Key takeaways:
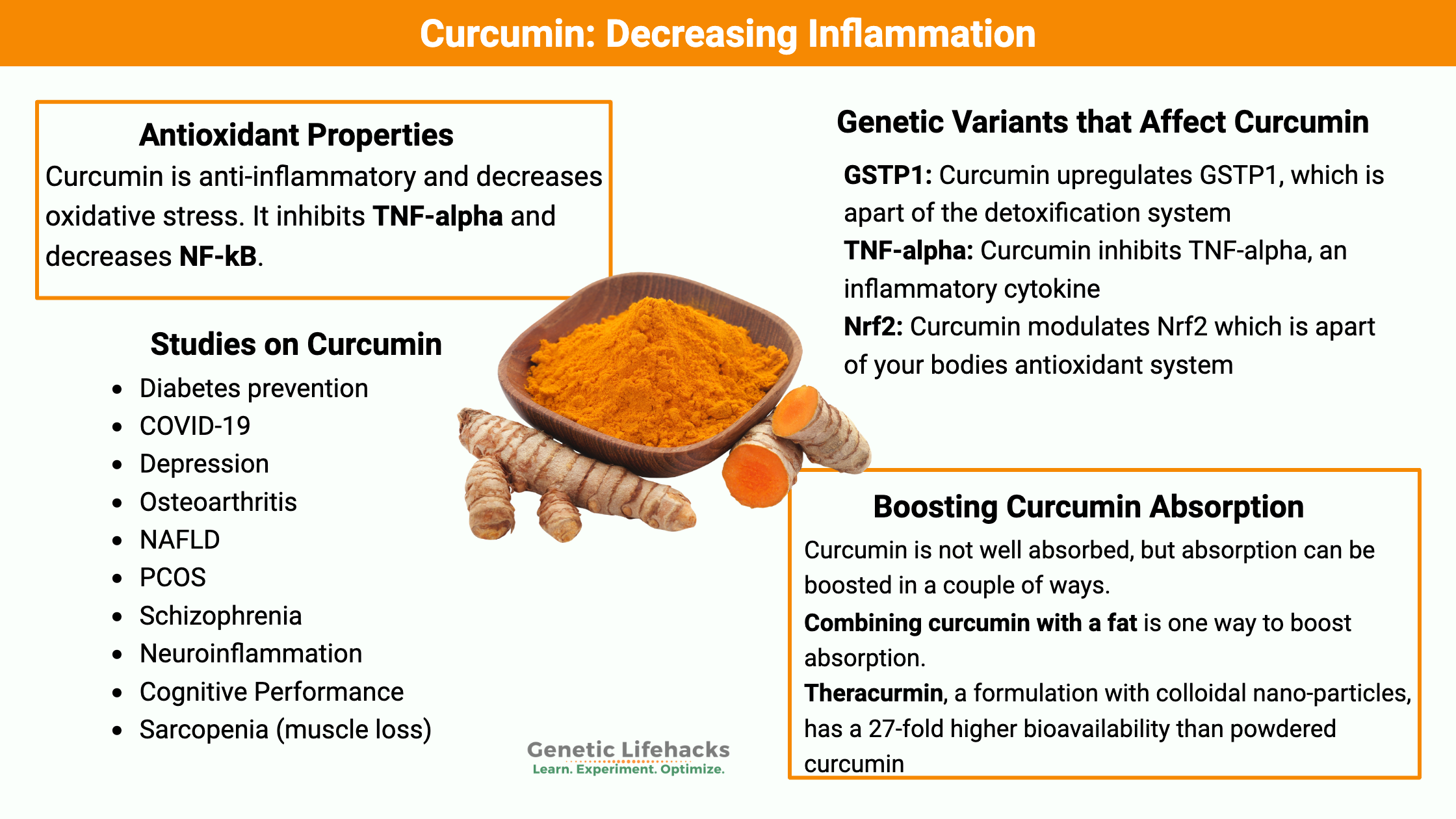
~ Curcumin is anti-inflammatory and decreases oxidative stress.
