Key takeaways:
~ Chronic sinus infections affect about 10% of the population.
~ Inflammation continues in the sinuses after an acute infection with a pathogen or allergies.
~ Genetic links to chronic inflammation point to specific solutions that may help.
Members will see their genotype report below, plus additional solutions in the Lifehacks section. Consider joining today.
What Causes Chronic Sinus Infections?
Doctors define chronic rhino-sinusitis as having inflamed sinuses (stuffiness, nasal discharge, and changes in the ability to smell) for 12 weeks or more. For many people, this can start with allergies or a cold that turns into a sinus infection that lingers on, never really clearing up and flaring up again periodically.
Chronic sinus infections often correlate with allergic rhinitis, frequent colds, atopic dermatitis, and asthma.[ref]
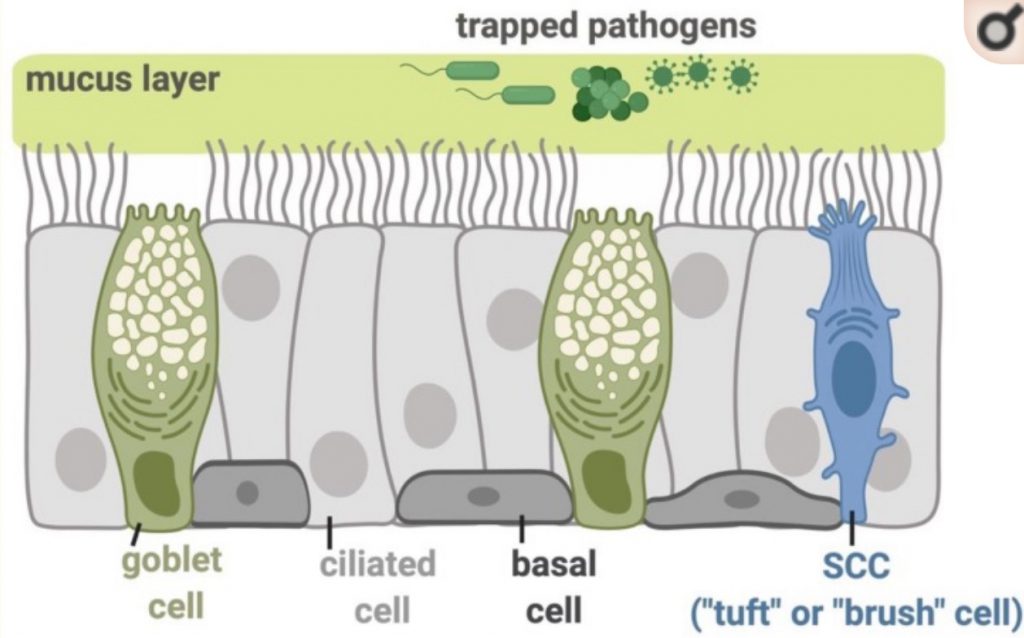
Your nose is constantly bringing in bacteria, fungi, and viruses. The first line of defense is the mucous membranes and cilia that clear out the particles coming into the nose.[ref]
In most people, the acute infection from a pathogen is not what continues to cause chronic sinus problems (defined as 12+ weeks). Instead, inflammation in the sinuses continues after a triggering episode (allergies, fungus, pathogen, etc.).[ref]
How do your genes influence sinus infections?
Genetics plays a role in the likelihood of having chronic sinus problems. The genetic component can range from genes that influence your inflammatory response to the mutations that cause cystic fibrosis or ciliary diseases.[ref]
When researchers investigate how genetics influences the risk of a condition, such as chronic sinus infections, they can go at this a couple of ways.
First, they can investigate whether specific genetic variants or mutations are more common in people with the condition. For example, researchers can look at people who carry one copy of the mutations that cause cystic fibrosis to see if they are linked to sinus infections. Or they can investigate genes related to immune response.
Another way to look at genetic connections is to do a ‘genome-wide association study’. These research studies involve looking at the whole genome of a large number of people and seeing if there is anything different about people with a particular condition. Lots of computing power is needed for these studies!
Genetic studies on chronic sinus infections:
Genome-wide studies link bitter taste receptor variants to susceptibility to chronic sinus infections.
