Key takeaways:
~ Common MTHFR gene variants (C677T and A1298C) reduce the body’s ability to convert folate to its active form, impacting the production of methyl groups needed for neurotransmitters.
~ People with MTHFR variants are at a statistically higher risk of depression.
~ Getting enough folate from your diet (leafy greens, legumes, liver) or low-dose supplements may help. Balance is key here.
MTHFR, methyl groups, and mood
We are all genetically unique, and a common genetic variant in the MTHFR gene causes some people to be more susceptible to having low methylfolate levels.
The MTHFR gene codes for a key enzyme in the folate cycle, which leads to the formation of methyl groups for the methylation cycle.
If all that sounds like gibberish, let me give a quick explanation of the methylation cycle (skip ahead if you know this stuff!):
How the methylation cycle works:
Methylation is the adding and removing of a methyl group (CH3) to amino acids, DNA, and other enzymes or proteins.
Most of the molecules in our body are chains of hydrocarbons — carbons plus hydrogens. So adding a methyl group stacks on one more link in a hydrocarbon chain. Sometimes it helps me to visualize it as if the molecule is made of Legos, and the methyl group just adds another Lego component to your creation.
Adding a methyl group – or an extra carbon plus three hydrogens – then changes the original molecule into something different.
Here’s an example:
A methyl group is added to the neurotransmitter serotonin in the conversion to melatonin, an important circadian rhythm hormone.

Methylation can turn on and off genes, maintain and repair your DNA, and alter proteins.
It is important in the nervous system in the production and breakdown of neurotransmitters and in the detoxification of some environmental toxicants.
The key here is that both neurotransmitter synthesis, DNA repair, and turning on or off genes can be important in depression.[ref]
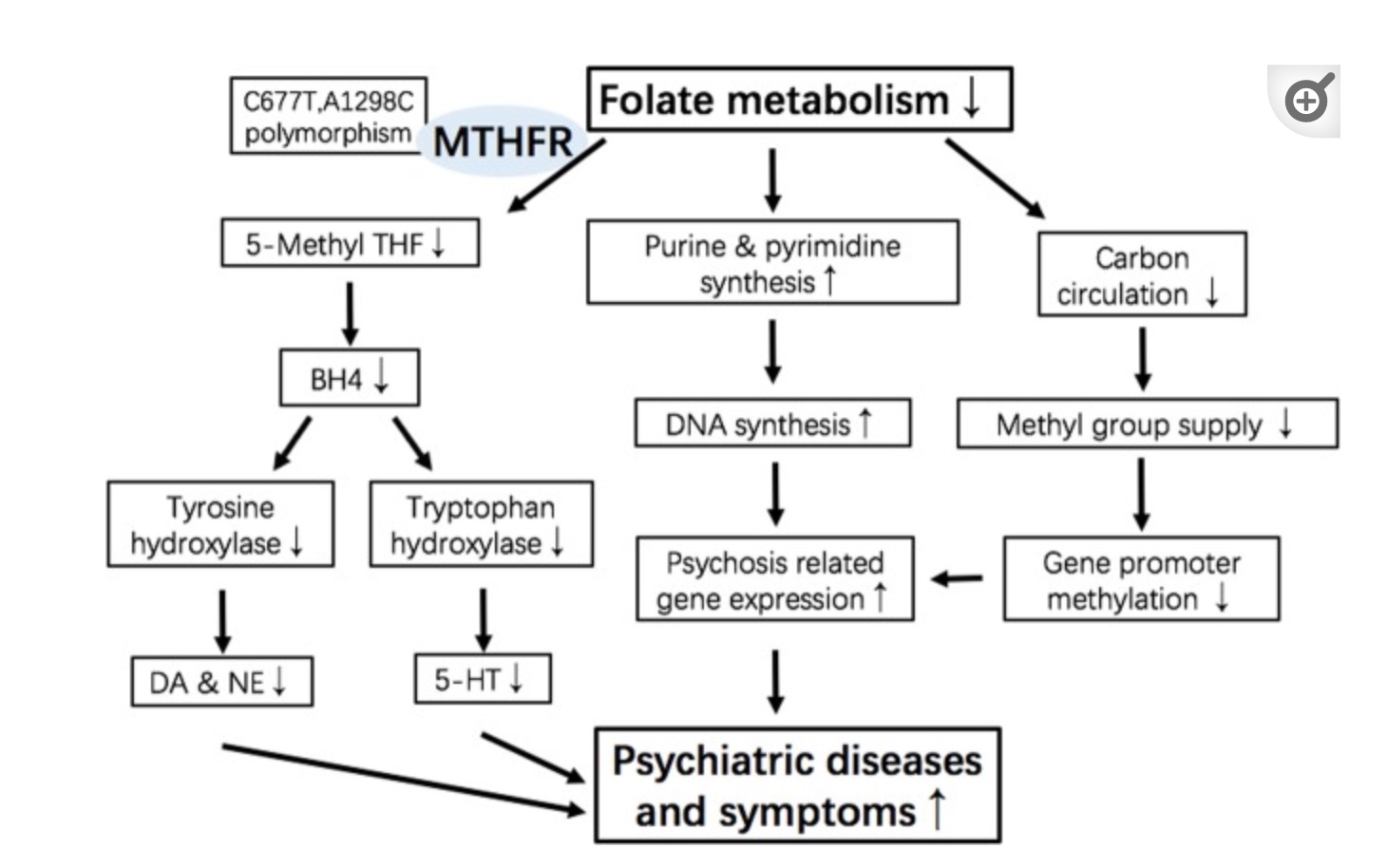
Here’s how one study visually sums up the possible ways MTHFR variants can impact mood:
Depression and Mood Swings with MTHFR
The MTHFR gene codes for methylenetetrahydrofolate reductase, a key enzyme needed to convert folate into methylfolate, which is used in the methylation cycle. When methyl groups are limited, a number of different reactions in the body can be constrained, including the recycling of homocysteine.[ref]
There are two main MTHFR genetic variants, known as C677T and A1298C, which decrease the functioning of the enzyme, which in turn may affect the methylation cycle. (see genotype report below)
MTHFR C677T:
- one copy of the variant decreases the enzyme function by ~40%
- two copies of the variant decrease enzyme function by ~70%
MTHFR A1298C:
- one copy of the variant decreases the enzyme function by 10-20%
- two copies of the variant decrease enzyme function by 30-40%