~ It inhibits TNF-alpha and decreases NF-kB.
~ Curcumin has been studied in a lot of human clinical trials with numerous beneficial outcomes.
~ It is not well absorbed, but absorption can be boosted in a couple of ways.
Members will see their genotype report below, plus additional solutions in the Lifehacks section. Consider joining today.
Talk with your doctor if you have any questions about supplements, especially if you are on prescription medications.
Benefits of curcumin:
Curcumin, a polyphenol found in turmeric, is a spice used in traditional Indian cuisine and in other areas of Asia as a drink. Turmeric is harvested from the rhizome of Curcuma longa, which is a member of the ginger family. It has a long history of use both as a spice and in traditional Ayurvedic medicine.
As a supplement, curcumin is well-studied, with randomized, placebo-controlled trials as well as tons of animal and cell studies.
The main effect of curcumin is a decrease in inflammation through a reduction in inflammatory cytokines. This decrease in inflammation impacts a variety of different chronic conditions such as arthritis, diabetes, NAFLD, and cognitive function.
Safety of Curcumin:
A new study looked into the reported liver injuries from 2004 to 2022 in the US. The researchers found that 10 of the liver injury cases over the last decade were attributed to turmeric combined with black pepper. Genetically, the researchers found that half of those 10 with liver injuries also carried a specific HLA type, HLA-B*35:01 (not found in 23andMe or AncestryDNA data). [ref]
While clinical trial data shows that curcumin is relatively safe, always keep in mind that any supplement could cause problems for some people.
Clinical trials using curcumin:
Hundreds of randomized, placebo-controlled clinical trials have investigated the efficacy of curcumin for a variety of different conditions. Here are just a few of the trials:
Diabetes prevention:
A clinical trial that included 240 participants assessed the efficacy of curcumin for preventing diabetes. The participants all had prediabetes, and half of the group took a curcumin supplement (500 mg/3 times a day). After 9 months, almost 1/5 of the control group had progressed to diabetes, but none of the curcumin group had progressed. In fact, the curcumin-treated group had a decrease in HOMA-IR.[ref]
Related article: Read about diabetes and blood glucose genes
COVID-19:
A clinical trial with 80 participants tested nano-curcumin for the effect on cytokine production in COVID-19 patients. Nano-curcumin decreased IL-6 and IL-1B secretion, which may be important in severe cases of COVID-19.[ref]
Depression:
A randomized clinical trial showed curcumin (500 mg/2x per day) to be more effective than placebo for improving depression. The benefits were shown at 4 to 8 weeks after starting the supplement.[ref]
Related article: Depression and Inflammation (check to see if your genes make you more susceptible to depression or anxiety due to inflammatory cytokines)
Osteoarthritis:
A curcumin-phosphatidylcholine complex (Meriva) was effective in decreasing inflammatory markers and in decreasing joint pain.[ref] Another clinical trial found that curcumin (500mg / 3x per day) was as effective as diclofenac for osteoarthritis – but with fewer side effects.[ref]
NAFLD:
A clinical trial with 50 fatty liver disease patients found that 1500mg/day of curcumin significantly decreased liver fibrosis and inflammatory markers.[ref]
Related article: Fatty Liver Disease Genetic Risk Factor
PCOS:
This clinical trial included women with PCOS who were taking metformin. The addition of curcumin additionally decreased blood glucose levels as well as LDL cholesterol.[ref]
Related article: PCOS genes
Gulf War Illness:
A clinical trial looked at the effect of curcumin and several other natural supplements on the symptoms of Gulf War Illness. Only curcumin significantly reduced symptoms of GWI.[ref]
Related article: Genetic risk factors for Gulf War Illness
