Key takeaways:
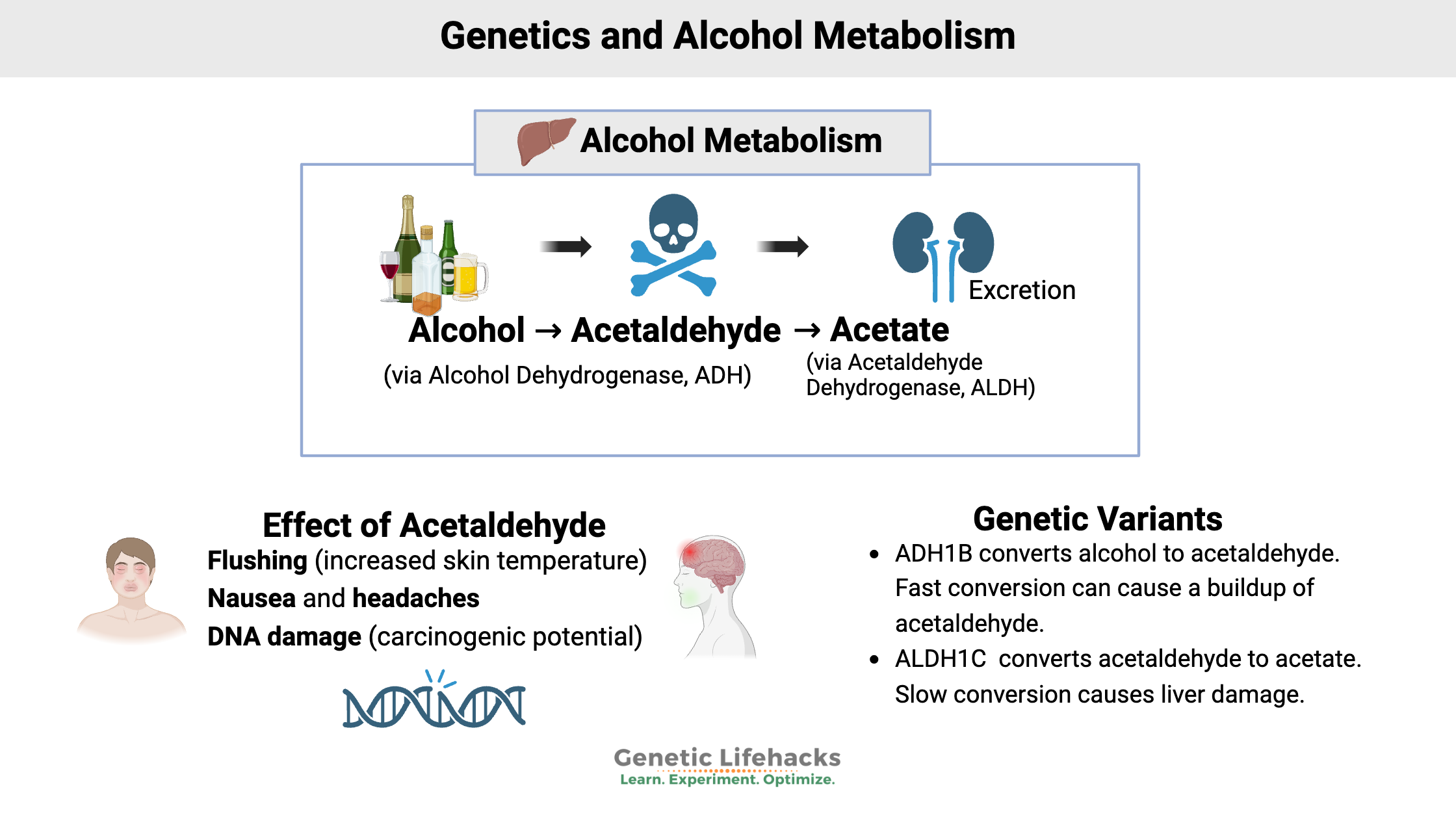
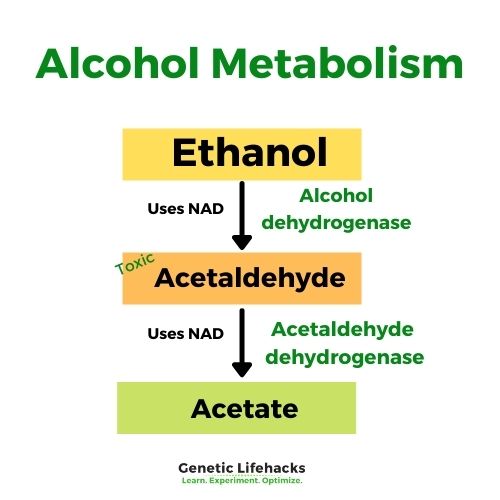
~ Alcohol metabolism is a two-step process: Alcohol is converted to acetaldehyde (toxic), which is then converted to acetate.
