Key takeaways:
~ Creatine acts as a backup energy source for muscles and the brain to use in times of stress.
~ Genetic variants in genes related to creatine creation can impact muscle pain, athletic performance, and cognitive ability.
~ Creatine supplements are inexpensive and readily available. Studies show that creatine monohydrate supplementation effectively boosts muscle power and brain creatine levels under certain conditions.
Members will see their genotype report below, plus additional solutions in the Lifehacks section. Consider joining today.
What is creatine?
Creatine is an amino acid that plays an important role in energy production within both brain tissue and muscles. Let’s take a look first at how cells produce energy.
Adenosine triposphate (ATP) is at the heart of cellular energy. ATP is primarily produce in mitochondria — you know, the powerhouse of the cell. ATP stores energy in the bonds between the phosphates, which store and then can release energy within the cell.
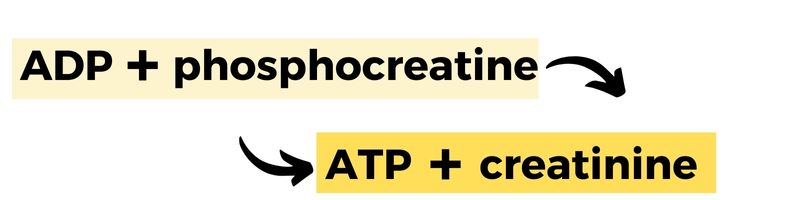
The ‘triphosphate’ part of ATP means it has three phosphates bound together. When ATP releases energy, it sheds one of its phosphates and becomes adenosinediphosphate (ADP) with only two phosphates remaining. Here’s where creatine comes in. In specific cell types, creatine helps recycle ADP back into ATP by donating a phosphate group. Thus, creatine can help replenishing cellular energy when it’s running low.
How does the body make creatine?
While creatine supplements are typically associated with bodybuilders, it is actually utilized in all types of muscles and the brain.
Creatine is synthesized from the amino acids glycine and arginine, along with a methyl group donated by SAMe.
The biosynthesis of creatine is a multi-step process.
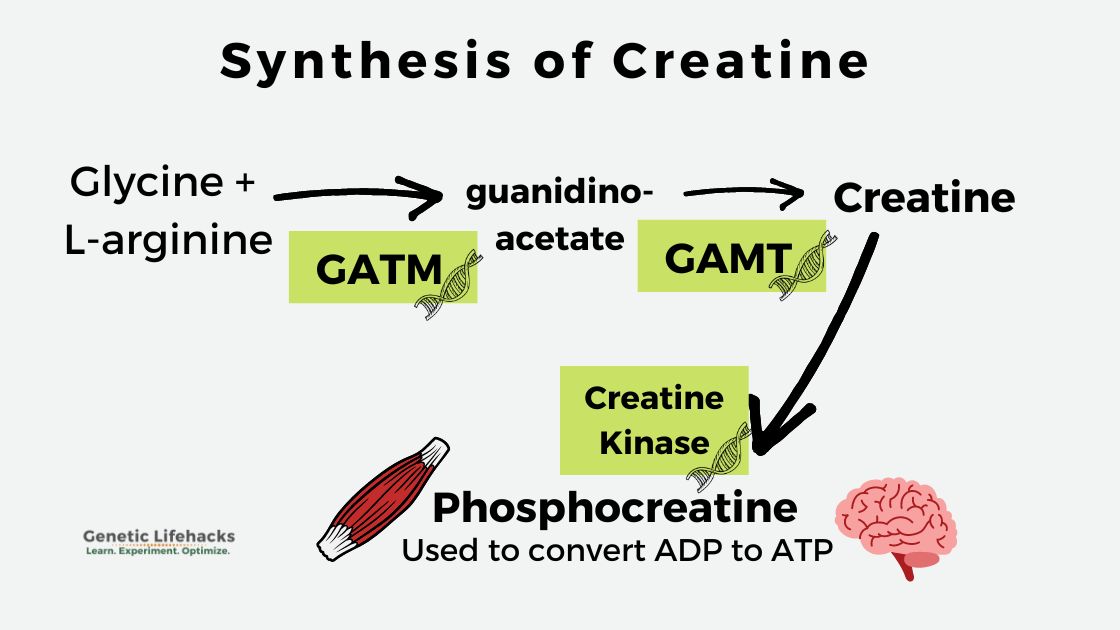
First, glycine and arginine, two common amino acids, combine to form guanidinoacetate. Then, creatine is formed from guanidinoacetate with the addition of a methyl group. This process occurs primarily in the liver and kidneys. Once synthesized, creatine then enters the bloodstream and can be used throughout the body.[ref]
Within cells, creatine can be further converted to phosphocreatine with the help of the enzyme creatine kinase (CK). Phosphocreatine, also known as creatine phosphate, stands ready, available for converting ADP to ATP when more energy is needed.
