exact cause. [article, article] Recent research, though, paints a different picture, and genetics points to the root causes of Meniere’s and tinnitus.
Let’s start with some background information on how the ear works, and how a slight misfunction can cause problems with balance and ringing.
Your balance is coordinated by the change in motion of the fluid in the inner ear. It is like a built-in accelerometer that knows when you are in motion. Peripheral vertigo, or feeling dizzy and off-balance, is due to inner ear dysfunction. The sense of balance gets messed up by signals sent to the brain that don’t match reality.
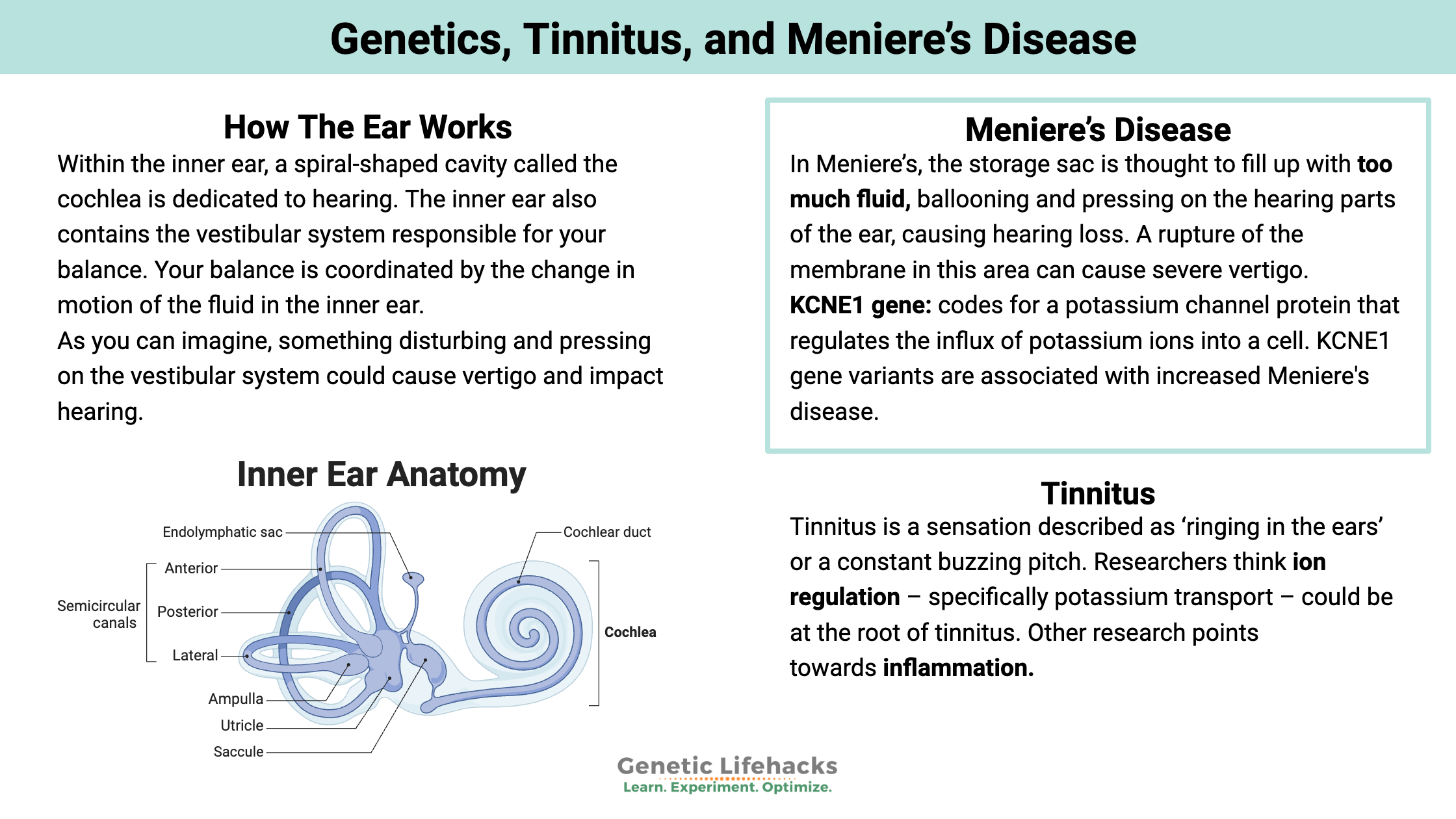
Within the inner ear, a spiral-shaped cavity called the cochlea is dedicated to hearing. Also, the inner ear contains the vestibular system responsible for your balance.[ref]
As you can imagine, something disturbing and pressing on the vestibular system could cause vertigo and impact hearing.