~ Genetic variants in the ADH1B and ALDH2 genes affect the speed of alcohol metabolism.
~ ADH1B variants can cause a faster buildup of acetaldehyde.
~ ALDH2 variants can slow acetaldehyde clearance, leading to flushing, nausea, and headaches.
Alcohol: Breaking it down and getting rid of it
People have been imbibing beer and wine for millennia, enjoying alcohol ever since someone discovered the altered sensations from fermented fruits and grains. In fact, archaeologists have discovered an Egyptian brewery dating to the time of the Great Pyramids.
What exactly does alcohol do in our bodies? And why do people react differently to alcohol? (yep – it’s genetic!)
First, alcohol is absorbed through the stomach into our bloodstream, making its way to our brain and liver.
In the liver, alcohol is first broken down with an enzyme called alcohol dehydrogenase, which helps to convert it into acetaldehyde.
In the second step of this elimination process, the enzyme acetaldehyde dehydrogenase helps convert the acetaldehyde into acetate. The acetate can then be easily excreted.
This is a simplified explanation, but it covers the majority of alcohol metabolism.[ref]
Genetics of alcohol metabolism:
The ADH genes, such as ADH1B, code for alcohol dehydrogenase.
The ALDH gene family, such as ALDH2, produces acetaldehyde dehydrogenase.
Two well-studied genetic variants have different ways of reaching the same endpoint:
~ an alcohol dehydrogenase (ADH1B) variant that speeds up the conversion to acetaldehyde, thus creating a buildup of acetaldehyde
~ an acetaldehyde dehydrogenase (ALDH2) variant that slows down the conversion from acetaldehyde to acetic acid, again creating a buildup of acetaldehyde.
More than just alcohol that we drink:
In addition to the beer, wine, and other alcohol we might drink, the alcohol dehydrogenase enzyme also breaks down alcohols produced by bacterial fermentation in the intestines. For example, some of your bug guts could be fermenting the apple you ate this morning, with the ADH genes activated.
Retinol (vitamin A) and bile acids are also metabolized by alcohol dehydrogenase.[ref]
Acetaldehyde: flushing, nausea, and carcinogenic (potentially cancer-causing)
Acetylaldehyde is created in the initial step of metabolizing alcohol. What does acetaldehyde do in the body?
- Acetaldehyde increases skin temperature, making you feel hot and flushed.
- It also causes nausea, headache, and allergy-like histamine release.
To top it off, it is carcinogenic and damaging to your DNA. Moreover, it may also be causing catecholamine release in your brain, giving you feelings of euphoria. Your body wants to get rid of it as soon as possible since it is toxic, but the euphoria makes you want to drink again.[ref]
People who don’t break down the acetaldehyde quickly enough are likely to flush and feel bad when drinking.
Alcohol Metabolism Genotype Report
Lifehacks for Drinking Alcohol:
Making alcohol less toxic?
The simple answer is that alcohol is toxic to everyone. Drinking a lot is bad for your body. I know that many people will ignore the ‘don’t drink’ advice, so below are ways to help your body clear acetaldehyde.
MitoQ, a mitochondrial supplement, has been shown in studies to enhance acetaldehyde clearance in the liver. “This study demonstrated that speeding up acetaldehyde clearance by preserving ALDH2 activity critically mediates the beneficial effect of MitoQ on alcohol-induced pathogenesis at the gut-liver axis.”[ref]
Zinc and niacin (vitamin B3) are both cofactors for acetaldehyde dehydrogenase.[ref] Make sure you have sufficient levels of both through foods or supplements.