You may be thinking – taste receptors in your nose? Researchers have discovered that taste receptors are found throughout the body and perform different functions. In your mouth, taste receptors are chemosensors abundant in taste bud cells. But these same receptors can detect secreted bacterial products in the nasal and sinus cavities and modulate the immune response.[ref]
The TAS2R38 gene codes for a bitter taste receptor. A fairly common variant in this gene causes some people not to taste certain bitter flavors. This lack of taste drives food preferences, to some extent, for things like bitter vegetables, coffee, and scotch.
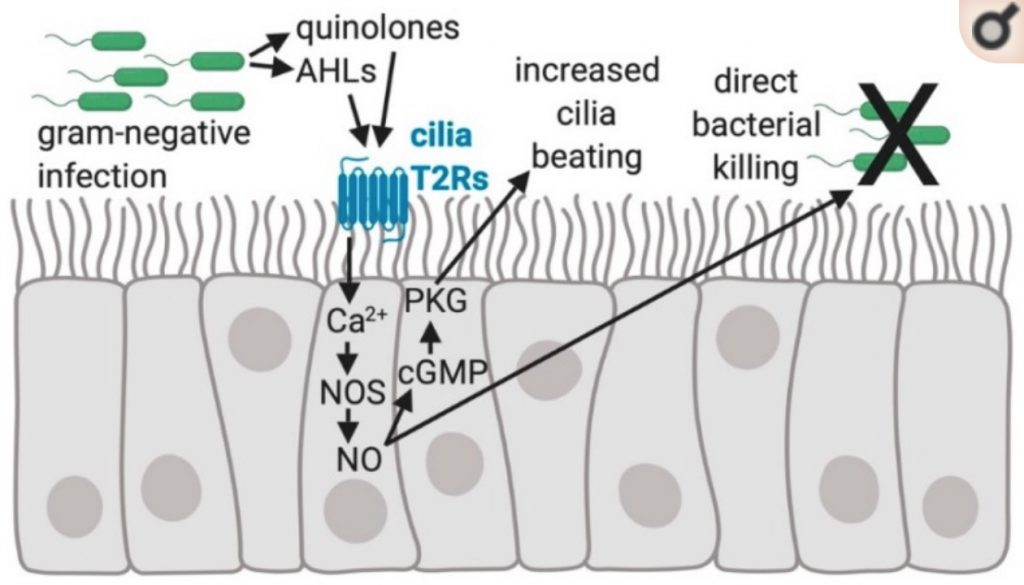
In the airways, though, it is thought that the TAS2R receptors are important for sensing specific gram-negative bacteria, including Pseudomonas aeruginosa, a multi-drug resistant pathogen.[ref]
When the TAS2R38 receptor is activated in the nasal passages, it causes the secretion of nitric oxide. The increase in nitric oxide causes two things to happen: first, it increases the movement of cilia in the nose; and second, it can directly kill bacteria.[ref]
Nasal polyps are a risk factor for chronic sinus infections. A genetic variant that causes the ALOX15 gene not to function is associated with a greatly decreased risk of both nasal polyps and chronic sinus infections. The ALOX15 gene codes for an enzyme that is important in the metabolism of polyunsaturated fats. It is also important in the inflammatory response to certain pathogens, including pathogens that cause periodontal disease, peritonitis, sepsis, and atherosclerosis.[ref] Specifically, ALOX15 helps to convert DHA, a polyunsaturated fat found in fish oil, into pro-resolving mediators that promote the resolution of inflammation. Read more about the resolution of inflammation.
Cystic fibrosis is a genetic disease causing an alteration to the thickness of mucous in the lungs, gut, and nasal passages. One complication of cystic fibrosis is chronic sinus infections, including those with drug-resistant P. aeruginosa. It is a big problem for people with cystic fibrosis because the pathogen can spread from the nose to the lungs, causing serious lung infections.[ref]
Alpha-1 antitrypsin deficiency is another genetic disease linked to an increased risk of chronic sinus infections. Mutations in the SERPINA1 gene cause alterations to the alpha-1 antitrypsin enzyme, which is active in the lungs at all times but is also part of the immune response against infections. People with Alpha-1 antitrypsin deficiency are at a greater risk for chronic rhinosinusitis.[ref]
Increased inflammatory response, both to pathogens and overall inflammation, is also implicated in chronic sinus infections. While many inflammatory cytokine-related genetic variants have been investigated, only a few studies have been replicated in more than one population group. However, the TNF-alpha variants have been found to increase the risk of chronic sinus infections in several studies. The TNF gene codes for tumor necrosis factor-alpha, which is a major player in the regulation of immune cells.
Chronic Sinus Infections Genotype Report
Members: Log in to see your data below.