Endolymph is the fluid inside the inner ear. This fluid moves and transmits sounds, movement, etc., to the brain. The makeup of the ions in that fluid is essential for transmitting signals to the brain. The endolymph within the cochlea has a very low calcium (Ca2+) concentration, which allows for better mechanoelectrical transduction with the little hair cells in the cochlea.[ref]
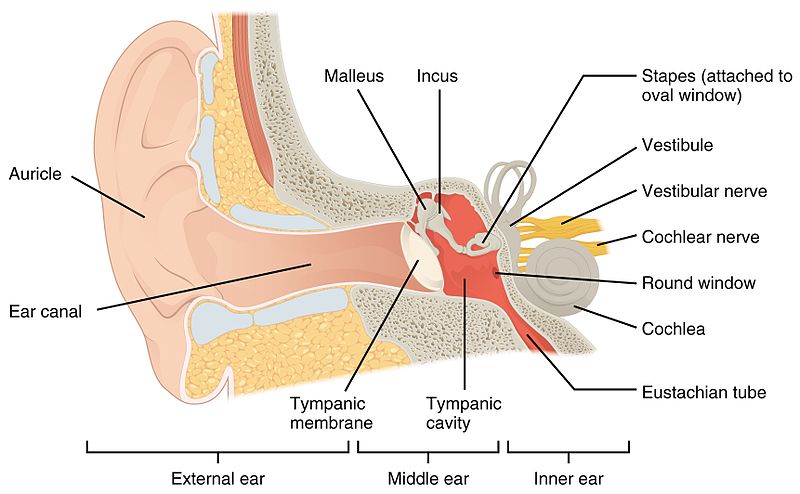
Here is a picture of the ear structure so you can visualize where the inner ear is – with the vestibular area and the cochlea. :
What goes wrong in the ear with Meniere’s disease?
Researchers think too much potassium (K+) in the inner ear causes too much endolymph in the vestibular organ. Any excess fluid is normally stored in an endolymphatic sac.
In Meniere’s, the storage sac is thought to fill up with too much fluid, ballooning and pressing on the hearing parts of the ear, causing hearing loss. A rupture of the membrane in this area can cause severe vertigo.
Often the symptoms in Meniere’s fluctuate, with the vertigo attacks suddenly becoming severe to the point of causing nausea and vomiting. The attacks sometimes may be preceded by changes in tinnitus, hearing, and the ear feeling full.[ref]
The membrane can heal up pretty quickly, leading to a cycle of increasing fluid and eventual rupture. Tinnitus and vertigo can fluctuate during the cycle when the fluid is building back up again.
Digging a little deeper:
So what do potassium and other ions have to do with fluid in the ear? Think back to osmosis experiments in high school science class… fluid can be drawn across a membrane to balance out ions.
The endolymph fluid has a different ion concentration and pH from the rest of the ear. The sodium concentration is higher, and the potassium and chloride concentrations are lower. Researchers think the ion gradient gets messed up (too much potassium), which is then balanced out with more fluid, causing swelling.
The cells surrounding the endolymphatic sac have receptors activated by cortisol and receptors sensitive to aldosterone. This ties Meniere’s to blood pressure and stress:
- Aldosterone is the hormone that controls the absorption of salt in the kidneys and is important in blood pressure.[ref]
- Cortisol is released by the adrenal glands when the body is stressed.
However, may not be the whole story for Meniere’s disease. Researchers note that some people have swelling within the endolymph system and don’t have the symptoms of Meniere’s. They also question whether the swelling can actually cause vertigo.[ref] Questions remain on what triggers Meniere’s.