Let’s take a look at what the research shows about how these MTHFR variants impact the risk of depression:
A meta-analysis that grouped the data from several different studies found that the MTHFR C677T variant increases the risk of depressive disorders.[ref]
Another meta-analysis, which included 26 different published studies, also found that the MTHFR C677T variant was associated with an increased risk of depression. This study noted that the association is stronger in Asian ancestry and more marginal in Caucasians (although still statistically significant).[ref]
Age and gender may also play a role here. Postmenopausal women who carried the MTHFR C677T variant were found to be at a 2 to 3-fold increased risk of depression.[ref]
I do want to point out that not all studies agree, and some researchers find that the MTHFR C677T variant has little to no impact on depression risk. This may be due to the difference that diet plays here. People who eat a diet that includes more folate (green veggies, legumes, etc) may not be at an increased risk, while people who are folate-deficient may be more susceptible to depression.[ref][ref]
What about MTHFR A1298C?
Women who were homozygous (two copies) for the MTHFR A1298C variant were found to be at twice the risk of major depressive disorder, and this risk was even higher in COMT MET allele carriers. (Check your COMT variant here)[ref]
Depression treatment clinical trial: high dose folate and vitamins
A 2016 placebo-controlled clinical trial investigated the effectiveness of treating depression using methylation cycle-specific vitamins. The trial included 330 adults with major depressive disorder and an MTHFR variant. The results of the study show a marked reduction in homocysteine levels in the vitamin-treated group as well as a very impressive reduction in depression scores. The vitamin-treated group was taking high doses of three forms of folate (1mg folic acid, 2.5 mg folinic acid, and 7mg of l-methyl folate), magnesium, zinc, phosphatidylserine, and iron, along with microgram doses of the active forms of thiamine, B6, adenosyl-B12, NADH, and TMG. The vitamin-treated group saw a decrease in depression score from an average score of 27 at baseline to 15 after 8 weeks, while the placebo group only saw a 1.3 point drop.[ref]
MTHFR Genotype Report
Lifehacks for MTHFR and depression:
First and foremost, if you are under the care of a physician or psychiatrist for a mood disorder, please check in with them before making any changes. Seriously. While it can be easy to think that a B-vitamin supplement is innocuous, for some people – especially combined with medications – supplements could alter your mental state.
Research does show that low folate levels correlate with higher depression scores.[ref][ref] The research, though, is on a group of people, averaging things out. You – as a unique individual – may be different than the group average.