Muscle cells and the brain both need a lot of ATP for energy. When a lot of energy is required, such as lifting something heavy or sprinting, phosphocreatine rapidly replenishes ATP from ADP. In normal, lower-energy situations, ATP is produced directly from glucose or fatty acids.
In addition to being synthesized in the liver, creatine can be obtained from the diet as well as from supplements. Creatine is naturally found in animal protein-rich foods, such as muscle meats. Supplemental creatine, such as bodybuilders commonly use, is also a source of creatine for creating the phosphocreatine used when repairing and building muscles.
Diving deeper into creatine kinase:
I mentioned above that creatine kinase is the enzyme used to convert creatine to phosphocreatine, which can then be used by cells for energy when needed.
There are two types of creatine kinase – mitochondrial and cytosolic – found in the muscle and brain. The phosphocreatine created in the reaction acts as an energy buffer, readily available when muscle cells are stressed and need a burst of ATP for energy.[ref]
In medical contexts, doctors often measure creatine kinase levels in the blood to assess tissue damage, especially in cases like cardiac muscle damage during a heart attack. When tissues are harmed, creatine kinase can leak into the bloodstream, serving as a valuable indicator.
Lab tests for creatine kinase:
Doctors often measure creatine kinase levels in the blood to assess tissue damage. When tissues are damaged, creatine kinase will leak into the blood. For example, if cardiac muscle is damaged during a heart attack, creatine kinase levels will usually be elevated.[ref]
What else elevates creatine kinase (CK) levels on tests?
Aside from heart attacks, strenuous execise can elevate CK levels up to 15 times the normal level. For instance, after running a marathon, CK levels peak after 24 hours and remain elevated for a week.[ref]
Additional causes of elevated CK levels:
- Obesity and African descent are associated with higher CK levels.[ref]
- CK levels increase in response to brain, heart, or muscle damage.[ref]
- Statins can raise CK levels in people who have statin-induced muscle pain.[ref]
Creatine and Brain Function:
The brain, despite its relatively small size, uses up a ton of energy (ATP) in comparison with the rest of the body.
In the brain, creatine serves as an energy buffer to provide energy in times of stress.[ref] Genetic mutations which cause creatine deficiency in the brain result in severe developmental disorders and seizures.
Creatine obtained from diet or supplements can cross the blood-brain barrier, but the amount that reaches the brain is generally less than what is absorbed by muscles. This implies that to positively impact brain function, higher intake of creatine might be necessary. Alternatively, it could mean that creatine is prioritized by the muscles unless there is an urgent requirement for it to go to the brain.
As one research study puts it: “It could be that the brain relies primarily on endogenous creatine synthesis until there is some sort of challenge to brain creatine status. These challenges, which could cause a decrease in brain creatine, could be acute (e.g., sleep deprivation, intense exercise) or chronic (e.g., aging, traumatic brain injury, depression, Alzheimer’s disease, creatine synthesis enzyme deficiencies).”[ref]
Creatine and the Methylation Cycle:
The methylation cycle is a cellular process for producing methyl groups (a carbon + 3 hydrogen atoms) for use in many types of biochemical reactions. Both folate and choline are key contributors of methyl groups in the methylation cycle.