Theories on the cause(s) of Meniere’s Disease:
The symptoms and progression of the disease vary a lot from person to person, making any single root cause of Meniere’s disease hard to pin down. Some scientists postulate that Meniere’s is an autoimmune condition due to elevated antibody titers and higher levels of circulating immune complexes. People with autoimmune diseases are also more likely to have more severe Meniere’s disease.[ref][ref] Certain HLA serotypes are associated with an increased risk of Meniere’s disease, adding to the evidence that it is autoimmune-related.[ref]
Other researchers point to Meniere’s being multifactorial, with causes including adrenal insufficiency, hypothyroidism, narrowing of the inner auditory canal, trauma, and allergies.[ref]
Genetic mutations and a familial aspect of Meniere’s disease are other lines of investigation.[ref] The genetic variants linked with Meniere’s point towards the body’s immune and inflammatory response as well as potassium regulation.
All of these, when taken together, point to a system that is out of balance.
Conditions that overlap with Meniere’s:
Meniere’s disease is linked to an increased risk of both migraines and motion sickness.[ref] In fact, migraine prevalence in Meniere’s is double that of the population in general.[ref] One study found that Meniere’s patients who didn’t respond to diuretics were more likely to respond to medications used to prevent migraines.[ref]
People with rheumatoid arthritis have a (slightly) increased risk of Meniere’s disease.[ref]
A study of patients with Meniere’s disease found that 1/3 were clinically hypothyroid. Treating them with thyroid medication improved Meniere’s symptoms in all of the hypothyroid patients.[ref]
Allergies and histamine intolerance are also linked to Meniere’s
Tinnitus:
Tinnitus is a sensation described as ‘ringing in the ears’ or a constant buzzing pitch. In addition to being a symptom of Meniere’s disease, tinnitus can also accompany other hearing loss diseases or can occur spontaneously.
It is thought to affect up to 15% of adults at some point in their lives, affecting both their quality of life and mental health.
What causes tinnitus?
Ions and nerve transmission:
Researchers think ion regulation – specifically potassium transport – could be at the root of tinnitus. Potassium (K+) and sodium (Na+) ions are thought to cause tinnitus by altering the electrical activity of neurons in the auditory pathway. The abnormal neuronal activity then leads to the perception of phantom sounds.[ref]
Genetic variants related to glutamate receptors are associated with an increased relative risk of tinnitus. Glutamate is an excitatory neurotransmitter, and excess glutamate signaling can lead to excitotoxicity and nerve damage.[ref]
Excess inflammation in the neurons of the ear:
TNF-alpha:
New studies using animal models of hearing impairment show that neuroinflammation may be a part of the picture for tinnitus and hearing loss. Blocking TNF-α prevents neuroinflammation and tinnitus in a mouse model. TNF-alpha is an inflammatory cytokine that is elevated in response to a bunch of different triggers – from infections to oxidative stress.[ref]
IL-1B:
Other studies point to IL-1B (interleukin 1 beta), a proinflammatory cytokine, as a risk factor.[ref] Studies show that higher IL-1B levels correlate with higher loudness perception in tinnitus, and that higher TNF-alpha levels also are correlated with the grade of tinnitus.[ref]
IL-10:
IL-10 is another part of the inflammatory response, and low levels of IL-10 can lead to higher levels of other inflammatory cytokines. A 2019 study in Portuguese adults found that IL10 was lower in tinnitus patients. IL-10 (interleukin 10) is an anti-inflammatory cytokine that limits your body’s inflammatory response. Thus, low IL-10 levels can lead to higher inflammation. Accordingly, the researchers found that IL-1a, an inflammatory cytokine, was higher in participants with tonal tinnitus.[ref]
Gum disease and inflammation:
People with periodontitis – inflamed gums – are statistically more likely to have tinnitus.[ref] Research shows that genetic variants linked to higher inflammatory cytokines are strongly linked to periodontitis and gingivitis.
Related article: Gum Disease, Inflammation, and Genetics
Is tinnitus genetic?
Genetic susceptibility is partly to blame for tinnitus, but it doesn’t act alone. Environmental and lifestyle factors that cause inflammation are also important here.