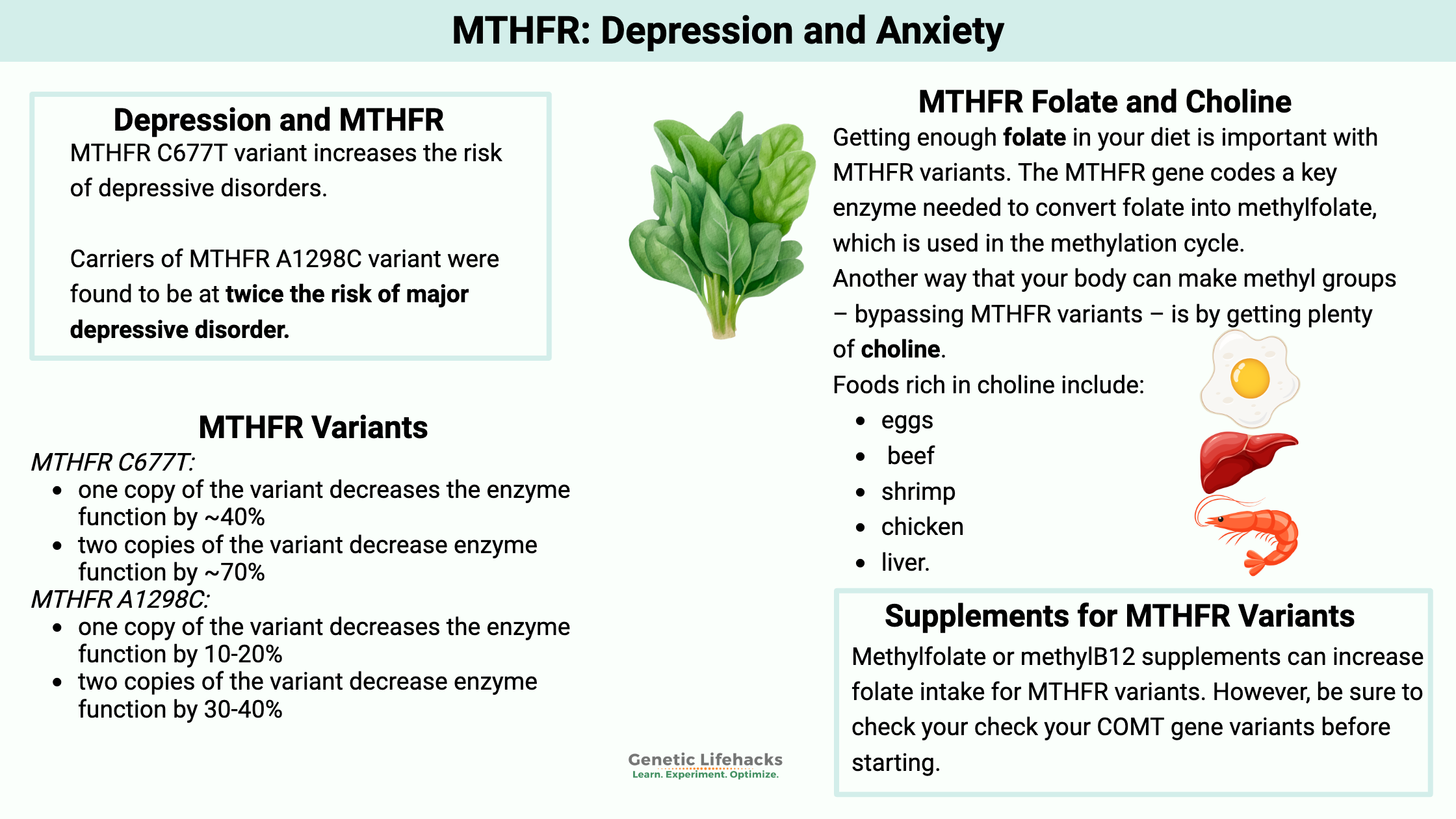
Folate and choline-rich foods:
Getting enough folate in your diet is important with MTHFR variants. You know how your mom said to eat your green veggies – it turns out she was right. Folate-rich foods include leafy greens, legumes, and beef liver.
Another way that your body can make methyl groups – bypassing a wonky MTHFR variant – is by getting plenty of choline. Foods rich in choline include eggs, beef, shrimp, chicken, and liver.
The website cronometer.com is a great place to keep track of your intake of choline and folate. Choline is not included by default, so you will need to go into your profile settings and turn it on as a nutrient. Track your food intake for a few days or a week and see whether you are regularly low on folate and choline… then adjust accordingly.
Supplements:
Related Genes and Articles:
COMT Gene: Neurotransmitter Levels, Estrogen Metabolism, and SNPs
Lithium Orotate and Vitamin B12: Benefits for Mood and Cognitive Support