I mentioned above that one step in creatine biosynthesis includes a methyl group. A significant portion of the body’s methyl groups – about 40% – is dedicated to producing creatine.[ref]
When methyl groups are low, homocysteine levels often will be elevated. High homocysteine is linked to an elevated risk of heart problems.
Related article: Homocysteine, heart health, and more
A placebo-controlled clinical trial involving individuals engaged in resistance training showed that creatine supplementation over eight weeks reduced homocysteine levels.. The study used an initial dose of 25 g/d of creatine for the first five days, followed by 5 g/day for the rest of the trial.[ref]
Methyl groups also play a role in detoxification processes, including arsenic detoxification. A study found that in people with suboptimal intake of choline or folate, supplementing with creatine or folic acid helps aid the detox reaction for arsenic.[ref]
What happens if you don’t get creatine in your diet?
Creatine is not considered an essential amino acid, meaning you can make it in your body and don’t always have to get it for food.
However, getting creatine in your diet may prevent problems as you age or in times of physical stress.
A study of people over age 65 found that getting less than 1g of creatine via diet each day resulted in more than double the risk of angina (chest pain) and 2.5x the risk of liver problems.
The authors of the study concluded: “The considerable shortage of dietary creatine is associated with an increased risk of heart and liver conditions, which calls for public measures that foster diets rich in creatine-containing foods, and additional research to investigate the role of creatine in age-related diseases.”[ref]
Another study found that getting over 0.95g of creatine in foods daily was protective against cognitive decline in older adults.[ref]
Clinical trials using creatine supplements:
Creatine supplements have been very well studied, with thousands of clinical trials.
Here are just a few of the clinical trials:
- A double-blind, placebo-controlled safety trial using 0.3g/kg of creatine per day in men found: “creatine monohydrate supplementation is safe for health and no detrimental effects on different organs and physiological systems were observed in our cohort of volunteers.”[ref]
- In healthy older adults (aged 50-71), creatine before resistance training increased lean muscle mass and decreased fat mass. The trial ran for 32 weeks and used 0.1g/kg of creatine, compared to a placebo.[ref]
- Vegetarians have lower creatine levels, on average. A study of supplemental creatine showed vegetarians had even greater increases in bench-press strength, lean tissue, and other biomarkers than did non-vegetarians. (Both groups on creatine had better results from resistance training than the vegetarian and non-vegetarian placebo groups.[ref]
- Creatine supplementation helped both men and women increase peak power in bench presses and back squats.[ref]
- Creatine plus electrolytes increased sprint cycling times in a double-blind, randomized control study.[ref]
- Under hypoxic (low oxygen) conditions, creatine helps with cognitive function. The study included 15 healthy adults who took creatine for seven days before the 90-minute hypoxia session.[ref]
Negative study results are also interesting:
- Creatine supplementation did not significantly improve bone health in menopausal women with osteopenia.[ref]
- In fibromyalgia patients, creatine supplementation increased muscle strength, but it didn’t reduce pain or improve quality of life.[ref]
Creatine in adipose (fat) tissue:
In fat cells (adipose tissue), creatine is important in thermogenic respiration. Loss of creatine can decrease whole-body energy expenditure.[ref]
Brown or beige fat is the type of fat that creates heat in the body – especially in babies. Brown fat is darker in color than white adipose tissue (white fat) because it contains a huge number of mitochondria cranking out heat as a metabolic waste product.
Exposure to cold can trigger brown fat to produce more energy. It is essential in infants who are too young to shiver. The brown fat helps them to maintain their temperature.
In animal studies, creatine has been shown to enhance energy production when ADP is limited. When researchers limit creatine levels, the cells try to compensate by increasing the enzymes to produce more creatine. Animals lacking the creatine kinase enzyme had increased body weight and elevated fasting blood glucose.[ref][ref] The research here is new and evolving, but it looks like creatine plays a role in adaptation to cold, energy expenditure, and metabolic health.
