Key Takeaways:
~ Rosacea is an inflammatory skin condition that causes facial redness.
~ Increased inflammatory activation due to various environmental factors causes redness, increased vascularization, and altered skin permeability.
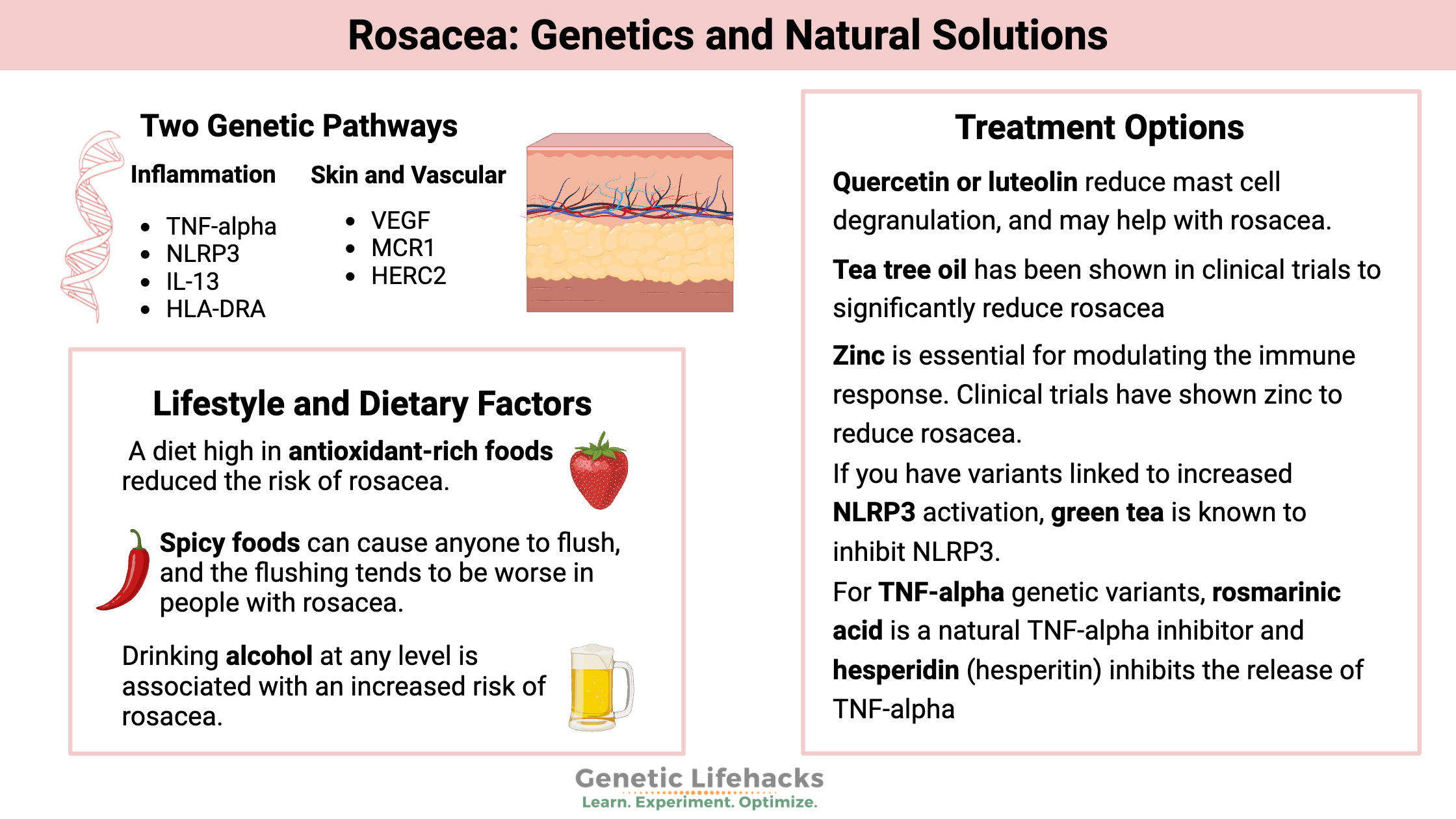
~ Genetic variants associated with increased inflammation and vascularization are associated with rosacea.