Researchers often study twins, siblings, and adoptees to determine whether a condition, such as tinnitus, is heritable, indicating it has a genetic component. In a large study in Sweden, researchers discovered that adoptees with a biological parent with tinnitus were over twice as likely to have tinnitus, showing a strong genetic susceptibility. The researchers also noted no association between tinnitus in an adopted parent and the adoptee, thus making the environment a less likely factor.[ref]
Genetic polymorphisms in genes related to inflammatory cytokines, potassium channels, blood pressure regulation, and histamine have been identified in studies as increasing the risk of tinnitus and Meniere’s. You’ll find these genes below in the Genotype Report section.
Salicylates and tinnitus:
In animal research, sodium salicylate, the sodium salt of salicylic acid (aspirin), is often given to animals to create tinnitus. Higher doses of aspirin can cause (or worsen) tinnitus in some people. Animal studies have shown that salicylate blocks a certain type of calcium channel in the inner ear. It could then cause decreased GABA, an inhibitory neurotransmitter, in the inner ear.[ref]
The thought here is that not enough inhibition = constant firing of the neurons and tinnitus. GABA inhibits excess firing, while glutamate can increase the neuron’s firing potential. Thus, alternatively, the salicylate could increase the neurons’ firing rate in the auditory nerve complex.[ref]
Brain involvement in tinnitus:
While tinnitus may be caused by changes in ion channels or neuron firing in the auditory canal, another possibility is that something is going wrong in the way the brain is interpreting the signal.
GABA is an inhibitory neurotransmitter found in the cortex of the brain. In mice, reducing GABA production in specific areas of the brain can induce tinnitus, and similarly, enhancing GABA can eliminate tinnitus. Thus, researchers think that loss of cortical GABA inhibition is a cause of tinnitus.[ref]
Meniere’s and Tinnitus Genotype Report:
This genotype report section is divided into two sections: Meniere’s genetic variants and Tinnitus genetic variants.
Lifehacks: Natural solutions for Meniere’s and Tinnitus:
Modulating NF-κB for NFKB1 variants:
NF-κB is a transcription factor that is responsible for activating and controlling the immune response.[ref] The genetic variants in the NFKB1 and the intergenic region show a definite link between NF-κB (nuclear factor – kappa beta) and Meniere’s disease for some people.
NF-κB is activated by cytokines such as TNFα and IL-1β. Thus, targeting chronic inflammation may help with Meniere’s.
Related Article: TNFα and inflammation lifehacks
Mold has been shown in one study to trigger “a significant release of TNF-α in [Meniere’s Disease] patients, which were not found in controls.”[ref] Consider testing your home and workplace for mold and getting mold remediation done if needed.
Related article: Mycotoxin and Mold Detoxification Genes
Heat therapy, such as sauna, increases heat shock proteins. This increase in heat shock proteins then helps modulate inflammatory stress by decreasing the activation of NF-κB.[ref] Specifically, repeatedly activating heat shock protein 70 (Hsp70) leads “to the inactivation of downstream of nuclear factor-κB (NF-κB) inflammation signaling pathway.”[ref]
You may be wondering if there is any clinical evidence that sauna decreases the symptoms of Meniere’s disease… This doesn’t seem to be well-studied. One case study from 1977 showed that sauna visits improved Meniere’s disease for the two participants.[ref]
Related Articles and Topics:
TNF-alpha: Inflammation, Chronic Diseases, and Genetic Susceptibility
References:
Abtahi, Seyed Hamidreza, et al. “Comparison of Melatonin and Sertraline Therapies on Tinnitus: A Randomized Clinical Trial.” International Journal of Preventive Medicine, vol. 8, 2017, p. 61. PubMed, https://doi.org/10.4103/ijpvm.IJPVM_229_17.
Ban, Ju Yeon, et al. “Microarray Analysis of Gene Expression Profiles in Response to Treatment with Melatonin in Lipopolysaccharide Activated RAW 264.7 Cells.” The Korean Journal of Physiology & Pharmacology : Official Journal of the Korean Physiological Society and the Korean Society of Pharmacology, vol. 15, no. 1, Feb. 2011, pp. 23–29. PubMed Central, https://doi.org/10.4196/kjpp.2011.15.1.23.
Brunt, Vienna E., et al. “Passive Heat Therapy Protects against Endothelial Cell Hypoxia-Reoxygenation via Effects of Elevations in Temperature and Circulating Factors.” The Journal of Physiology, vol. 596, no. 20, Oct. 2018, pp. 4831–45. PubMed, https://doi.org/10.1113/JP276559.