Creatine for post-viral fatigue syndrome:
Post-viral fatigue syndrome is just what it sounds like – overwhelming fatigue that doesn’t end after you’ve gotten over a viral infection. It can refer to long covid or chronic fatigue syndrome (ME/CFS).
In people with post-viral fatigue syndrome (PVFS), muscle fatigue is reached much more rapidly than normal. It is thought that PVFS perturbs energy metabolism in the muscles. Research shows patients with chronic fatigue have reduced levels of hippocampal creatine also. While there is “not enough evidence to unequivocally endorse supplemental creatine for PVFS”, researchers do think it is possibly effective — as well as being low-risk and inexpensive.[ref]
Sarcopenia and creatine
Sarcopenia is the loss of muscle mass causing decreased strength in aging or chronic disease.
It is tempting to think creatine could be used to stop the aging effect on muscles, but research shows it isn’t quite that easy.
Studies in older adults show creatine supplementation alone has little effect on muscle function or mass. But… when creatine supplementation is added to weight training, the results show that it enhances the muscle’s response to training, potentially increasing capacity for higher intensity exercise and improving the muscle’s response post-exercise.[ref]
Thus, one way creatine may be beneficial in older adults is by increasing their capacity for exercising a little longer or lifting a little more weight. Even minor increases in exercise capacity can be important in older adults, and increasing muscle mass or grip strength can help with stability and independence.[ref]
Creatine Synthesis Genotype Report
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Member Content:
Why join Genetic Lifehacks?
~ Membership supports Genetic Lifehack's goal of explaining the latest health and genetics research.
~ It gives you access to the full article, including the Genotype and Lifehacks sections.
~ You'll see your genetic data in the articles and reports.
Join Here
Lifehacks:
The estimated daily requirement for creatine for an adult male weighing 70kg (154 lbs) is about 2g. Half of this usually comes from the diet, with the other half being synthesized from arginine plus glycine.[ref]
Foods high in creatine
Animal proteins:
- One pound of beef contains around 5 grams of creatine.
- Fish is also an excellent source of creatine, with about 4.5 grams in one pound of salmon.[ref]
| Food | Creatine Content (per 100g) |
|---|---|
| Beef (cooked) | 2-5g |
| Pork (cooked) | 1-2g |
| Chicken (cooked) | 0.3-0.5g |
| Salmon (cooked) | 0.4-0.9g |
| Tuna (cooked) | 0.3-0.4g |
| Herring (cooked) | 0.4-0.6g |
| Cod (cooked) | 0.1-0.3g |
| Shrimp (cooked) | 0.1-0.2g |
| Turkey (cooked) | 0.1-0.3g |
| Rabbit (cooked) | 0.1-0.2g |
| Venison (cooked) | 2-5g |
| Pork liver (cooked) | 3-4g |
| Beef liver (cooked) | 3-5g |
| Chicken breast (raw) | 0.1-0.2g |
| Tofu (cooked) | 0.1-0.2g |
| Cottage cheese | 0.1-0.5g |
| Milk | 0.1-0.5g |
| Yogurt | 0.1-0.5g |
| Parsley | 0.3-0.5g |
| Wheat germ | 0.2-0.3g |
If you aren’t eating animal-based protein-containing creatine, you may want to consider supplementing – especially if you are concerned about muscle mass or sarcopenia. Vegetarians, for example, usually have lower plasma and muscle levels of creatine.[ref]
Keep in mind: Creatine is synthesized from the amino acids arginine and glycine. You may also want to consider supplemental creatine if you don’t get a lot of those amino acids in your diet.
You may also want to consider supplemental creatine if you have any genetic variants related to lower creatine creation.
Let’s dig into the research on creatine supplements – how much, how often, and how is it absorbed:
Creatine monohydrate supplementation: Safety and Benefits
Creatine monohydrate comes as a flavorless powder and easily mixes into water or a drink, or you can get it in flavored drink mixes.
Does supplemental creatine work?