Schizophrenia:
As an adjunct to regular antipsychotic medication, the addition of nanocurcumin significantly improved psychiatric symptom scores.[ref]
Sarcopenia (muscle loss):
Muscle mass decline is a serious problem in the elderly. Curcumin supplementation increased handgrip strength and weight lifting strength compared to placebo.[ref]
Cognitive Performance:
Curcumin supplementation improved cognitive performance in middle-aged, overweight people.[ref]
Neuroinflammation:
A trial of curcumin plus fish oil showed a significant reduction in IL-1β levels.[ref]
Muscle pain after exercise:
In a clinical trial, curcumin supplementation reduced delayed-onset muscle pain after exercise.[ref]
Curcumin decreases chronic inflammation:
While the many human clinical trials show that curcumin is effective at reducing symptoms in chronic inflammatory conditions, cell and animal studies elucidate the mechanism of action:
IL-17 reduction:
Curcumin reduces IL-17 production through the induction of IDO (tryptophan enzyme in the kynurenine pathway).[ref]
Inflammatory cytokines:
A randomized clinical trial of curcumin (1g/day) in people with metabolic syndrome showed statistically significant reductions in TNF-α, IL-6, TGF-β, and MCP-1.[ref]
What are the side effects of curcumin?
Phase I clinical trials show that curcumin is safe at high doses of 12 g/day.[ref]
Anecdotally, curcumin at higher doses may give some people intestinal issues. Thus, keep an eye out for gastrointestinal side effects and cut back if needed.
Research shows that curcumin can stimulate the gall bladder.[ref] For someone with gallstones, this could cause issues.
Some research studies show that curcumin increases the excretion of oxalates in the urine.[ref] People who are prone to kidney stones may want to talk to their doctor about curcumin.
Curcumin Genotype Report:
Not a member? Join here. Membership lets you see your data right in each article and also gives you access to the member’s only information in the Lifehacks sections.
GSTP1: Curcumin induces the expression of GSTP1 (glutathione S-transferase P1).[ref] GSTP1 is part of the body’s detoxification system, responsible for getting rid of certain toxicants through conjugation with glutathione. GSTP1 is important in cancer prevention through its elimination of carcinogens.[ref] For women, GSTP1 is important in the way estrogen is metabolized, and promoting better GSTP1 function may help to decrease the risk of breast cancer.[ref]
Related article: Estrogen metabolism
Some people have GSTP1 variants that cause the enzyme not to function as well as normal, and curcumin may help to increase expression.
Check your genetic data for rs1695 (23andMe v4, v5; AncestryDNA):
- A/A: typical; possibly higher IL-6 in men who take vitamin E[ref]
- A/G: typical risk of breast cancer
- G/G: reduced function, increased risk of breast cancer[ref][ref] increased risk of prostate cancer[ref] increased risk of nasal polyps[ref]
Members: Your genotype for rs1695 is —.
TNF-alpha: Curcumin decreases TNF-alpha levels. TNF-alpha is an inflammatory cytokine, important in the cellular defense against pathogens. Too much TNF-alpha can cause chronic inflammation and the downstream effects resulting in chronic disease.
Some people have genetic variants that increase their cellular production of TNF-alpha.
Check your genetic data for rs1800629 -308A/G (23andMe v4, v5; AncestryDNA):
- A/A: Higher TNF-alpha levels. Increased risk of: ulcerative colitis[ref] celiac disease[ref] (note – must have HLA type also), septic shock[ref], diabetic foot ulcers[ref], asthma[ref] , Hashimoto’s thyroiditis[ref], skin infections[ref], periodontitis[ref], asthma[ref] in children, COPD[ref], stroke[ref], gum disease[ref], heart disease[ref]; nasal polyps[ref] Lower risk of: Malaria (half the risk)[ref], osteoporosis[ref], stroke[ref]
- A/G: somewhat higher TNF-alpha levels – see above
- G/G: typical, better response to high protein/low carb diet
Members: Your genotype for rs1800629 is —.