~ Understanding your genetic susceptibility can help you find the right solution for your skin.
Members will see their genotype report below, plus additional solutions in the Lifehacks section. Consider joining today.
What is rosacea?
Rosacea is a chronic, inflammatory skin condition on the face that causes redness and irritation. It is three times more common on the cheeks and chin in women than men, while men are more likely to have the nose affected.
Activation of the immune system and vascular changes are at the heart of rosacea. Genetic variants play a role in susceptibility, of course, as does the skin microbiome. Research studies also show that there are a lot of ways to put rosacea into remission. Not every treatment or lifestyle change works for everyone, so it can take a bit of experimentation to figure out what works for you.
The key takeaway here is that understanding your genetic variants and their role in inflammation and skin permeability may point you toward the right solutions for your skin.
Let’s take a look at the research on what causes rosacea, how it is defined, and the genetic variants that increase susceptibility.
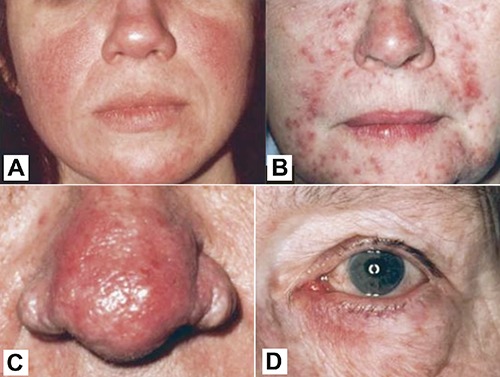
Four subtypes of rosacea:
Rosacea is divided into four types, each with different characteristics:
- Erythematotelangiectatic rosacea: facial flushing, redness, visible capillaries
- Papulopustular rosacea: facial redness with inflammatory bumps that kind of look like acne