Glutathione is also needed for the conversion of acetaldehyde into acetic acid. NAC is a precursor to glutathione.
H2 blockers such as cimetidine can help reduce the flushing symptoms of the ALDH2 variant. Note that this is just helping the flushing and not moving out the acetaldehyde faster.[ref]
Supplement Stacks for Alcohol Metabolism SNPs
Related Articles and Topics:
Key Genes to check for Alcoholism
Are there key genes to check for alcoholism? Learn more about the genetic connections to alcohol addiction and what research-backed treatment options are available.
Dopamine Receptors
Dopamine is a powerful player in our cognitive function – impacting mood, movement, and motivation. Genetic variants in the dopamine receptors influence addiction, ADHD, neurological diseases, depression, psychosis, and aggression.
Bipolar Disorder, Depression, Circadian Clock Genes
New research shows that depression and bipolar disorder are linked to changes or disruptions in circadian genes. Some people carry genetic variants in the circadian genes that make them more susceptible to circadian disruption.
Lithium Orotate + B12: Boosting mood and decreasing anxiety, for some people…
For some people, low-dose, supplemental lithium orotate is a game-changer for mood issues when combined with vitamin B12. But other people may have little to no response. The difference may be in your genes.
References:
“Ancient Egyptian Beer-Making Facilities Found by Archaeologists.” The Independent, 8 Feb. 2018, https://www.independent.co.uk/news/science/archaeology/egypt-beer-making-ancient-brewery-archaeologists-a8201471.html.
“Antihistamines Prevent ‘Asian Flush’ — Alcohol-Induced Facial Redness — but Pose Risks.” USC News, 8 Dec. 2016, https://news.usc.edu/112489/antihistamines-prevent-asian-flush-the-red-face-some-people-get-from-alcohol-but-with-huge-risks/.
Butterworth, R. F. “Pathophysiology of Alcoholic Brain Damage: Synergistic Effects of Ethanol, Thiamine Deficiency and Alcoholic Liver Disease.” Metabolic Brain Disease, vol. 10, no. 1, Mar. 1995, pp. 1–8. PubMed, https://doi.org/10.1007/BF01991777.
Edenberg, Howard J. “The Genetics of Alcohol Metabolism: Role of Alcohol Dehydrogenase and Aldehyde Dehydrogenase Variants.” Alcohol Research & Health, vol. 30, no. 1, 2007, pp. 5–13.
—. “The Genetics of Alcohol Metabolism: Role of Alcohol Dehydrogenase and Aldehyde Dehydrogenase Variants.” Alcohol Research & Health, vol. 30, no. 1, 2007, pp. 5–13.
—. “The Genetics of Alcohol Metabolism: Role of Alcohol Dehydrogenase and Aldehyde Dehydrogenase Variants.” Alcohol Research & Health, vol. 30, no. 1, 2007, pp. 5–13.
—. “The Genetics of Alcohol Metabolism: Role of Alcohol Dehydrogenase and Aldehyde Dehydrogenase Variants.” Alcohol Research & Health, vol. 30, no. 1, 2007, pp. 5–13.
Ehlers, Cindy L. “Variations in ADH and ALDH in Southwest California Indians.” Alcohol Research & Health, vol. 30, no. 1, 2007, pp. 14–17.
Eriksson, C. J. “The Role of Acetaldehyde in the Actions of Alcohol (Update 2000).” Alcoholism, Clinical and Experimental Research, vol. 25, no. 5 Suppl ISBRA, May 2001, pp. 15S-32S. PubMed, https://doi.org/10.1097/00000374-200105051-00005.
Fang, F., et al. “Association between Alcohol Dehydrogenase 1C Gene *1/*2 Polymorphism and Pancreatitis Risk: A Meta-Analysis.” Genetics and Molecular Research: GMR, vol. 14, no. 4, Nov. 2015, pp. 15267–75. PubMed, https://doi.org/10.4238/2015.November.30.2.
Gainza-Cirauqui, M. L., et al. “Production of Carcinogenic Acetaldehyde by Candida Albicans from Patients with Potentially Malignant Oral Mucosal Disorders.” Journal of Oral Pathology & Medicine: Official Publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology, vol. 42, no. 3, Mar. 2013, pp. 243–49. PubMed, https://doi.org/10.1111/j.1600-0714.2012.01203.x.
