Key takeaways:
~IL-17 is a proinflammatory cytokine produced by T cells, including Th17 cells.
~ IL-17 is produced to fight off pathogens, such as tuberculosis or
~ Some people have a more sensitive immune system and are more prone to inflammatory reactions. Variants in the IL17 genes are part of this. Members will see their genotype report below and the solutions in the Lifehacks section. Consider joining today.
Inflammation and IL-17:
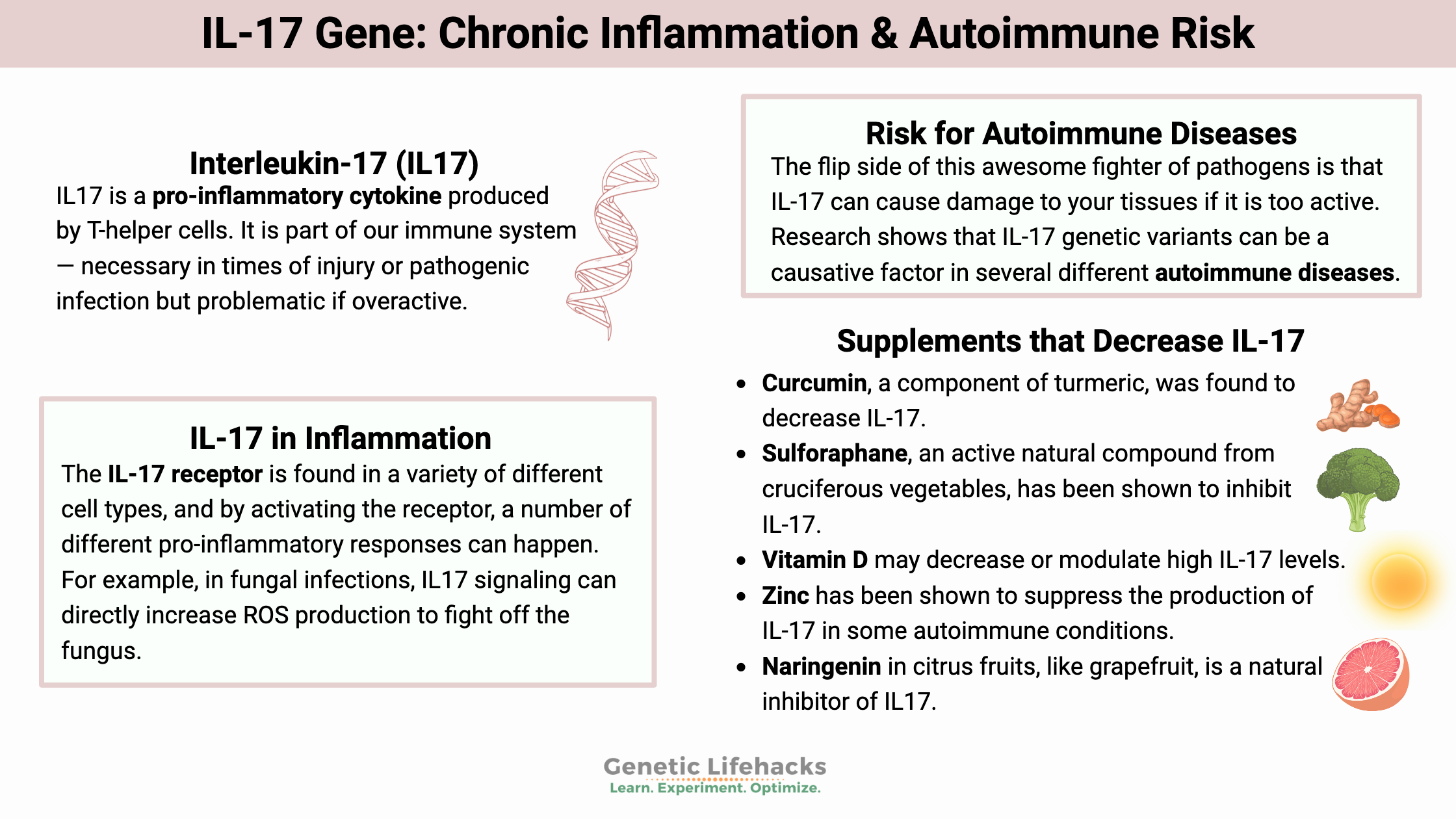
Interleukin-17 (IL17) is a pro-inflammatory cytokine produced by T-helper cells. It is part of our immune system — necessary in times of injury or pathogenic infection but problematic if overactive.[ref]
A quick overview of the immune system:
Our immune system’s composition includes many different parts and is responsible both for fighting off foreign pathogens (bacteria, viruses, etc.) and clearing out old or defective cells in the body. Thus, the immune system needs to recognize which cells are pathogens and which cells are part of the body. T-cells, also called T-lymphocytes, are a type of white blood cell that seeks out and destroys pathogens. There are two types of T-cells, T-helper cells and T-effector cells. T helper cells help to organize the immune response against a pathogen.