p53 (tumor suppressor): The TP53 gene encodes a tumor suppressor, called p53, which is important in preventing cancer. Studies have shown that curcumin increases p53 in colon cancer patients.[ref][ref] It is being studied as an adjuvant to chemotherapy.[ref]
Nrf2 and Keap1: Studies show that curcumin decreases inflammation through modulating Nrf2. The Nrf2 pathway regulates the expression of antioxidants created in the cells and counteracts cellular oxidative stress. Keap1 is a protein that has been identified as a repressor of Nrf2 activation. Recent research shows that curcumin inhibits Keap1 expression, thus repressing the repressor of Nrf2.[ref]
Nrf2 levels are partly impacted by genetics:
Check your genetic data for rs6721961 (23andMe v4):
- G/G: typical
- G/T: typical
- T/T: significantly diminished Nrf2 expression, increased risk of lung cancer[ref]
Members: Your genotype for rs6721961 is —.
Epigenetics and curcumin:
Epigenetics is the changing of gene expression. These aren’t inherited changes to your DNA, but rather the increases or decreases in gene expression.
One way that genes turn ‘off or on’ is through histone modification. Histones control how your DNA is packaged up so that a gene can’t be translated into a protein. Modifying histones, therefore, allows a gene to ‘express’ or turn into its encoded protein.
Curcumin has been shown in studies to be a potent inhibitor of histone deacetylases. This means that curcumin inhibits the enzymes that control how histones package up DNA and prevent it from being read. In fact, curcumin seems to be more effective at inhibiting histone deacetylases than drugs, such as valproic acid or sodium butyrate, which are well known for this function. The key, though, is that this occurs at levels similar to pharmacological drugs only when curcumin concentrations are fairly high.[ref] (Higher than through regular supplement levels, if I’m understanding the research right).
Let me give you an example…
One way that curcumin may help as an adjunct in cancer treatments is through acting as a histone modifier to increase p53. The tumor suppressor p53 often ‘turns off’ in cancer cells, and studies show that curcumin is one molecule that may be able to turn it back on.[ref]
Absorption and metabolism of curcumin:
The rest of this article is for Genetic Lifehacks members only. Consider joining today to see the rest of this article.
Conclusion:
Curcumin is a well-studied natural supplement that has been tested in a myriad of clinical trials. It offers anti-inflammatory properties that may help with chronic diseases. There are many options for curcumin supplements, and you may find that experimenting with several types is the best way to find out what works for you.
References:
Amalraj, Augustine, et al. “The Effects of Bioavailable Curcumin (Cureit) on Delayed Onset Muscle Soreness Induced By Eccentric Continuous Exercise: A Randomized, Placebo-Controlled, Double-Blind Clinical Study.” Journal of Medicinal Food, vol. 23, no. 5, May 2020, pp. 545–53. PubMed, https://doi.org/10.1089/jmf.2019.4533.
Anand, Preetha, et al. “Bioavailability of Curcumin: Problems and Promises.” Molecular Pharmaceutics, vol. 4, no. 6, Dec. 2007, pp. 807–18. PubMed, https://doi.org/10.1021/mp700113r.
Belcaro, Gianni, et al. “Efficacy and Safety of Meriva®, a Curcumin-Phosphatidylcholine Complex, during Extended Administration in Osteoarthritis Patients.” Alternative Medicine Review: A Journal of Clinical Therapeutic, vol. 15, no. 4, Dec. 2010, pp. 337–44.
Chuengsamarn, Somlak, et al. “Curcumin Extract for Prevention of Type 2 Diabetes.” Diabetes Care, vol. 35, no. 11, Nov. 2012, pp. 2121–27. PubMed Central, https://doi.org/10.2337/dc12-0116.
Cuomo, John, et al. “Comparative Absorption of a Standardized Curcuminoid Mixture and Its Lecithin Formulation.” Journal of Natural Products, vol. 74, no. 4, Apr. 2011, pp. 664–69. PubMed, https://doi.org/10.1021/np1007262.