There is quite a bit of research showing supplemental creatine is beneficial in exercise and in strength training. It isn’t a miracle supplement that will make you look like Arnold Swartzenegar, but hundreds of research studies show it gives a bit of a muscle-building and muscle-repair boost.
You may have read that creatine supplements can cause weight gain. Researchers think the initial weight gain sometimes noticed with higher doses comes from increased water weight and not from increased body fat.[ref]
Safety:
As with all supplements, choose a high-quality brand to avoid contaminants. Labdoor is one company independently testing the purity of different creatine brands.
Studies often use a large loading dose of 20g/day for 5-7 days, followed by chronic dosing of 3-5g/day with no safety issues.
Safety assessments show creatine is safe at doses of up to 5g/day for long-term supplementation in healthy adults.[ref]
If you have health concerns, especially kidney disease, you should talk with your doctor to be sure that creatine is safe for you. The studies on healthy people show creatine to be safe, but there are a few case studies with chronic kidney disease patients having problems with supplemental creatine.[ref]
Also, talk with your doctor if you have asthma. Studies in mice show that creatine may exacerbate airway sensitivity.[ref]
Just to note: Anecdotal reports on the web mention gastrointestinal distress when using higher doses too quickly. If you aren’t using creatine for bodybuilding and find it gives you intestinal issues, try going with the lower doses to start with.
Member Content:
Why join Genetic Lifehacks?
~ Membership supports Genetic Lifehack's goal of explaining the latest health and genetics research.
~ It gives you access to the full article, including the Genotype and Lifehacks sections.
~ You'll see your genetic data in the articles and reports.
Join Here
Related Articles and Topics:
ACTN3: Muscle type
The ACTN3 gene impacts fast-twitch muscle creation that is utilized in power sports. A common variant causes this gene not to function.
Brain Fog: Causes, genetics, and individualized solutions
Explore brain fog in detail, looking at the physiological causes, genetic susceptibility, and personalized solutions.
Intelligence Genes
Hundreds of identified genes influence intelligence, from IQ scores to musical ability. Learn more about your intelligence strengths and ways to enhance your cognitive function.
Which type of choline works best with your genes?
Choline is an often neglected nutrient essential to a healthy diet. Your genes are important in how much and which types of choline you need.
References:
Alessandrì, Maria Grazia, et al. “Increased Creatine Demand during Pregnancy in Arginine: Glycine Amidino-Transferase Deficiency: A Case Report.” BMC Pregnancy and Childbirth, vol. 20, no. 1, Sept. 2020, p. 506. PubMed, https://doi.org/10.1186/s12884-020-03192-4.
Almeida, Douglas, et al. “Creatine Supplementation Improves Performance, but Is It Safe? Double-Blind Placebo-Controlled Study.” The Journal of Sports Medicine and Physical Fitness, vol. 60, no. 7, July 2020, pp. 1034–39. PubMed, https://doi.org/10.23736/S0022-4707.20.10437-7.
Alves, Christiano R. R., et al. “Creatine Supplementation in Fibromyalgia: A Randomized, Double-Blind, Placebo-Controlled Trial.” Arthritis Care & Research, vol. 65, no. 9, Sept. 2013, pp. 1449–59. PubMed, https://doi.org/10.1002/acr.22020.
Assanangkornchai, N., et al. “Characteristics of Trauma Patients with Creatine Kinase Elevation.” Critical Care, vol. 19, no. Suppl 1, 2015, p. P282. PubMed Central, https://doi.org/10.1186/cc14362.
Balberova, Olga V., et al. “Candidate Genes of Regulation of Skeletal Muscle Energy Metabolism in Athletes.” Genes, vol. 12, no. 11, Oct. 2021, p. 1682. PubMed Central, https://doi.org/10.3390/genes12111682.
Bereket-Yücel, S. “Creatine Supplementation Alters Homocysteine Level in Resistance Trained Men.” The Journal of Sports Medicine and Physical Fitness, vol. 55, no. 4, Apr. 2015, pp. 313–19.