- Rhinophyma (phymatous rosacea): thickened, red skin on the nose that may be bumpy, waxy, and have visible blood vessels
- Ocular rosacea: watery, bloodshot eyes with redness on the eyelids.
Rosacea doesn’t always fit neatly into categories. Many people have multiple subtypes or fluctuate between types.[ref]
Burning, stinging, and overly sensitive skin also comes with rosacea, making it difficult to find skincare solutions that help rather than aggravate the condition.
People with rosacea often have visible small blood vessels close to the skin. This is called telangiectasia – the small, dilated blood vessels that are usually visible on the nose and cheeks.
Red, bumpy nose in older men: Rhinophyma
Rhinophyma is the name given to a red, bumpy, thickened nose that is often seen in men over the age of 50. Many people think it is caused by drinking too much alcohol, but it is actually a type of rosacea.
I think this is a change that older men overlook because they don’t know what’s causing it — and they likely don’t know that there are readily available treatments for it.
Cause of rosacea:
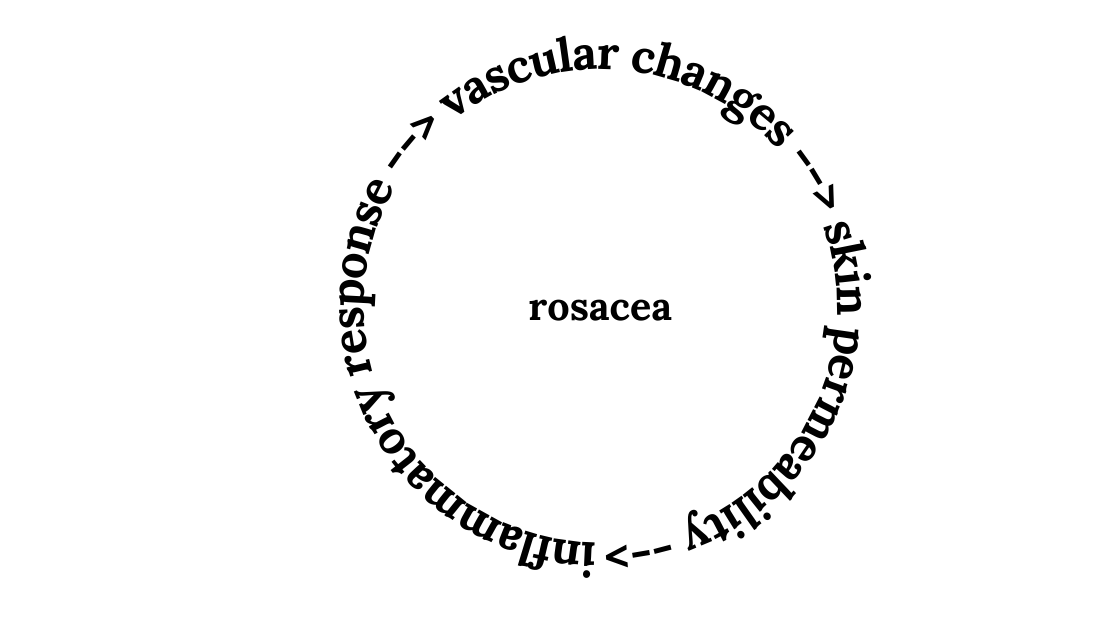
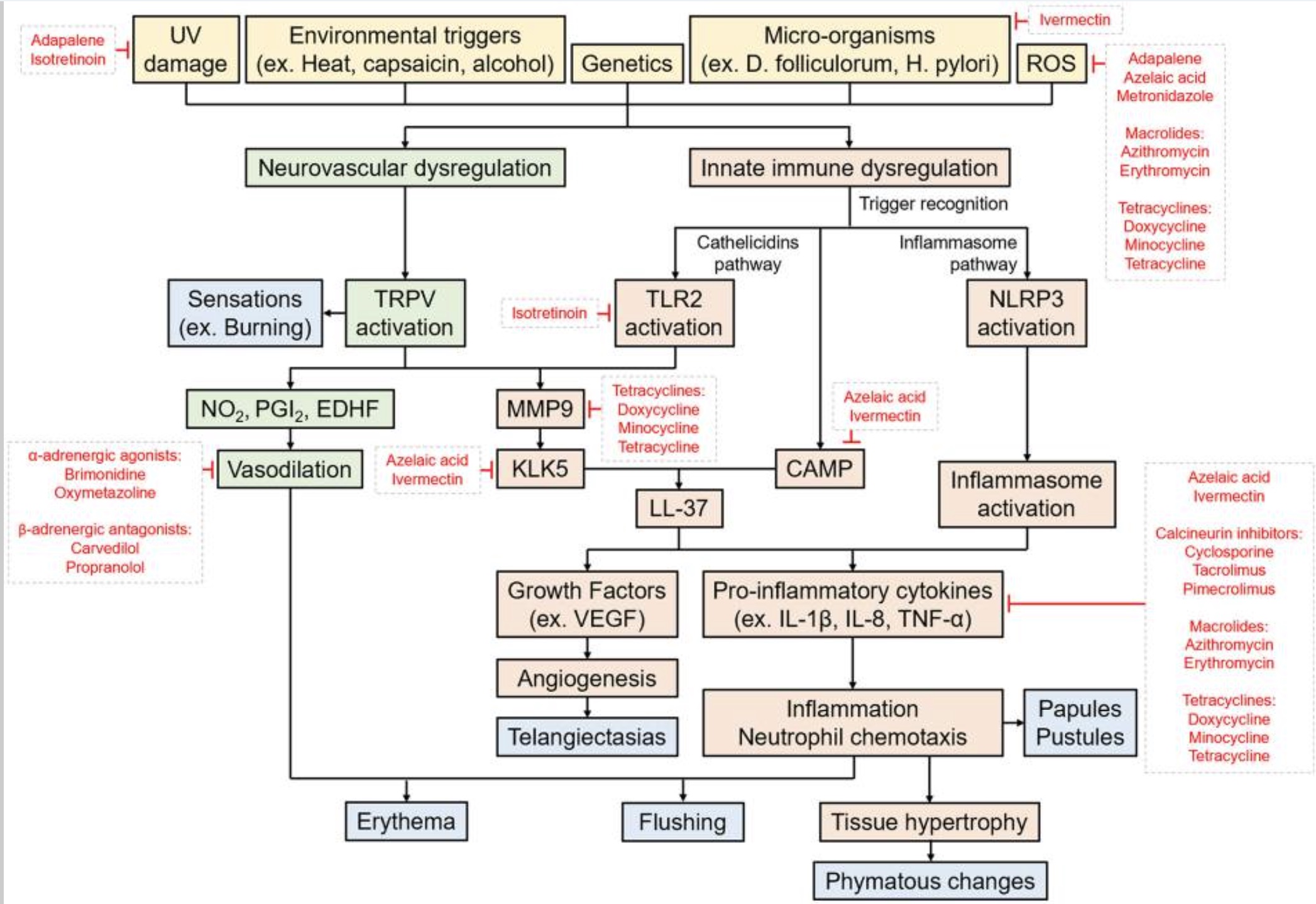
Research reveals that the cause of rosacea is a combination of overactivation of inflammatory pathways, changes in tiny blood vessels of the face, and changes in the tight junctions between skin cells.
