Key takeaways:
- Psoriasis is an autoimmune disease that affects about 7.5 million people in the US and has a strong genetic component.
- The immune system in psoriasis patients attacks skin cells, speeding up their turnover and causing dry, itchy patches.
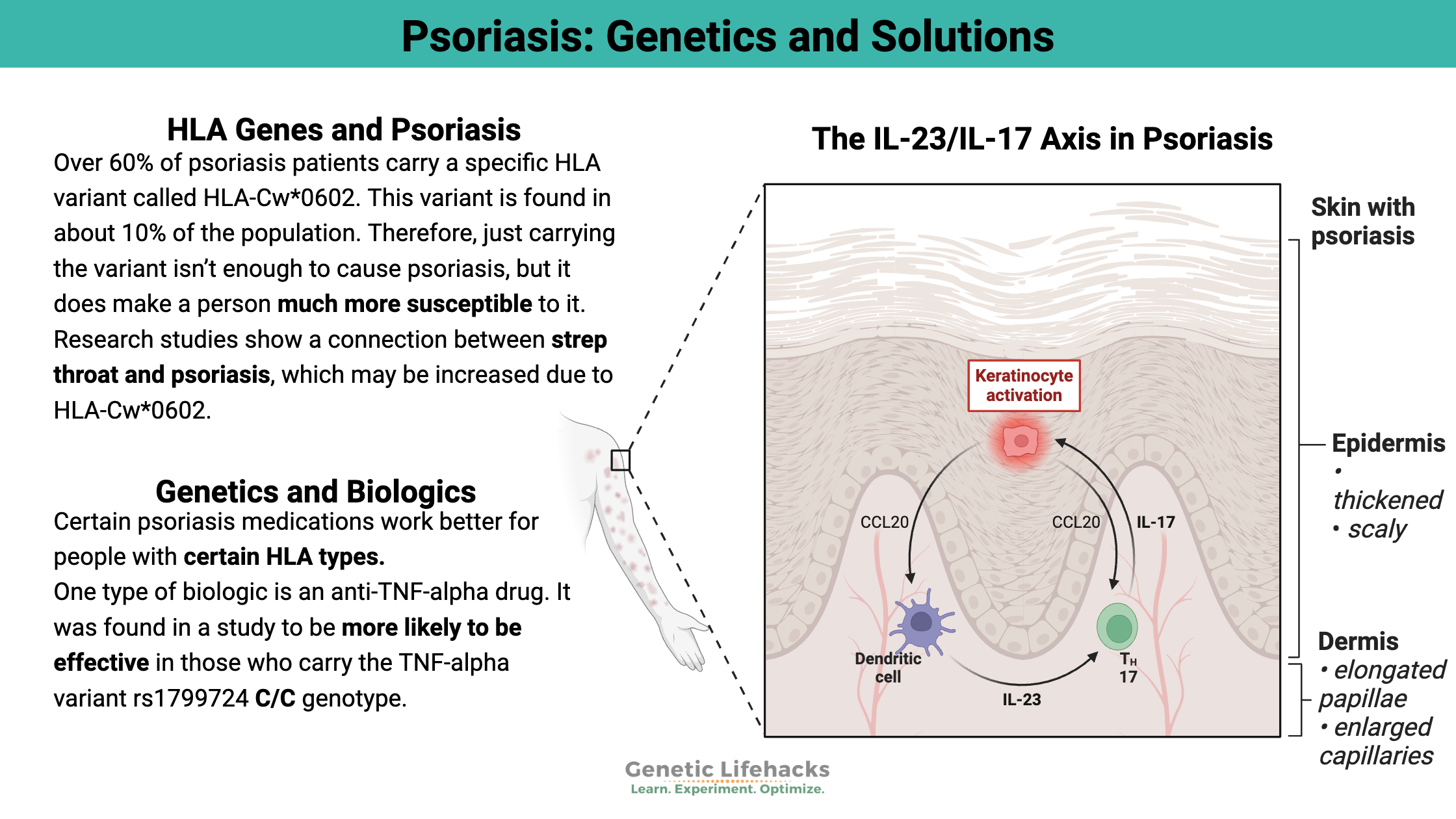
- Certain HLA genes, particularly HLA-Cw*0602, are linked to an increased risk of psoriasis.