Bozack, Anne K., et al. “Betaine and Choline Status Modify the Effects of Folic Acid and Creatine Supplementation on Arsenic Methylation in a Randomized Controlled Trial of Bangladeshi Adults.” European Journal of Nutrition, vol. 60, no. 4, June 2021, pp. 1921–34. PubMed, https://doi.org/10.1007/s00394-020-02377-z.
Brosnan, John T., et al. “The Metabolic Burden of Creatine Synthesis.” Amino Acids, vol. 40, no. 5, May 2011, pp. 1325–31. PubMed, https://doi.org/10.1007/s00726-011-0853-y.
Brosnan, Margaret E., and John T. Brosnan. “The Role of Dietary Creatine.” Amino Acids, vol. 48, no. 8, Aug. 2016, pp. 1785–91. PubMed, https://doi.org/10.1007/s00726-016-2188-1.
Burke, Darren G., et al. “Effect of Creatine and Weight Training on Muscle Creatine and Performance in Vegetarians.” Medicine and Science in Sports and Exercise, vol. 35, no. 11, Nov. 2003, pp. 1946–55. PubMed, https://doi.org/10.1249/01.MSS.0000093614.17517.79.
Cabaniss, C. Daniel. “Creatine Kinase.” Clinical Methods: The History, Physical, and Laboratory Examinations, edited by H. Kenneth Walker et al., 3rd ed., Butterworths, 1990. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK352/.
Candow, Darren G., et al. “Strategic Creatine Supplementation and Resistance Training in Healthy Older Adults.” Applied Physiology, Nutrition, and Metabolism = Physiologie Appliquee, Nutrition Et Metabolisme, vol. 40, no. 7, July 2015, pp. 689–94. PubMed, https://doi.org/10.1139/apnm-2014-0498.
Chiou, W. L., and F. H. Hsu. “Pharmacokinetics of Creatinine in Man and Its Implications in the Monitoring of Renal Function and in Dosage Regimen Modifications in Patients with Renal Insufficiency.” Journal of Clinical Pharmacology, vol. 15, no. 5–6, June 1975, pp. 427–34. PubMed, https://doi.org/10.1002/j.1552-4604.1975.tb02364.x.
Crisafulli, Daniel L., et al. “Creatine-Electrolyte Supplementation Improves Repeated Sprint Cycling Performance: A Double Blind Randomized Control Study.” Journal of the International Society of Sports Nutrition, vol. 15, 2018, p. 21. PubMed, https://doi.org/10.1186/s12970-018-0226-y.
Dolan, Eimear, et al. “Muscular Atrophy and Sarcopenia in the Elderly: Is There a Role for Creatine Supplementation?” Biomolecules, vol. 9, no. 11, Oct. 2019, p. E642. PubMed, https://doi.org/10.3390/biom9110642.
Doma, Kenji, et al. “The Paradoxical Effect of Creatine Monohydrate on Muscle Damage Markers: A Systematic Review and Meta-Analysis.” Sports Medicine, vol. 52, no. 7, July 2022, pp. 1623–45. Springer Link, https://doi.org/10.1007/s40279-022-01640-z.
Dubé, Marie-Pierre, et al. “CKM and LILRB5 Are Associated with Serum Levels of Creatine Kinase.” Circulation. Cardiovascular Genetics, vol. 7, no. 6, Dec. 2014, pp. 880–86. PubMed, https://doi.org/10.1161/CIRCGENETICS.113.000395.
Fernández-Torres, Javier, et al. “Ancestral Contribution of the Muscle-Specific Creatine Kinase (CKM) Polymorphism Rs4884 in the Knee Osteoarthritis Risk: A Preliminary Study.” Clinical Rheumatology, vol. 40, no. 1, Jan. 2021, pp. 279–85. PubMed, https://doi.org/10.1007/s10067-020-05238-6.
Forbes, Scott C., et al. “Effects of Creatine Supplementation on Brain Function and Health.” Nutrients, vol. 14, no. 5, Feb. 2022, p. 921. PubMed Central, https://doi.org/10.3390/nu14050921.