Overactivation of inflammatory pathways includes the activation of toll-like receptors (TLR2) and the activation of mast cells. The activation of mast cells releases histamine, which causes blood vessel dilation and permeability. Inflammation increases skin permeability, leading to more irritation from environmental factors and the skin microbiome, feeding into more inflammatory cytokine production.
Let’s dig into the details of each of these components of rosacea.
Inflammation and immune system dysfunction:
In rosacea, there is an overactive response in the immune system that reacts to environmental and microbial factors on the skin. Many studies show that cathelicidin, an antimicrobial peptide, is overactive in rosacea, and it can trigger a cascade of inflammatory processes including mast cell activation. Kallikrein (KLK) 5 is the main serine protease that converts cathelicidin into LL37, the active version of cathelicidin that is abundant in rosacea skin. [ref]
Mast cells :
Mast cells are part of the immune system’s first line of defense against invaders. Activation of mast cells causes the release of histamine and other vasodilators and inflammatory cytokines, such as in allergic reactions. Mast cells are abundant in areas of the body exposed to foreign invaders, such as the skin, lungs, and intestines.
The MRGPRX2 receptor on mast cells is activated by cathelicidin, triggering inflammation and vasodilation. Animal studies show that when the MRGPRX2 receptor on mast cells is blocked, rosacea doesn’t develop.
Related article: MRGBRX2 receptor, genetics
TRPV channels:
Research shows that TRPV channels are also upregulated in rosacea. TRPV channels are ion channel receptors found throughout the body with a number of different functions, such as sensing pain or temperature. The TRPV4 ion channel has been specifically linked to rosacea and is upregulated in the skin where rosacea occurs. TRPV4 is activated by heat and also interacts with mast cells to send signals based on inflammation. Activation of TRPV can increase blood vessel formation as well as send the signal for the burning or irritated skin sensation.[ref]
TLR4, TLR2, and oxidative stress:
Toll-like receptor 4 (TLR4) is also elevated in rosacea, particularly in ocular rosacea. Oxidative stress (high ROS) is also implicated in causing ocular rosacea.[ref] Toll-like receptor 2 (TLR2) is also found to be upregulated in the skin of rosacea patients. Activation of TLR2 leads to the production of cathelicidin (and LL37).[ref]
Toll-like receptors are part of the immune system activation. TLR4 and TLR2 recognize bacteria as being foreign and mount an inflammatory response against them.
NLRP3 inflammasome activation:
Recent research suggests that the NLRP3 inflammasome pathway, which causes inflammation to be generally upregulated in tissues, is involved in rosacea. Importantly, NLRP3 inhibitors have been shown to reduce rosacea symptoms.
Related article: NLRP3, genes and elevated inflammation
Recap: All of this comes together in the ways that inflammatory pathways interact. Activation of toll-like receptors leads to cathelicidin production. Cathelicidin activates the MRGPRX2 receptor on mast cells. Mast cells release histamine and inflammatory cytokines causing vasodilation and triggering an inflammatory cascade. TRPV channels alongside mast cells are activated, triggering pain and blood vessel formation, and TRPV channels on mast cells can be activated by heat, triggering mast cell degranulation.