- Genetic variants in genes like IL23, PTPN22, and IL-17F also influence psoriasis risk.
- Understanding the genetic pathways involved in your risk factors may help you to figure out the best individualized treatment options.
What causes psoriasis?
Psoriasis is an autoimmune condition that causes scaly, red patches of skin that can be itchy or painful. The immune system attacks the skin cells, causing a speed-up in the turnover of the cells. The National Psoriasis Foundation estimates that about 7.5 million people in the US have psoriasis.
There is a strong genetic component to psoriasis, and it tends to run in families. Along with the skin condition, other autoimmune conditions, such as Crohn’s disease, psoriatic arthritis, and uveitis, can be found more often in people with psoriasis.[ref][ref]
Human skin cells are in constant motion of shedding older cells and replacing them with new skin cells about once a month. However, for people with psoriasis, the turnover rate for skin cells can be as fast as 3-4 days, with the dead cells building up and flaking off in itchy, dry patches.[ref]
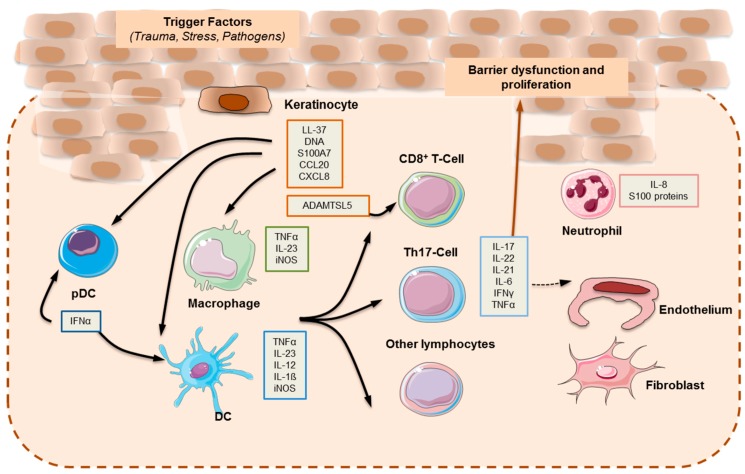
The outermost layer of skin is made up of keratinocytes, and in psoriasis, these skin cells interact with cells spanning the dermal layers, allowing inflammatory cells to interact with the skin barrier.
Psoriasis often starts with a triggering factor, such as a wound, stressor, or pathogen, that then activates immune cells known as dendritic cells. A cascade of events takes place in the adaptive immune response that results in elevated inflammatory cytokines, including IL-17, IL-21, IL-22, TNF-alpha, and interferon-gamma.[ref]
The skin microbiome plays a role for some people with psoriasis. The bacteria that reside on the skin help to maintain immune system homeostasis, and studies show that the cutaneous (skin) microbiome is out of balance in psoriasis flare-ups. There is a positive feedback loop between IL-17A in the skin and Staphylococcus that promotes the expression of multiple inflammatory cytokines.[ref]
HLA genes and psoriasis:
The HLA genes code for proteins that are a big part of our immune system, known as the major histocompatibility complex(MHC), which helps the body identify foreign invaders. There are six different HLA class I genes (A, B, C, E, F, and G) and five different HLA class II genes (DM, DO, DQ, DP, and DR). (Here is a good video on the HLA family for those who want to learn more.)
There are a lot of genetic differences within the HLA genes, leading to some people being more susceptible to certain conditions, while also being less susceptible to something else.
Tradeoffs: The variability of HLA genes is a tradeoff that keeps our population as a whole thriving — some of us are great at fighting off the herpes virus, while others are less susceptible to getting tuberculosis or leprosy.
In fact, some researchers hypothesize that the HLA type susceptible to psoriasis is prevalent in humans because it is protective for leprosy.[ref]
Different HLA genes are often associated with autoimmune diseases. For example, HLA-DQ2 is implicated in susceptibility to celiac disease, and HLA-B27 is tied to several different autoimmune diseases. There is also a link between IBD (Crohn’s disease and ulcerative colitis) and psoriasis.[ref]
Susceptibility to psoriasis is linked to a couple of HLA genes. Just carrying the HLA type is not enough to cause psoriasis by itself, so the genetic variants act together with other genes or environmental factors to cause psoriasis.