Büki, Béla, et al. “The Price of Immune Responses and the Role of Vitamin D in the Inner Ear.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology, vol. 40, no. 6, July 2019, pp. 701–09. PubMed, https://doi.org/10.1097/MAO.0000000000002258.
Büki, Bela, et al. “Vitamin D Supplementation May Improve Symptoms in Meniere’s Disease.” Medical Hypotheses, vol. 116, July 2018, pp. 44–46. PubMed Central, https://doi.org/10.1016/j.mehy.2018.04.019.
Cabrera, Sonia, et al. “Intronic Variants in the NFKB1 Gene May Influence Hearing Forecast in Patients with Unilateral Sensorineural Hearing Loss in Meniere’s Disease.” PloS One, vol. 9, no. 11, 2014, p. e112171. PubMed, https://doi.org/10.1371/journal.pone.0112171.
Cederroth, Christopher R., et al. “Association of Genetic vs Environmental Factors in Swedish Adoptees With Clinically Significant Tinnitus.” JAMA Otolaryngology– Head & Neck Surgery, vol. 145, no. 3, Mar. 2019, pp. 222–29. PubMed, https://doi.org/10.1001/jamaoto.2018.3852.
Cronometer: Track Nutrition & Count Calories. https://cronometer.com/. Accessed 13 Apr. 2022.
Dabiri, Sasan, et al. “HLA-Cw Allele Frequency in Definite Meniere’s Disease Compared to Probable Meniere’s Disease and Healthy Controls in an Iranian Sample.” Iranian Journal of Otorhinolaryngology, vol. 28, no. 87, July 2016, pp. 262–66.
Ding, Jing, et al. “Serum Levels of 25-Hydroxy Vitamin D Correlate with Idiopathic Benign Paroxysmal Positional Vertigo.” Bioscience Reports, vol. 39, no. 4, Apr. 2019, p. BSR20190142. PubMed Central, https://doi.org/10.1042/BSR20190142.
Doi, Katsumi, et al. “Ménière’s Disease Is Associated with Single Nucleotide Polymorphisms in the Human Potassium Channel Genes, KCNE1 and KCNE3.” ORL; Journal for Oto-Rhino-Laryngology and Its Related Specialties, vol. 67, no. 5, 2005, pp. 289–93. PubMed, https://doi.org/10.1159/000089410.
Frejo, Lidia, Alvaro Gallego-Martinez, et al. “Proinflammatory Cytokines and Response to Molds in Mononuclear Cells of Patients with Meniere Disease.” Scientific Reports, vol. 8, no. 1, Apr. 2018, p. 5974. PubMed, https://doi.org/10.1038/s41598-018-23911-4.
Frejo, Lidia, Teresa Requena, et al. “Regulation of Fn14 Receptor and NF-ΚB Underlies Inflammation in Meniere’s Disease.” Frontiers in Immunology, vol. 8, Dec. 2017, p. 1739. PubMed Central, https://doi.org/10.3389/fimmu.2017.01739.
Furuta, T., et al. “Association of Interleukin-1 Gene Polymorphisms with Sudden Sensorineural Hearing Loss and Ménière’s Disease.” International Journal of Immunogenetics, vol. 38, no. 3, June 2011, pp. 249–54. PubMed, https://doi.org/10.1111/j.1744-313X.2011.01004.x.
Gazquez, Irene, et al. “High Prevalence of Systemic Autoimmune Diseases in Patients with Menière’s Disease.” PloS One, vol. 6, no. 10, 2011, p. e26759. PubMed, https://doi.org/10.1371/journal.pone.0026759.
Ghavami, Yaser, et al. “Evaluating Quality of Life in Patients With Meniere’s Disease Treated as Migraine.” The Annals of Otology, Rhinology, and Laryngology, vol. 127, no. 12, Dec. 2018, pp. 877–87. PubMed, https://doi.org/10.1177/0003489418799107.
Golding, John F., and Mitesh Patel. “Meniere’s, Migraine, and Motion Sickness.” Acta Oto-Laryngologica, vol. 137, no. 5, May 2017, pp. 495–502. Taylor and Francis+NEJM, https://doi.org/10.1080/00016489.2016.1255775.