Dhamodharan, Umapathy, et al. “Genetic Association of IL-6, TNF-α and SDF-1 Polymorphisms with Serum Cytokine Levels in Diabetic Foot Ulcer.” Gene, vol. 565, no. 1, July 2015, pp. 62–67. PubMed, https://doi.org/10.1016/j.gene.2015.03.063.
Ding, Cheng, et al. “TNF-α Gene Promoter Polymorphisms Contribute to Periodontitis Susceptibility: Evidence from 46 Studies.” Journal of Clinical Periodontology, vol. 41, no. 8, Aug. 2014, pp. 748–59. PubMed, https://doi.org/10.1111/jcpe.12279.
Donovan, Emily K., et al. “A Placebo-Controlled, Pseudo-Randomized, Crossover Trial of Botanical Agents for Gulf War Illness: Curcumin (Curcuma Longa), Boswellia (Boswellia Serrata), and French Maritime Pine Bark (Pinus Pinaster).” International Journal of Environmental Research and Public Health, vol. 18, no. 5, Mar. 2021, p. 2468. PubMed, https://doi.org/10.3390/ijerph18052468.
Dragovic, Sanja, et al. “Effect of Human Glutathione S-Transferase HGSTP1-1 Polymorphism on the Detoxification of Reactive Metabolites of Clozapine, Diclofenac and Acetaminophen.” Toxicology Letters, vol. 224, no. 2, Jan. 2014, pp. 272–81. PubMed, https://doi.org/10.1016/j.toxlet.2013.10.023.
Durães, Cecília, et al. “Polymorphisms in the TNFA and IL6 Genes Represent Risk Factors for Autoimmune Thyroid Disease.” PloS One, vol. 9, no. 8, 2014, p. e105492. PubMed, https://doi.org/10.1371/journal.pone.0105492.
Edwards, Rebecca L., et al. “The Anti-Inflammatory Activity of Curcumin Is Mediated by Its Oxidative Metabolites.” The Journal of Biological Chemistry, vol. 292, no. 52, Dec. 2017, pp. 21243–52. PubMed, https://doi.org/10.1074/jbc.RA117.000123.
—. “The Anti-Inflammatory Activity of Curcumin Is Mediated by Its Oxidative Metabolites.” The Journal of Biological Chemistry, vol. 292, no. 52, Dec. 2017, pp. 21243–52. PubMed Central, https://doi.org/10.1074/jbc.RA117.000123.
England, Anna, et al. “Variants in the Genes Encoding TNF-α, IL-10, and GSTP1 Influence the Effect of α-Tocopherol on Inflammatory Cell Responses in Healthy Men.” The American Journal of Clinical Nutrition, vol. 95, no. 6, June 2012, pp. 1461–67. Silverchair, https://doi.org/10.3945/ajcn.111.012781.
Feng, Bo, et al. “Association of Tumor Necrosis Factor α -308G/A and Interleukin-6 -174G/C Gene Polymorphism with Pneumonia-Induced Sepsis.” Journal of Critical Care, vol. 30, no. 5, Oct. 2015, pp. 920–23. PubMed, https://doi.org/10.1016/j.jcrc.2015.04.123.
Gichohi-Wainaina, Wanjiku N., et al. “Tumour Necrosis Factor Allele Variants and Their Association with the Occurrence and Severity of Malaria in African Children: A Longitudinal Study.” Malaria Journal, vol. 14, June 2015, p. 249. PubMed, https://doi.org/10.1186/s12936-015-0767-3.
Hassan, Faiz-ul, et al. “Curcumin as an Alternative Epigenetic Modulator: Mechanism of Action and Potential Effects.” Frontiers in Genetics, vol. 10, June 2019, p. 514. PubMed Central, https://doi.org/10.3389/fgene.2019.00514.