Blood flow, vasodilation:
In addition to inflammation, rosacea is known for redness and small capillaries that appear on the surface of the skin. Part of the inflammatory process is increased blood flow and the growth of small blood vessels near the surface of the facial skin.
Inflammatory factors, including cathelicidins and TNF-alpha, lead to increased vascularization. Histamine released from mast cells also increases vasodilation.[ref]
The increased blood vessels near the surface of the skin cause the redness, flushing, and visible blood vessels in rosacea.
Skin barrier:
A recent study showed that people with rosacea have a more permeable skin barrier than normal. The study looked at the tight junctions and the depth of permeability in rosacea skin and found that there was increased permeability at 8μm on the face.[ref] Another study explains that in rosacea, certain pathways related to the skin barrier are altered so that the permeability is increased. In people with papulopustular rosacea, the skin barrier alterations were found near sebaceous (oil) glands and hair follicles. [ref]
Triggers and environmental factors:
What triggers immune system activation? This is where environmental factors come into play.
The skin microbiome is altered in rosacea, and microscopic skin mites are often increased. This is combined with environmental triggers that worsen or flare rosacea, including UV radiation (sunburn), wind, extreme heat or cold, and air pollution. Diet, stress, and alcohol, all of which affect overall systemic inflammation, can make rosacea worse. Exposure to certain skin care products may also come into play – all of which comes back to the interaction with skin microbes and the inflammatory response.
Skin microbiome in rosacea:
It makes sense that the skin microbiome can play a role in the inflammation seen in rosacea. We all have bacteria on our skin, and there is a balance between healthy skin, microbes, and immune response.
A study in twin pairs, where one had rosacea and the other didn’t, clearly shows the role of bacteria in activating the inflammatory response. The study showed that there were changes in the levels of certain genera of bacteria that are found in low abundance on normal skin. There was an increase in Gordonia species and a decrease in Geobacillus species in rosacea.[ref]
Other studies have also found that the skin microbiome is altered in people with rosacea. The studies found that certain bacterial species are depleted, while other normal skin bacteria are overabundant.[ref]
Demodex mites:
In addition to microbes on the skin, most people also have microscopic mites on their skin and hair follicles. While this is usually tolerated at some level, researchers believe that Demodex mite infestations cause inflammation in papulopustular rosacea.[ref]
A study of 242 patients with face papulopustules showed that the density of Demodex mites was associated with facial redness and papulopustules.[ref] Other studies point to a combination of Demodex mites along with certain bacteria that live on the mites.[ref]
Skin mites and bacteria on the skin are normal (whether we like to think about it or not). However, the difference in rosacea is that the immune response to the mites and certain bacteria is different from normal. There’s an over-activation of inflammation, which then causes a cascade of events that leads to redness, irritation, skin permeability, and increased capillaries.
Environmental triggers:
Exposure to UV rays can make rosacea worse for some people. UV radiation can increase oxidative stress in cells. Cold or heat is another common environmental trigger.
Cosmetics and skin care products can often irritate and worsen rosacea symptoms. One study showed that rosacea patients with a more permeable skin barrier had increased skin irritation to common skin care ingredients such as sodium lauryl sulfate.[ref]
Here’s a schematic drawing from a review article summing up the causes and pathways involved in rosacea:[ref]
Overall inflammation:
Increased inflammatory cytokines throughout the body may worsen rosacea.