Haider, Haúla F., et al. “Tinnitus, Hearing Loss and Inflammatory Processes in an Older Portuguese Population.” International Journal of Audiology, vol. 59, no. 5, Apr. 2020, pp. 323–32. Taylor and Francis+NEJM, https://doi.org/10.1080/14992027.2019.1698775.
Herman, L. E., et al. “Diaphoresis and Meniere’s Disease.” Archives of Otolaryngology (Chicago, Ill.: 1960), vol. 103, no. 12, Dec. 1977, pp. 700–04. PubMed, https://doi.org/10.1001/archotol.1977.00780290036002.
Hietikko, Elina, Jouko Kotimäki, et al. “A Replication Study on Proposed Candidate Genes in Ménière’s Disease, and a Review of the Current Status of Genetic Studies.” International Journal of Audiology, vol. 51, no. 11, Nov. 2012, pp. 841–45. PubMed, https://doi.org/10.3109/14992027.2012.705900.
Hietikko, Elina, Martti Sorri, et al. “Higher Prevalence of Autoimmune Diseases and Longer Spells of Vertigo in Patients Affected with Familial Ménière’s Disease: A Clinical Comparison of Familial and Sporadic Ménière’s Disease.” American Journal of Audiology, vol. 23, no. 2, June 2014, pp. 232–37. PubMed, https://doi.org/10.1044/2014_AJA-13-0060.
Hussain, Kiran, et al. “Restriction of Salt, Caffeine and Alcohol Intake for the Treatment of Ménière’s Disease or Syndrome.” The Cochrane Database of Systematic Reviews, vol. 2018, no. 12, Dec. 2018, p. CD012173. PubMed Central, https://doi.org/10.1002/14651858.CD012173.pub2.
Ledesma, Alleluia Lima Losno, et al. Caffeine and Meniere’s Disease. IntechOpen, 2017. www.intechopen.com, https://doi.org/10.5772/intechopen.69667.
Li, Yan, et al. “Cardiovascular Risk in Relation to Alpha-Adducin Gly460Trp Polymorphism and Systolic Pressure: A Prospective Population Study.” Hypertension (Dallas, Tex.: 1979), vol. 46, no. 3, Sept. 2005, pp. 527–32. PubMed, https://doi.org/10.1161/01.HYP.0000174988.81829.72.
Liu, Yanxing, et al. “Salicylate Blocks L-Type Calcium Channels in Rat Inferior Colliculus Neurons.” Hearing Research, vol. 205, no. 1–2, July 2005, pp. 271–76. PubMed, https://doi.org/10.1016/j.heares.2005.03.028.
Lopes, Karen de Carvalho, et al. “Ménière’s Disease: Molecular Analysis of Aquaporins 2, 3 and Potassium Channel KCNE1 Genes in Brazilian Patients.” Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology, vol. 37, no. 8, Sept. 2016, pp. 1117–21. PubMed, https://doi.org/10.1097/MAO.0000000000001136.
Lopez-Escamez, Jose A., et al. “Association of a Functional Polymorphism of PTPN22 Encoding a Lymphoid Protein Phosphatase in Bilateral Meniere’s Disease: PTPN22 Encoding in Meniere’s Disease.” The Laryngoscope, vol. 120, no. 1, Jan. 2010, pp. 103–07. DOI.org (Crossref), https://doi.org/10.1002/lary.20650.
Lopez-Escamez, Jose Antonio, et al. “Towards Personalized Medicine in Ménière’s Disease.” F1000Research, vol. 7, Aug. 2018, p. F1000 Faculty Rev-1295. PubMed Central, https://doi.org/10.12688/f1000research.14417.1.
Marchiori, Luciana Lozza de Moraes, et al. “Interleukin-1 Alpha Gene Polymorphism (IL-1α) and Susceptibility to Tinnitus in the Elderly.” Noise & Health, vol. 21, no. 99, 2019, pp. 77–82. PubMed Central, https://doi.org/10.4103/nah.NAH_67_18.
Megwalu, Uchechukwu C., et al. “The Effects of Melatonin on Tinnitus and Sleep.” Otolaryngology–Head and Neck Surgery: Official Journal of American Academy of Otolaryngology-Head and Neck Surgery, vol. 134, no. 2, Feb. 2006, pp. 210–13. PubMed, https://doi.org/10.1016/j.otohns.2005.10.007.