One of the HLA types strongly associated with an increased risk of psoriasis is HLA-Cw*0602. Research studies show a connection between strep throat and psoriasis, which may be increased due to HLA-Cw*0602:
- People with HLA-Cw*0602 are twice as likely to have a positive throat swab for Streptococcus at the onset of psoriasis symptoms.[ref]
- A small study found that people with two copies of the HLA-Cw*0602 serotype had a much greater improvement in their psoriasis after a tonsillectomy than those without the HLA-Cw type. [ref]
Environmental triggers of psoriasis:
Genetic susceptibility is only part of the picture in psoriasis. Environmental and lifestyle factors also play a role. A common theme for these environmental factors is that they initiate an immune response that then goes a bit awry.
Triggers that cause or exacerbate psoriasis include:[ref]
- Infections (Strep, Staph, Candida)
- Injury or skin irritation
- Radiotherapy or UV-B radiation
- Medications
- Vaccinations (BCG, flu, adenovirus, DPT)
- Smoking, alcohol consumption
- Obesity, diabetes
Medications identified as causing or exacerbating psoriasis: [ref]
- β-blockers
- lithium
- anti-malarial drugs
- interferons
- imiquimod
- ACE inhibitors
- terbinafine
- tetracycline
- nonsteroidal anti-inflammatory drugs (NSAIDs)
- fibrate drugs
More than just a skin disease:
While psoriasis typically affects the skin, the autoimmune inflammation can also affect other systems in the body, including: [ref]
- Vascular inflammation and heart disease
- Increased risk of metabolic syndrome, diabetes
- Joint and tendon inflammation
- Systemic inflammation
- Changes in the finger or toenails
How is psoriasis treated?
The most common option for psoriasis patients is drugs referred to as biologics or monoclonal antibodies. These can be a great help… sometimes. Genetic variants in inflammatory genes, like TNF-alpha, have been shown in research studies to impact the efficacy of different drugs for psoriasis. Some of these variants are included below in the genotype report section, with information that you can talk with your doctor about. Also, below in the Lifehacks section are natural options for treating or preventing flare-ups.
Genotype report: Psoriasis Genes
Overview of genetic risk factors:
| Gene | Role in Psoriasis | Additional Notes |
|---|---|---|
| HLA-Cw*0602 | Strongly increases risk | Also linked to medication response |
| IL23 | Influences the immune pathway | Target of some biologic drugs |
| PTPN22 | Modulates immune cell activity | Associated with other autoimmune diseases |
| IL-17F | Involved in the inflammatory response | Targeted by new therapies |
| TNF | Predicts better response to anti-TNF drugs | May help guide treatment choices |
Access this content:
An active subscription is required to access this content.
Lifehacks:
Natural options for treating psoriasis:
Dietary interventions:
A study of 1,206 psoriasis patients found that several dietary modifications were effective.[ref]
- Reducing alcohol use helped 54% of patients.
- Cutting out gluten and/or nightshades helped over half of the patients.
- Adding fish oil, more vegetables, and vitamin D helped around 40% of the patients.
When looking at magnesium deficiency scores, researchers found that individuals with low magnesium scores had a 75% increased relative risk of psoriasis.[ref] Foods high in magnesium include leafy greens (spinach, Swiss chard), nuts (almonds, cashews), pumpkin seeds, legumes, dark chocolate, and avocados.
Related articles w/ genetic connections: Nightshade sensitivity, vitamin D genes, fish oil, and magnesium
Probiotics:
A 2019 randomized, placebo-controlled clinical trial found that a probiotic mixture of Bifidobacterium longum and Lactobacillus rhamnosus was effective in controlling psoriasis for two-thirds of the study participants. [ref]
Natural supplements for psoriasis:
Quercetin reduces TNF:
Several animal studies show that quercetin reduces levels of TNF-alpha and NF-kappa beta in models of psoriasis.[ref]
A 2025 study in patients with psoriasis found that “… quercetin in particular is capable of suppressing cellular production of NO, TNF‑α and IL-6 and regulating the IL-23/IL-17A inflammatory axis by mediating STAT3 phosphorylation to inhibit inflammatory response.” [ref]
Related article: Read more about Quercetin, doses, absorption, etc
Luteolin:
A human cell study of psoriasis patients found that luteolin was effective in reducing NF-κB and TNF-alpha. [ref]
Berberine:
Berberine, a natural supplement from Oregon grape leaf, decreases psoriasis symptoms when used topically.[ref][ref]
Sea Buckthorn Oil:
A natural anti-inflammatory, sea buckthorn oil has been shown to help with the skin inflammation involved in psoriasis.[ref] It is available online – check the reviews of the different brands.