Going a little deeper here… multiple types of T-helper cells secrete different cytokines needed for different types of immune responses. One of the T-helper cells is Th17, which secretes the inflammatory cytokine IL-17 (interleukin-17).[ref]
IL-17 in Inflammation and Autoimmunity:
IL-17, produced by Th17, is important in eliminating bacteria and fungi both inside cells and outside cells.[ref]
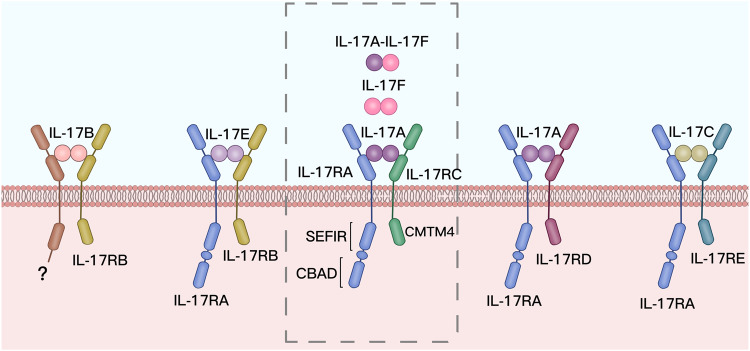
IL-17 has six different subtypes, from IL-17A to IL-17F. As inflammatory signaling molecules, both IL-17A and IL-17F act on the same receptor (IL-17R).
The IL-17 receptor is found in a variety of different cell types, and by activating the receptor, a number of different pro-inflammatory responses can happen. For example, in fungal infections, IL17 signaling can directly increase ROS production to fight off the fungus.[ref]
One of the main roles of IL17 is to protect ‘barrier integrity’ – the body’s front line against outside invaders. This means that the IL-17 receptor is found in skin tissue, mucosal tissue, the lungs, and other epithelial cells, such as those lining the intestines. One role of IL-17 is to maintain the tight junctions between the epithelial cells, and another action is to induce the release of antimicrobial chemokines in response to pathogens.[ref]
IL-17 is important in the defense against tuberculosis (Mycobacterium tuberculosis) and Staph infections on the skin. It is also important in fighting off fungal infections, such as Candida albicans. IL-17 is also important in your body’s defense against whooping cough.[ref] Thus, genetic variants that increased IL-17 were likely an advantage historically, when tuberculosis and pertussis were significant and common threats.
Increased risk for autoimmune diseases:
The flip side of this awesome fighter of pathogens is that IL-17 can cause damage to your tissues if it is too active. Research shows that IL-17 genetic variants can be a causative factor in several different autoimmune diseases.[ref][ref]
IL-17 is implicated in increasing the risk for several autoimmune diseases, including psoriasis, Hashimoto’s, and asthma. As mentioned above, IL-17 is mainly active in the epithelial and mucosal regions (lungs, gastrointestinal tract, skin), which explains its role in psoriasis, asthma, and other related conditions.
Genetic variants that increase the body’s production of IL-17A are a risk factor for inflammatory bowel disease (IBD), psoriasis, rheumatoid arthritis, bronchitis severity, gastric cancer, and more.
IL-17A is also implicated in celiac disease, with increased expression of IL-17A found in the intestinal mucosa of Celiac patients. Gluten sensitivity, though, was not found to increase IL-17A.[ref][ref]
IL-17 Genotype Report
There are genetic variations in IL-17 causing it to be either more active than normal (increasing risk of autoimmune/inflammatory conditions) – OR – less active than normal (protective against autoimmune/inflammatory conditions).
As is almost always the case, diet and environment interact with genetics in the development of chronic diseases. Thus, just carrying the variant doesn’t cause inflammatory diseases, per se, but instead increases the susceptibility to them in conjunction with other factors.
Lifehacks for decreasing high IL-17
Balance is key with the immune response – excess IL-17 is linked to autoimmune and inflammatory conditions, but IL-17 is also important in fighting off specific pathogens.
If you have an increased IL-17 response that is exacerbating an inflammatory condition, you may want to look into natural ways to decrease IL17.
Keep in mind that tamping down IL-17 may not be a good idea if you’re also trying to fight off a pathogen. Talk with your doctor if you have any questions about supplements and their interactions with medications.
Dietary Changes that Impact IL-17:
Salt increases IL-17:
Studies in mice show that a high-salt diet can increase the differentiation of Th17 cells and thus increase IL-17.[ref] If you have an autoimmune disease, track how much salt you get in your diet and talk with your doctor about whether you should try a low-salt diet.
Sprinkle on the spices:
Ursolic acid, which is a natural carboxylic acid found in rosemary and thyme, is a strong inhibitor of IL-17.[ref] It is also a component of rosemary extract, which was traditionally used for treating rashes, wounds, dyspepsia, etc.[ref]
Vitamin C appears to upregulate IL-17, which may be good when fighting off a pathogen.[ref] Some vitamin C is essential for your health and a complete lack of vitamin C results in scurvy. However, if you have an autoimmune disease related to high IL-17, you may want to take this as a heads-up to be on the alert for increased symptoms if supplementing with vitamin C.
An apple a day?
Apples contain high concentrations of procyanidin B1 and B2, which inhibit the production of IL17.[ref]
Statins and IL-17:
Statins can inhibit IL-17 secretion. This may be helpful in autoimmune diseases that are driven by IL-17, but it also may interact with the ability of IL-17 to fight off certain pathogens. [ref]
7 Natural supplements that decrease IL-17:
Related Articles and Topics:
Psoriasis Genes: How genetics point to individualized solutions
TNF-alpha: Inflammation, Chronic Diseases, and Genetic Susceptibility