Not a member? Join here.
Why is this section is now only for members? Here’s why…
Lifehacks: Natural solutions for chronic sinus infections
Neti pot or nasal irrigation:
Many studies show that nasal irrigation statistically improves chronic sinus infections. There are several ways to do sinus irrigation, including using a neti pot. Make sure to only use distilled water for your saline rinse.[ref][ref][ref]
Iodine rinse: One study found that a 0.08% diluted povidone-iodine solution reduced sinus infection symptoms in patients with ‘recalcitrant’ infections.[ref] Look for a package for sinus rinse or a prepared solution labeled for sinus infections. Povidone-iodine is also called betadine.
☑ Increase nitric oxide in your nose:
Related Articles and Genes:
Top 10 Genes to Check in Your Genetic Raw Data
Wondering what is actually important in your genetic data? These 10 genes have important variants with a big impact on health. Check your genes (free article).
Mast cells: MCAS, genetics, and solutions
Mast Cell Activation Syndrome, or MCAS, is a recently recognized disease involving mast cells misbehaving in various ways. Symptoms of MCAS can include abdominal pain, nausea, itching, flushing, hives, headaches, heart palpitations, anxiety, brain fog, and anaphylaxis.
Histamine Intolerance
Chronic headaches, sinus drainage, itchy hives, problems staying asleep, and heartburn — all these symptoms can be caused by the body not breaking down histamine very well. Your genetic variants could be causing you to be more sensitive to foods high in histamine. Check your genetic data to see if this could be at the root of your symptoms.
Genetics and Food Allergies
Do you have a food allergy? Discover how environmental factors and genetic susceptibility can shape individual reactions.
References:
Bernstein, Joel M., et al. “Genetic Polymorphisms in Chronic Hyperplastic Sinusitis with Nasal Polyposis.” The Laryngoscope, vol. 119, no. 7, July 2009, pp. 1258–64. PubMed, https://doi.org/10.1002/lary.20239.
Cardell, Lars Olaf. “The Paranasal Sinuses and a Unique Role in Airway Nitric Oxide Production?” American Journal of Respiratory and Critical Care Medicine, vol. 166, no. 2, July 2002, pp. 131–32. atsjournals.org (Atypon), https://doi.org/10.1164/rccm.2205014.
Carey, Ryan M., and Robert J. Lee. “Taste Receptors in Upper Airway Innate Immunity.” Nutrients, vol. 11, no. 9, Aug. 2019, p. 2017. PubMed Central, https://doi.org/10.3390/nu11092017.
Chang, Eugene H., et al. “Early Life Risk Factors for Chronic Sinusitis: A Longitudinal Birth Cohort Study.” The Journal of Allergy and Clinical Immunology, vol. 141, no. 4, Apr. 2018, pp. 1291-1297.e2. PubMed Central, https://doi.org/10.1016/j.jaci.2017.11.052.
Eby, George A. “Strong Humming for One Hour Daily to Terminate Chronic Rhinosinusitis in Four Days: A Case Report and Hypothesis for Action by Stimulation of Endogenous Nasal Nitric Oxide Production.” Medical Hypotheses, vol. 66, no. 4, 2006, pp. 851–54. PubMed, https://doi.org/10.1016/j.mehy.2005.11.035.
Erbek, Selim S., et al. “Proinflammatory Cytokine Single Nucleotide Polymorphisms in Nasal Polyposis.” Archives of Otolaryngology–Head & Neck Surgery, vol. 133, no. 7, July 2007, pp. 705–09. PubMed, https://doi.org/10.1001/archotol.133.7.705.
Hashemian, Farnaz, et al. “Effects of Vitamin D Supplementation on Recurrence of Nasal Polyposis after Endoscopic Sinus Surgery.” Iranian Journal of Otorhinolaryngology, vol. 32, no. 108, Jan. 2020, pp. 21–28. PubMed, https://doi.org/10.22038/ijorl.2019.37766.2241.
Hsu, Joy, et al. “Genetics of Chronic Rhinosinusitis: State of the Field and Directions Forward.” The Journal of Allergy and Clinical Immunology, vol. 131, no. 4, Apr. 2013, pp. 977-993.e5. PubMed Central, https://doi.org/10.1016/j.jaci.2013.01.028.