He, Zhen-Yu, et al. “Upregulation of P53 Expression in Patients with Colorectal Cancer by Administration of Curcumin.” Cancer Investigation, vol. 29, no. 3, Feb. 2011, pp. 208–13. Taylor and Francis+NEJM, https://doi.org/10.3109/07357907.2010.550592.
Honarvar, Niyaz M., et al. “Anti-Neuroinflammatory Properties of n-3 Fatty Acids and Nano- Curcumin on Migraine Patients from Cellular to Clinical Insight: A Randomized, Double-Blind and Placebo-Controlled Trial.” Endocrine, Metabolic & Immune Disorders Drug Targets, vol. 21, no. 2, 2021, pp. 365–73. PubMed, https://doi.org/10.2174/1871530320666200729144430.
Hosseininasab, Masumeh, et al. “Nanocurcumin as an Add-on to Antipsychotic Drugs for Treatment of Negative Symptoms in Patients With Chronic Schizophrenia: A Randomized, Double-Blind, Placebo-Controlled Study.” Journal of Clinical Psychopharmacology, vol. 41, no. 1, Feb. 2021, pp. 25–30. PubMed, https://doi.org/10.1097/JCP.0000000000001324.
Jäger, Ralf, et al. “Comparative Absorption of Curcumin Formulations.” Nutrition Journal, vol. 13, Jan. 2014, p. 11. PubMed Central, https://doi.org/10.1186/1475-2891-13-11.
Khan, Saif, et al. “TNF-α -308 G > A (Rs1800629) Polymorphism Is Associated with Celiac Disease: A Meta-Analysis of 11 Case-Control Studies.” Scientific Reports, vol. 6, Sept. 2016, p. 32677. PubMed, https://doi.org/10.1038/srep32677.
Kotrych, Daniel, et al. “TNF-α and IL10 Gene Polymorphisms in Women with Postmenopausal Osteoporosis.” European Journal of Obstetrics, Gynecology, and Reproductive Biology, vol. 199, Apr. 2016, pp. 92–95. PubMed, https://doi.org/10.1016/j.ejogrb.2016.01.037.
Larussa, Tiziana, et al. “Downregulation of Interleukin- (IL-) 17 through Enhanced Indoleamine 2,3-Dioxygenase (IDO) Induction by Curcumin: A Potential Mechanism of Tolerance towards Helicobacter Pylori.” Journal of Immunology Research, vol. 2018, Oct. 2018, p. 3739593. PubMed Central, https://doi.org/10.1155/2018/3739593.
Lopresti, Adrian L., et al. “Curcumin for the Treatment of Major Depression: A Randomised, Double-Blind, Placebo Controlled Study.” Journal of Affective Disorders, vol. 167, 2014, pp. 368–75. PubMed, https://doi.org/10.1016/j.jad.2014.06.001.
MacIntyre, Elaina A., et al. “GSTP1 and TNF Gene Variants and Associations between Air Pollution and Incident Childhood Asthma: The Traffic, Asthma and Genetics (TAG) Study.” Environmental Health Perspectives, vol. 122, no. 4, Apr. 2014, pp. 418–24. PubMed, https://doi.org/10.1289/ehp.1307459.
Majumder, Poulami, et al. “Association of Tumor Necrosis Factor-α (TNF-α) Gene Promoter Polymorphisms with Aggressive and Chronic Periodontitis in the Eastern Indian Population.” Bioscience Reports, vol. 38, no. 4, Aug. 2018, p. BSR20171212. PubMed, https://doi.org/10.1042/BSR20171212.
Najafi, Masoud, et al. “The Role of Curcumin/Curcuminoids during Gastric Cancer Chemotherapy: A Systematic Review of Non-Clinical Study.” Life Sciences, vol. 257, Sept. 2020, p. 118051. ScienceDirect, https://doi.org/10.1016/j.lfs.2020.118051.