Hao, Liuyi, et al. “Mitochondria-Targeted Ubiquinone (MitoQ) Enhances Acetaldehyde Clearance by Reversing Alcohol-Induced Posttranslational Modification of Aldehyde Dehydrogenase 2: A Molecular Mechanism of Protection against Alcoholic Liver Disease.” Redox Biology, vol. 14, Apr. 2018, pp. 626–36. PubMed, https://doi.org/10.1016/j.redox.2017.11.005.
Jiménez-Jiménez, Félix Javier, et al. “Association Between the Rs1229984 Polymorphism in the Alcohol Dehydrogenase 1B Gene and Risk for Restless Legs Syndrome.” Sleep, vol. 40, no. 12, Dec. 2017. PubMed, https://doi.org/10.1093/sleep/zsx174.
Lai, Ching-Long, et al. “Inhibition of Human Alcohol and Aldehyde Dehydrogenases by Cimetidine and Assessment of Its Effects on Ethanol Metabolism.” Chemico-Biological Interactions, vol. 202, no. 1–3, Feb. 2013, pp. 275–82. PubMed, https://doi.org/10.1016/j.cbi.2012.11.016.
Langhi, Cédric, et al. “Regulation of Human Class I Alcohol Dehydrogenases by Bile Acids.” Journal of Lipid Research, vol. 54, no. 9, Sept. 2013, pp. 2475–84. PubMed, https://doi.org/10.1194/jlr.M039404.
Li, Dawei, et al. “Further Clarification of The Contribution of The ADH1C Gene to The Vulnerability of Alcoholism And Selected Liver Diseases.” Human Genetics, vol. 131, no. 8, Aug. 2012, pp. 1361–74. PubMed Central, https://doi.org/10.1007/s00439-012-1163-5.
—. “Strong Association of the Alcohol Dehydrogenase 1B Gene (ADH1B) with Alcohol Dependence and Alcohol-Induced Medical Diseases.” Biological Psychiatry, vol. 70, no. 6, Sept. 2011, pp. 504–12. PubMed, https://doi.org/10.1016/j.biopsych.2011.02.024.
Park, Ji Young, et al. “Impact of Smoking on Lung Cancer Risk Is Stronger in Those with the Homozygous Aldehyde Dehydrogenase 2 Null Allele in a Japanese Population.” Carcinogenesis, vol. 31, no. 4, Apr. 2010, pp. 660–65. PubMed, https://doi.org/10.1093/carcin/bgq021.
“PDB101: Molecule of the Month: Alcohol Dehydrogenase.” RCSB: PDB-101, http://pdb101.rcsb.org/motm/13. Accessed 26 Oct. 2021.
Pham, Toan, et al. “MitoQ and CoQ10 Supplementation Mildly Suppresses Skeletal Muscle Mitochondrial Hydrogen Peroxide Levels without Impacting Mitochondrial Function in Middle-Aged Men.” European Journal of Applied Physiology, vol. 120, no. 7, July 2020, pp. 1657–69. PubMed, https://doi.org/10.1007/s00421-020-04396-4.
Sakiyama, Masayuki, et al. “Independent Effects of ADH1B and ALDH2 Common Dysfunctional Variants on Gout Risk.” Scientific Reports, vol. 7, no. 1, May 2017, p. 2500. PubMed, https://doi.org/10.1038/s41598-017-02528-z.
Yokoyama, Akira, et al. “Slow-Metabolizing ADH1B and Inactive Heterozygous ALDH2 Increase Vulnerability to Fatty Liver in Japanese Men with Alcohol Dependence.” Journal of Gastroenterology, vol. 53, no. 5, May 2018, pp. 660–69. PubMed, https://doi.org/10.1007/s00535-017-1402-6.
Zellner, Tobias, et al. “The Use of Activated Charcoal to Treat Intoxications.” Deutsches Arzteblatt International, vol. 116, no. 18, May 2019, pp. 311–17. PubMed, https://doi.org/10.3238/arztebl.2019.0311.
Originally published June, 2018. Revised Feb. 2020