Meniere’s Disease. https://medlineplus.gov/menieresdisease.html. Accessed 13 Apr. 2022.
“Meniere’s Disease – Causes, Symptoms, Treatments.” Healthy Hearing, https://www.healthyhearing.com/help/tinnitus/menieres-disease. Accessed 13 Apr. 2022.
Mori, Nozomu, et al. “Ion Transport Its Regulation in the Endolymphatic Sac: Suggestions for Clinical Aspects of Meniere’s Disease.” European Archives of Oto-Rhino-Laryngology, vol. 274, no. 4, 2017, pp. 1813–20. PubMed Central, https://doi.org/10.1007/s00405-016-4362-1.
Nakashima, Tsutomu, et al. “Meniere’s Disease.” Nature Reviews Disease Primers, vol. 2, no. 1, May 2016, pp. 1–18. www.nature.com, https://doi.org/10.1038/nrdp.2016.28.
Qin, Danxia, et al. “Histamine H4 Receptor Gene Polymorphisms: A Potential Contributor to Meniere Disease.” BMC Medical Genomics, vol. 12, no. 1, May 2019, p. 71. PubMed, https://doi.org/10.1186/s12920-019-0533-4.
Sand, Philipp G., et al. “Deep Resequencing of the Voltage-Gated Potassium Channel Subunit KCNE3 Gene in Chronic Tinnitus.” Behavioral and Brain Functions : BBF, vol. 7, Sept. 2011, p. 39. PubMed Central, https://doi.org/10.1186/1744-9081-7-39.
Santosh, U. P., and M. S. Sudhakar Rao. “Incidence of Hypothyroidism in Meniere’s Disease.” Journal of Clinical and Diagnostic Research : JCDR, vol. 10, no. 5, May 2016, pp. MC01–3. PubMed Central, https://doi.org/10.7860/JCDR/2016/17587.7759.
Scuto, Maria, et al. “Nutritional Mushroom Treatment in Meniere’s Disease with Coriolus Versicolor: A Rationale for Therapeutic Intervention in Neuroinflammation and Antineurodegeneration.” International Journal of Molecular Sciences, vol. 21, no. 1, Dec. 2019, p. 284. PubMed Central, https://doi.org/10.3390/ijms21010284.
Tan, Dun-Xian, et al. “Melatonin as a Potent and Inducible Endogenous Antioxidant: Synthesis and Metabolism.” Molecules, vol. 20, no. 10, Oct. 2015, pp. 18886–906. PubMed Central, https://doi.org/10.3390/molecules201018886.
Wang, Li-Chao, et al. “Highly Selective Activation of Heat Shock Protein 70 by Allosteric Regulation Provides an Insight into Efficient Neuroinflammation Inhibition.” EBioMedicine, vol. 23, Aug. 2017, pp. 160–72. PubMed Central, https://doi.org/10.1016/j.ebiom.2017.08.011.
Wang, Weihua, et al. “Neuroinflammation Mediates Noise-Induced Synaptic Imbalance and Tinnitus in Rodent Models.” PLoS Biology, vol. 17, no. 6, June 2019, p. e3000307. PubMed Central, https://doi.org/10.1371/journal.pbio.3000307.
Weinreich, Heather M., and Yuri Agrawal. “The Link Between Allergy and Menière’s Disease.” Current Opinion in Otolaryngology & Head and Neck Surgery, vol. 22, no. 3, June 2014, pp. 227–30. PubMed Central, https://doi.org/10.1097/MOO.0000000000000041.
Wu, Cong, et al. “Changes in GABA and Glutamate Receptors on Auditory Cortical Excitatory Neurons in a Rat Model of Salicylate-Induced Tinnitus.” American Journal of Translational Research, vol. 10, no. 12, Dec. 2018, pp. 3941–55. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6325520/.
Yuce, Salim, et al. “Angiotensin-Converting Enzyme (ACE) I/D and Alpha-Adducin (ADD1) G460W Gene Polymorphisms in Turkish Patients with Severe Chronic Tinnitus.” The Journal of International Advanced Otology, vol. 12, no. 1, Apr. 2016, pp. 77–81. PubMed, https://doi.org/10.5152/iao.2016.1732.