Nishinaka, Toru, et al. “Curcumin Activates Human Glutathione S-Transferase P1 Expression through Antioxidant Response Element.” Toxicology Letters, vol. 170, no. 3, May 2007, pp. 238–47. PubMed, https://doi.org/10.1016/j.toxlet.2007.03.011.
Panahi, Yunes, et al. “Effects of Curcumin on Serum Cytokine Concentrations in Subjects with Metabolic Syndrome: A Post-Hoc Analysis of a Randomized Controlled Trial.” Biomedicine & Pharmacotherapy = Biomedecine & Pharmacotherapie, vol. 82, Aug. 2016, pp. 578–82. PubMed, https://doi.org/10.1016/j.biopha.2016.05.037.
Patiño-Morales, Carlos César, et al. “Curcumin Stabilizes P53 by Interaction with NAD(P)H:Quinone Oxidoreductase 1 in Tumor-Derived Cell Lines.” Redox Biology, vol. 28, Jan. 2020, p. 101320. PubMed, https://doi.org/10.1016/j.redox.2019.101320.
Qiu, Juanjuan, et al. “Association between Polymorphisms in Estrogen Metabolism Genes and Breast Cancer Development in Chinese Women.” Medicine, vol. 97, no. 47, Nov. 2018, p. e13337. PubMed Central, https://doi.org/10.1097/MD.0000000000013337.
Ren, Liwei, et al. “Curcumin Upregulates the Nrf2 System by Repressing Inflammatory Signaling-Mediated Keap1 Expression in Insulin-Resistant Conditions.” Biochemical and Biophysical Research Communications, vol. 514, no. 3, June 2019, pp. 691–98. ScienceDirect, https://doi.org/10.1016/j.bbrc.2019.05.010.
Reséndiz-Hernández, Juan Manuel, et al. “Identification of Genetic Variants in the TNF Promoter Associated with COPD Secondary to Tobacco Smoking and Its Severity.” International Journal of Chronic Obstructive Pulmonary Disease, vol. 10, 2015, pp. 1241–51. PubMed, https://doi.org/10.2147/COPD.S83298.
Saadati, Saeede, et al. “Curcumin and Inflammation in Non-Alcoholic Fatty Liver Disease: A Randomized, Placebo Controlled Clinical Trial.” BMC Gastroenterology, vol. 19, no. 1, July 2019, p. 133. PubMed, https://doi.org/10.1186/s12876-019-1055-4.
Sasaki, Hiroki, et al. “Innovative Preparation of Curcumin for Improved Oral Bioavailability.” Biological & Pharmaceutical Bulletin, vol. 34, no. 5, 2011, pp. 660–65. PubMed, https://doi.org/10.1248/bpb.34.660.
Shep, Dhaneshwar, et al. “Safety and Efficacy of Curcumin versus Diclofenac in Knee Osteoarthritis: A Randomized Open-Label Parallel-Arm Study.” Trials, vol. 20, no. 1, Apr. 2019, p. 214. PubMed, https://doi.org/10.1186/s13063-019-3327-2.
Shoba, G., et al. “Influence of Piperine on the Pharmacokinetics of Curcumin in Animals and Human Volunteers.” Planta Medica, vol. 64, no. 4, May 1998, pp. 353–56. PubMed, https://doi.org/10.1055/s-2006-957450.
Sohrevardi, Seyed Mojtaba, et al. “Therapeutic Effect of Curcumin in Women with Polycystic Ovary Syndrome Receiving Metformin: A Randomized Controlled Trial.” Advances in Experimental Medicine and Biology, vol. 1308, 2021, pp. 109–17. PubMed, https://doi.org/10.1007/978-3-030-64872-5_9.