Kilty, Shaun J., et al. “Polymorphisms in the SERPINA1 (Alpha-1-Antitrypsin) Gene Are Associated with Severe Chronic Rhinosinusitis Unresponsive to Medical Therapy.” American Journal of Rhinology & Allergy, vol. 24, no. 1, Feb. 2010, pp. e4-9. PubMed, https://doi.org/10.2500/ajra.2010.24.3429.
Kłodzińska, Sylvia Natalie, et al. “Inhalable Antimicrobials for Treatment of Bacterial Biofilm-Associated Sinusitis in Cystic Fibrosis Patients: Challenges and Drug Delivery Approaches.” International Journal of Molecular Sciences, vol. 17, no. 10, Oct. 2016, p. 1688. PubMed Central, https://doi.org/10.3390/ijms17101688.
Kristjansson, Ragnar P., et al. “A Loss-of-Function Variant in ALOX15 Protects against Nasal Polyps and Chronic Rhinosinusitis.” Nature Genetics, vol. 51, no. 2, Feb. 2019, pp. 267–76. PubMed, https://doi.org/10.1038/s41588-018-0314-6.
Lee, Robert J., and Noam A. Cohen. “Role of the Bitter Taste Receptor T2R38 in Upper Respiratory Infection and Chronic Rhinosinusitis.” Current Opinion in Allergy and Clinical Immunology, vol. 15, no. 1, Feb. 2015, pp. 14–20. PubMed Central, https://doi.org/10.1097/ACI.0000000000000120.
Little, Paul, et al. “Effectiveness of Steam Inhalation and Nasal Irrigation for Chronic or Recurrent Sinus Symptoms in Primary Care: A Pragmatic Randomized Controlled Trial.” CMAJ : Canadian Medical Association Journal, vol. 188, no. 13, Sept. 2016, pp. 940–49. PubMed Central, https://doi.org/10.1503/cmaj.160362.
Mfuna Endam, Leandra, et al. “Genetic Variations in Taste Receptors Are Associated with Chronic Rhinosinusitis: A Replication Study.” International Forum of Allergy & Rhinology, vol. 4, no. 3, Mar. 2014, pp. 200–06. PubMed, https://doi.org/10.1002/alr.21275.
Panchmatia, Rikesh, et al. “The Efficacy of Diluted Topical Povidone-Iodine Rinses in the Management of Recalcitrant Chronic Rhinosinusitis: A Prospective Cohort Study.” European Archives of Oto-Rhino-Laryngology: Official Journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS): Affiliated with the German Society for Oto-Rhino-Laryngology – Head and Neck Surgery, vol. 276, no. 12, Dec. 2019, pp. 3373–81. PubMed, https://doi.org/10.1007/s00405-019-05628-w.
Payne, Spencer C., et al. “Genetics and Phenotyping in Chronic Sinusitis.” Journal of Allergy and Clinical Immunology, vol. 128, no. 4, Oct. 2011, pp. 710–20. ScienceDirect, https://doi.org/10.1016/j.jaci.2011.05.022.
Purnell, Phillip R., et al. “Single Nucleotide Polymorphisms in Chemosensory Pathway Genes GNB3, TAS2R19, and TAS2R38 Are Associated with Chronic Rhinosinusitis.” International Archives of Allergy and Immunology, vol. 180, no. 1, 2019, pp. 72–78. www.karger.com, https://doi.org/10.1159/000499875.
Rabago, David, et al. “Efficacy of Daily Hypertonic Saline Nasal Irrigation among Patients with Sinusitis: A Randomized Controlled Trial.” The Journal of Family Practice, vol. 51, no. 12, Dec. 2002, pp. 1049–55.
Risso, Davide S., et al. “Global Diversity in the TAS2R38 Bitter Taste Receptor: Revisiting a Classic Evolutionary PROPosal.” Scientific Reports, vol. 6, May 2016, p. 25506. PubMed Central, https://doi.org/10.1038/srep25506.
Weitzberg, Eddie, and Jon O. N. Lundberg. “Humming Greatly Increases Nasal Nitric Oxide.” American Journal of Respiratory and Critical Care Medicine, vol. 166, no. 2, July 2002, pp. 144–45. PubMed, https://doi.org/10.1164/rccm.200202-138BC.
Zhang, Yuan, et al. “Polymorphisms in the Nitric Oxide Synthase 1 Gene Are Associated with Severe Chronic Rhinosinusitis.” American Journal of Rhinology & Allergy, vol. 25, no. 2, Apr. 2011, pp. e49-54. PubMed, https://doi.org/10.2500/ajra.2011.25.3588.