- People with autoimmune diseases, alcohol abuse disorder, obesity, and diabetes are at an increased relative risk of rosacea.[ref]
- Smoking or being a former smoker increases the risk of rosacea by 2-fold.[ref]
- People with inflammatory bowel disease are at a higher risk of rosacea.[ref]
The flip side is also true. Reducing systemic inflammation reduces rosacea symptoms and risk. For example, eating a healthy diet rich in antioxidants reduces the risk of rosacea by more than 40%. [ref]
Genetic studies on rosacea:
Twin studies show that genetics play a role in who gets rosacea. One study showed about a 46% genetic contribution to rosacea.[ref]
Genes interact with environmental factors to trigger rosacea symptoms. For example, Demodex mites are commonly found on the skin and usually don’t cause an immune system response. However, higher levels of the mites upregulate TLR2 and trigger an immune response in some people who tend to have higher levels of inflammatory cytokines.[ref]
A 23andMe study found that several genetic variants related to increased inflammatory response were linked to rosacea risk. Additionally, melanocortin receptor (MC1R) variants also increased the relative risk of rosacea. The MC1R gene encodes a receptor found in skin cells that produce melanin.[ref]
Vitamin D:
There are two types of vitamin D in the body – 25-hydroxyvitamin D3 [25(OH)D3 ] which is the inactive form and 1,25(OH)2D3 or calcitriol which is the active form. Vitamin D acts by binding to the vitamin D receptor (VDR) and activating the transcription of other genes. In the immune system, vitamin D can both increase the immune response, e.g. to a bacteria or pathogen, and it can modulate the immune response, such as in autoimmune diseases.
Serum 25(OH)D3 levels show the inactive form of vitamin D, which can be from supplements or from sun exposure. A study of 60 rosacea patients and 60 age and sex-matched healthy controls showed that high serum 25(OH)D3 levels were associated with a 36% increased risk of rosacea.[ref] However, another study found that having vitamin D above 25ng/dl decreased the risk of rosacea.[ref] Both studies showed that vitamin D receptor variants influence the risk of rosacea.
Genotype report:
This section covers the more common genetic variants that increase susceptibility to rosacea. There are also a handful of rare mutations that are linked to rosacea, but these aren’t included in 23andMe or AncestryDNA data.[ref] I’ve divided this into genetic variants related to inflammation and then genetic variants related to vasculature and skin formation.
Lifehacks:
A dermatologist should be able to help you with your rosacea, and this is the first place most people start when looking for treatment options. The only FDA-approved oral treatment is a low dose of doxycycline, an antibiotic, but there are many other prescription topical treatments that a dermatologist can help you with. Topical options include antibiotics, antihistamines, and mite killers. For example, ivermectin is used for rosacea because it kills skin mites and reduces TNF-alpha. Some doctors prescribe beta-blockers to reduce the redness.[ref][ref]
However, with multiple underlying causes of inflammation, many times rosacea patients will end up trying multiple topical options before they figure out what works.
Again, this schematic of the pathways involved in rosacea is a good overview. The prescription medications are listed in red and show the pathways that they impact. Click on it for a larger view.
In addition to medications, laser therapy is also an option for rosacea. It may work especially well for rhinophyma (thick skin, red nose).[ref] Photobiomodulation may also be an option.
There are also natural options for rosacea that are often overlooked! Let’s take a look at the other options and the research that supports them.
Lifestyle and Diet:
Clean, antioxidant-rich diet:
A new study (March 2024) showed that a diet high in antioxidant-rich foods reduced the risk of rosacea by 40-45%, which is a pretty big impact. Participants in the study recorded their diets, and it was found that those who ate more antioxidant-rich foods were much less likely to have rosacea at all, and those who did have rosacea had fewer symptoms.[ref]
Avoiding spicy foods:
The TRPV channels are activated by spicy foods that contain capsaicin or cinnamaldehyde. Spicy foods can cause anyone to flush, and the flushing tends to be worse in people with rosacea. Dermatologists often recommend avoiding spicy foods to reduce flushing.[ref]
Alcohol consumption:
Drinking alcohol at any level is associated with an increased risk of rosacea.[ref] Alcohol at higher levels or in people with ALDH gene variants can cause flushing. Alcohol also affects your ability to metabolize histamine. Check your alcohol metabolism genes here.
Face masks:
Wearing face masks increases moisture and bacteria, leading to skin irritation. A number of studies show that wearing masks increases and worsens rosacea symptoms. In addition, the polypropylene material, fabric dyes, formaldehyde, and plasticizers in masks cause skin irritation.[ref]
Supplements and topical options for rosacea:
These are not in any particular order. I suggest looking at your genetic variants related to rosacea to see which pathways to target and then reading the references. Talk to your dermatologist if you have any questions.
Related Articles and Topics:
MRGPRX2: Mast Cells, Itching, & Drug Hypersensitivity Reactions, Including Fluoroquinolones