George, Michael D., et al. “Creatine Kinase in the U.S. Population: Impact of Demographics, Comorbidities, and Body Composition on the Normal Range.” Medicine, vol. 95, no. 33, Aug. 2016, p. e4344. PubMed, https://doi.org/10.1097/MD.0000000000004344.
Horino, Masato, et al. “The Role of Thermogenic Fat Tissue in Energy Consumption.” Current Issues in Molecular Biology, vol. 44, no. 7, July 2022, pp. 3166–79. PubMed Central, https://doi.org/10.3390/cimb44070219.
Hummer, Erik, et al. “Creatine Electrolyte Supplement Improves Anaerobic Power and Strength: A Randomized Double-Blind Control Study.” Journal of the International Society of Sports Nutrition, vol. 16, no. 1, May 2019, p. 24. PubMed, https://doi.org/10.1186/s12970-019-0291-x.
Kazak, Lawrence, et al. “A Creatine-Driven Substrate Cycle Enhances Energy Expenditure and Thermogenesis in Beige Fat.” Cell, vol. 163, no. 3, Oct. 2015, pp. 643–55. PubMed Central, https://doi.org/10.1016/j.cell.2015.09.035.
Kazak, Lawrence, and Paul Cohen. “Creatine Metabolism: Energy Homeostasis, Immunity and Cancer Biology.” Nature Reviews. Endocrinology, vol. 16, no. 8, Aug. 2020, pp. 421–36. PubMed, https://doi.org/10.1038/s41574-020-0365-5.
Kobayashi, Yoshio, et al. “Effect of a Marathon Run on Serum Lipoproteins, Creatine Kinase, and Lactate Dehydrogenase in Recreational Runners.” Research Quarterly for Exercise and Sport, vol. 76, no. 4, Dec. 2005, pp. 450–55. PubMed, https://doi.org/10.1080/02701367.2005.10599318.
Mangravite, Lara M., et al. “A Statin-Dependent QTL for GATM Expression Is Associated with Statin-Induced Myopathy.” Nature, vol. 502, no. 7471, Oct. 2013, pp. 377–80. PubMed Central, https://doi.org/10.1038/nature12508.
McMorris, Terry, et al. “Creatine Supplementation and Cognitive Performance in Elderly Individuals.” Neuropsychology, Development, and Cognition. Section B, Aging, Neuropsychology and Cognition, vol. 14, no. 5, Sept. 2007, pp. 517–28. PubMed, https://doi.org/10.1080/13825580600788100.
NM_001482.3(GATM):C.446G>A (p.Trp149Ter) AND Arginine:Glycine Amidinotransferase Deficiency – ClinVar – NCBI. https://www.ncbi.nlm.nih.gov/clinvar/112859991/. Accessed 15 Nov. 2022.
Ostojic, Sergej M. “Diagnostic and Pharmacological Potency of Creatine in Post-Viral Fatigue Syndrome.” Nutrients, vol. 13, no. 2, Feb. 2021, p. 503. PubMed Central, https://doi.org/10.3390/nu13020503.
—. “Dietary Creatine and Cognitive Function in U.S. Adults Aged 60 Years and Over.” Aging Clinical and Experimental Research, vol. 33, no. 12, Dec. 2021, pp. 3269–74. PubMed, https://doi.org/10.1007/s40520-021-01857-4.
—. “Dietary Intake of Creatine and Risk of Medical Conditions in U.S. Older Men and Women: Data from the 2017-2018 National Health and Nutrition Examination Survey.” Food Science & Nutrition, vol. 9, no. 10, Oct. 2021, pp. 5746–54. PubMed, https://doi.org/10.1002/fsn3.2543.
Rawson, Eric S., et al. “Creatine Supplementation Does Not Improve Cognitive Function in Young Adults.” Physiology & Behavior, vol. 95, no. 1–2, Sept. 2008, pp. 130–34. PubMed, https://doi.org/10.1016/j.physbeh.2008.05.009.