Curcumin:
Curcumin has been shown in multiple studies and clinical trials to reduce the inflammation of psoriasis. Human studies usually use oral curcumin supplements, and animal studies use topical curcumin. It is a TNF-alpha inhibitor as well as tamping down other aspects of inflammation.[ref][ref][ref]
Related article: Curcumin Supplements – Decreasing Inflammation
Curcumin + Blue light:
A 2026 study in animals showed that topical curcumin, along with blue light, restored the skin microbiome to a healthy state in psoriasis. The study showed that the combination inhibited IL-17A, reduced Staph and Streptococcus species, and also increased nitric oxide. [ref]
Sulforaphane:
Sulforaphane is a compound found in cruciferous vegetables that upregulates antioxidant defense pathways in the body. Animal models of psoriasis show positive results with sulforaphane treatment.[ref]
Vitamin B12:
Studies show that vitamin B12 may help, especially if you are low in B12.[ref]
Related article: Vitamin B12 genes.
Nigella sativa:
Also called black cumin seed oil, Nigella sativa has been shown in animal studies to reduce or eliminate psoriasis. The studies showed that both topical and oral routes were effective (in mice). [ref][ref] Black seed oil is readily available online and in health stores.
Negative studies:
Knowing what is less likely to be effective can help you prioritize which solutions to try first.
CBD oil:
Topical CBD did not lead to statistical improvement in psoriasis scores, although it did help some with itching.[ref]
Check homocysteine levels:
Studies show that psoriasis patients tend to have high homocysteine levels compared to controls. In some studies, the severity of psoriasis directly correlates with homocysteine levels.[ref]
You can get a blood test to know your homocysteine levels. If your doctor can’t order it for you, you can get it through UltaLabTests ($34) or another online lab company in the US. Supplementing with folate (B9), vitamin B6, and riboflavin helps to lower homocysteine for many people.
Related article: Homocysteine SNPs
Recap of your genes:
| Gene | RS ID | Your Genotype | Effect Allele | Effect Allele Frequency | Notes About Effect Allele |
|---|---|---|---|---|---|
| HLA-C | rs10484554 | -- | T | 0.14 | Increased risk of psoriasis |
| HLA-C | rs1265181 | -- | C | 0.2 | Increased risk of psoriasis |
| HLA-B*5701 | rs2395029 | -- | G | 0.03 | Increased risk of psoriasis |
| IL23 | rs11209026 | -- | A | 0.06 | Decreased risk of psoriasis |
| PTPN22 | rs1217414 | -- | A | 0.3 | AA: increased risk of psoriasis |
| L12B | rs4085613 | -- | T | 0.37 | Increased risk of psoriasis |
| IL-17F | rs763780 | -- | C | 0.06 | Increased risk of psoriasis, increased risk of rheumatoid arthritis, increased risk of autoimmune thyroid disease |
| HLA-C | rs4406273 | -- | A | 0.08 | HLA-Cw*0602; increased relative risk of psoriasis |
| TNF | rs1799724 | -- | T | 0.11 | TT and CT: anti-TNF-alpha biologic less likely to be effective; CC: anti-TNF-alpha biologic more likely to be effective |
| TNF | rs1800629 | -- | A | 0.15 | Higher TNF levels, not as good of a response to anti-TNF biologics |
| TNF | rs361525 | -- | A | 0.05 | Higher TNF levels, increased risk of psoriasis, not as good of a response to anti-TNF biologics |
| TNFRSF1B | rs1061622 | -- | G | 0.23 | Increase TNF receptor; not as good of a response to anti-TNF biologics |
| MIR146A | rs2910164 | -- | C | 0.24 | increased relative risk of psoriasis |
| CIAS1 | rs10754558 | -- | C | 0.61 | higher inflammation, increased relative risk of psoriasis, less response to psoriasis medication |
[/mepr-show]
Related Articles and Topics:
Familial Mediterranean Fever: Mimics fibromyalgia, arthritis, inflammation