Stappers, M. H. T., et al. “Polymorphisms in Cytokine Genes IL6, TNF, IL10, IL17A and IFNG Influence Susceptibility to Complicated Skin and Skin Structure Infections.” European Journal of Clinical Microbiology & Infectious Diseases: Official Publication of the European Society of Clinical Microbiology, vol. 33, no. 12, Dec. 2014, pp. 2267–74. PubMed, https://doi.org/10.1007/s10096-014-2201-0.
Suzuki, Takafumi, et al. “Regulatory Nexus of Synthesis and Degradation Deciphers Cellular Nrf2 Expression Levels.” Molecular and Cellular Biology, vol. 33, no. 12, June 2013, pp. 2402–12. PubMed Central, https://doi.org/10.1128/MCB.00065-13.
Tavares, M., et al. “Tumour Necrosis Factor-Alpha (-308G/A) Promoter Polymorphism Is Associated with Ulcerative Colitis in Brazilian Patients.” International Journal of Immunogenetics, vol. 43, no. 6, Dec. 2016, pp. 376–82. PubMed, https://doi.org/10.1111/iji.12289.
Valizadeh, Hamed, et al. “Nano-Curcumin Therapy, a Promising Method in Modulating Inflammatory Cytokines in COVID-19 Patients.” International Immunopharmacology, vol. 89, no. Pt B, Dec. 2020, p. 107088. PubMed, https://doi.org/10.1016/j.intimp.2020.107088.
Varma, Karthik, et al. “The Efficacy of the Novel Bioavailable Curcumin (Cureit) in the Management of Sarcopenia in Healthy Elderly Subjects: A Randomized, Placebo-Controlled, Double-Blind Clinical Study.” Journal of Medicinal Food, vol. 24, no. 1, Jan. 2021, pp. 40–49. PubMed, https://doi.org/10.1089/jmf.2020.4778.
Vidal, Igor, et al. “GSTP1 Positive Prostatic Adenocarcinomas Are More Common in Black than White Men in the United States.” PLOS ONE, vol. 16, no. 6, June 2021, p. e0241934. PLoS Journals, https://doi.org/10.1371/journal.pone.0241934.
Wu, Jun-Cang, et al. “Gene Polymorphisms and Circulating Levels of the TNF-Alpha Are Associated with Ischemic Stroke: A Meta-Analysis Based on 19,873 Individuals.” International Immunopharmacology, vol. 75, Oct. 2019, p. 105827. PubMed, https://doi.org/10.1016/j.intimp.2019.105827.
—. “Gene Polymorphisms and Circulating Levels of the TNF-Alpha Are Associated with Ischemic Stroke: A Meta-Analysis Based on 19,873 Individuals.” International Immunopharmacology, vol. 75, Oct. 2019, p. 105827. PubMed, https://doi.org/10.1016/j.intimp.2019.105827.
Yucesoy, Berran, et al. “Genetic Variants in TNFα, TGFB1, PTGS1 and PTGS2 Genes Are Associated with Diisocyanate-Induced Asthma.” Journal of Immunotoxicology, vol. 13, no. 1, 2016, pp. 119–26. PubMed, https://doi.org/10.3109/1547691X.2015.1017061.
Zhang, Guimin, et al. “The Role of TNF Alpha Polymorphism and Expression in Susceptibility to Nasal Polyposis.” Immunological Investigations, vol. 47, no. 4, May 2018, pp. 360–71. Taylor and Francis+NEJM, https://doi.org/10.1080/08820139.2018.1433204.
Zhang, Peng, et al. “Tumor Necrosis Factor-Alpha Gene Polymorphisms and Susceptibility to Ischemic Heart Disease.” Medicine, vol. 96, no. 14, Apr. 2017, p. e6569. PubMed Central, https://doi.org/10.1097/MD.0000000000006569.
Zhang, Yonglan, et al. “Glutathione S-Transferase Gene Polymorphisms and Risk of Nasal or Colorectal Polyposis.” Bioscience Reports, vol. 39, no. 1, Jan. 2019, p. BSR20181226. PubMed, https://doi.org/10.1042/BSR20181226.