Roschel, Hamilton, et al. “Creatine Supplementation and Brain Health.” Nutrients, vol. 13, no. 2, Feb. 2021, p. 586. PubMed, https://doi.org/10.3390/nu13020586.
Sales, Lucas Peixoto, et al. “Creatine Supplementation (3 g/d) and Bone Health in Older Women: A 2-Year, Randomized, Placebo-Controlled Trial.” The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, vol. 75, no. 5, Apr. 2020, pp. 931–38. PubMed, https://doi.org/10.1093/gerona/glz162.
Sarshin, Amir, et al. “Short-Term Co-Ingestion of Creatine and Sodium Bicarbonate Improves Anaerobic Performance in Trained Taekwondo Athletes.” Journal of the International Society of Sports Nutrition, vol. 18, no. 1, Jan. 2021, p. 10. PubMed, https://doi.org/10.1186/s12970-021-00407-7.
Schlattner, Uwe, et al. “Mitochondrial Creatine Kinase in Human Health and Disease.” Biochimica Et Biophysica Acta, vol. 1762, no. 2, Feb. 2006, pp. 164–80. PubMed, https://doi.org/10.1016/j.bbadis.2005.09.004.
Semeredi, Sasa, et al. “Guanidinoacetic Acid with Creatine Compared with Creatine Alone for Tissue Creatine Content, Hyperhomocysteinemia, and Exercise Performance: A Randomized, Double-Blind Superiority Trial.” Nutrition (Burbank, Los Angeles County, Calif.), vol. 57, Jan. 2019, pp. 162–66. PubMed, https://doi.org/10.1016/j.nut.2018.04.009.
Shao, Andrew, and John N. Hathcock. “Risk Assessment for Creatine Monohydrate.” Regulatory Toxicology and Pharmacology: RTP, vol. 45, no. 3, Aug. 2006, pp. 242–51. PubMed, https://doi.org/10.1016/j.yrtph.2006.05.005.
Taylor, Beth A., et al. “Increased Creatine Kinase with Statin Treatment May Identify Statin-Associated Muscle Symptoms.” International Journal of Cardiology, vol. 209, Apr. 2016, pp. 12–13. PubMed Central, https://doi.org/10.1016/j.ijcard.2016.02.028.
Toniolo, Ricardo Alexandre, Michelle Silva, et al. “A Randomized, Double-Blind, Placebo-Controlled, Proof-of-Concept Trial of Creatine Monohydrate as Adjunctive Treatment for Bipolar Depression.” Journal of Neural Transmission (Vienna, Austria: 1996), vol. 125, no. 2, Feb. 2018, pp. 247–57. PubMed, https://doi.org/10.1007/s00702-017-1817-5.
Toniolo, Ricardo Alexandre, Francy de Brito Ferreira Fernandes, et al. “Cognitive Effects of Creatine Monohydrate Adjunctive Therapy in Patients with Bipolar Depression: Results from a Randomized, Double-Blind, Placebo-Controlled Trial.” Journal of Affective Disorders, vol. 224, Dec. 2017, pp. 69–75. PubMed, https://doi.org/10.1016/j.jad.2016.11.029.
Turner, Clare E., et al. “Creatine Supplementation Enhances Corticomotor Excitability and Cognitive Performance during Oxygen Deprivation.” The Journal of Neuroscience: The Official Journal of the Society for Neuroscience, vol. 35, no. 4, Jan. 2015, pp. 1773–80. PubMed, https://doi.org/10.1523/JNEUROSCI.3113-14.2015.
Wallace, B., et al. “Common Creatine Kinase Gene Mutation Results in Falsely Reassuring CK Levels in Muscle Disorders.” QJM: An International Journal of Medicine, vol. 109, no. 6, June 2016, pp. 413–14. PubMed Central, https://doi.org/10.1093/qjmed/hcv215.
Youn, Bo-Young, et al. “Genetic Basis of Elite Combat Sports Athletes: A Systematic Review.” Biology of Sport, vol. 38, no. 4, Oct. 2021, pp. 667–75. PubMed Central, https://doi.org/10.5114/biolsport.2022.102864.