Key takeaways:
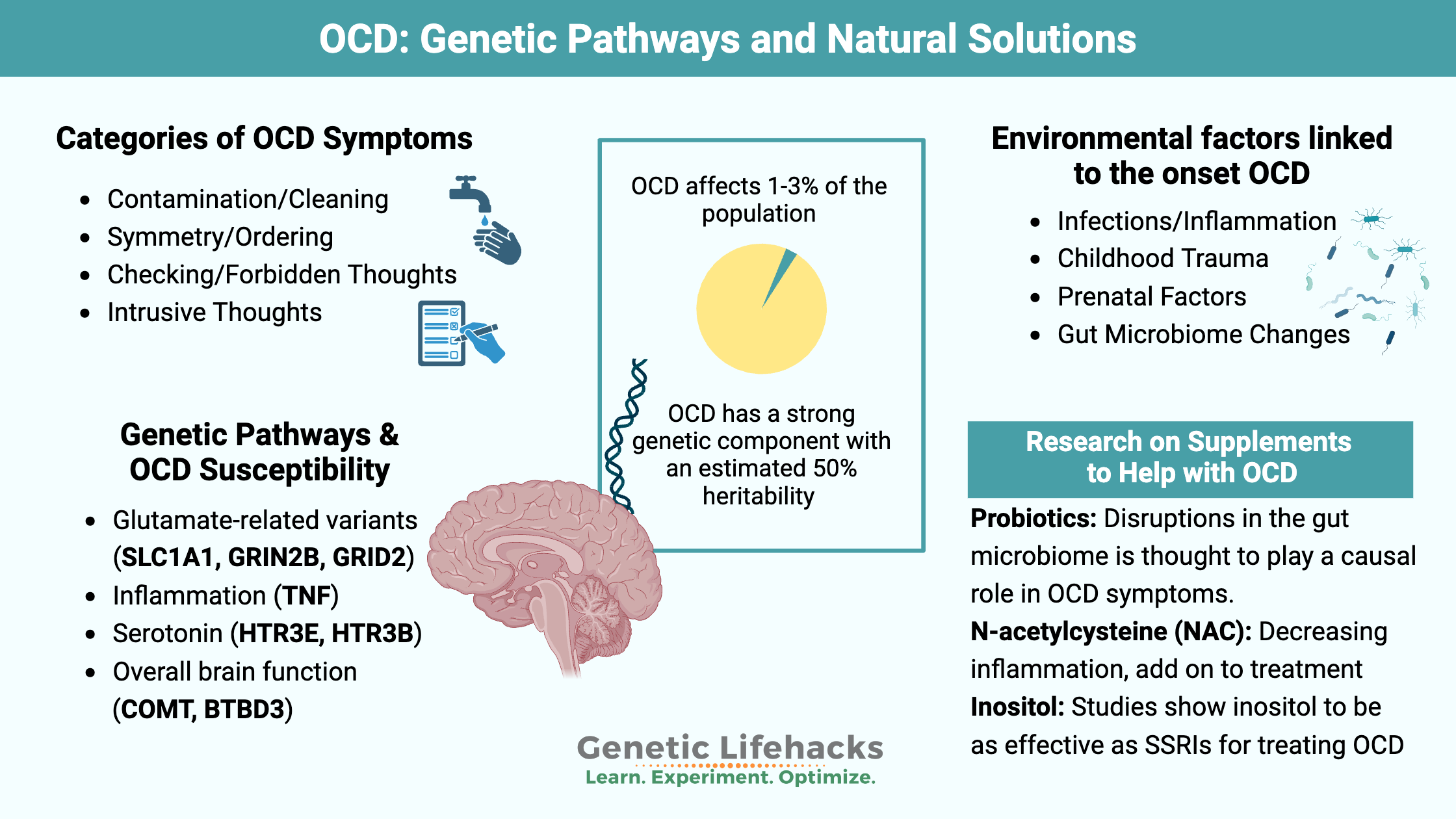
~ Obsessive-compulsive disorder is a psychiatric disorder that includes both genetic and environmental factors.
~ Alterations in glutamate, GABA, and other neurotransmitter levels are seen in specific brain regions in OCD.
~ Genetic variants in glutamate receptors, inflammatory cytokines, and serotonin pathways are linked to increased susceptibility to OCD.
What is OCD?
Obsessive-compulsive disorder (OCD) is considered a multi-symptom psychiatric disorder. It affects 2-3% of the population worldwide. Genetic studies show that it is strongly heritable, involving both common and rare genetic variants. Heritability studies in twins show that OCD is ~50% heritable with monozygotic twins having a concordance rate of 50-87%[ref][ref]
OCD often has an early onset in life, with about 50% of people now diagnosed in adolescence or childhood.[ref]
Symptoms of OCD:
Symptoms of OCD vary greatly from person to person, but generally consist of intrusive obsessions and then compulsions that are both distressing and time-consuming.[ref]
- Obsessions can be thoughts, urges, or mental images that are intrusive and associated with anxiety or distress. Common obsessions include worries about being a bad person, hurting others, or contaminating oneself.
- Compulsions are repetitive behaviors that relieve the stress or anxiety caused by the obsession. Examples include checking for safety, repetitive counting, ordering things, or frequent hand washing.
Obsession –> Worry or anxiety –> Compulsive action –> Relief from worry
As an example: An obsessive fear of contamination leads to ritual hand washing, which temporarily reduces the anxiety. [ref]
Four broad categories of OCD symptoms include:[ref]
- Contamination and cleaning
- Symmetry, repetition, organizing, and counting
- Checking and forbidden thoughts (sex, religion, aggression)
- General obtrusive thoughts
However, these general categories may not tell the whole story. There is now a spectrum of related disorders grouped with OCD, such as hoarding, skin picking, tics, and body dysmorphia.[ref]
Obsessive-compulsive disorder often overlaps genetically and functionally with other disorders, such as Tourette’s syndrome (tics), anorexia nervosa, bulimia, orthorexia, depression, schizophrenia, and autism spectrum disorder. One study found that 25% of schizophrenia patients also have OCD symptoms.[ref][ref][ref]
Related article: Schizophrenia genes
What happens in the brain in OCD?
Researchers and doctors are still trying to figure out exactly what happens in OCD. Brain imaging studies show that people with OCD have altered brain connectivity and activity in certain regions.[ref] Another study involving over 2,500 children with OCD symptoms found that they had a larger thalamus.[ref]
Let’s look at some of the known physiological changes in OCD.
GABA and glutamate balance:
Glutamate acts as an excitatory neurotransmitter for glutamatergic neurons. Glutamate levels, or more specifically the balance of glutamate in certain regions of the brain, are also thought to play a role in OCD.
Studies show that people with OCD are likely to have higher levels of glutamate in their cerebrospinal fluid (CSF).[ref] Other studies show lower levels of glutamate in the prefrontal cortex in people with OCD, showing that it is tissue-dependent alterations of glutamate rather than an overall increase or decrease.[ref]
GABA is the inhibitory neurotransmitter that keeps neurons from becoming overexcited, like the “off” switch for an excitatory neuron. GABA is synthesized from glutamate in the brain.
A recent study used new techniques to look at glutamate and GABA in the brains of people with OCD compared to healthy controls. They found that people with OCD had higher levels of glutamate and lower levels of GABA in the anterior cingulate cortex.[ref] The anterior cingulate cortex is the brain region that connects the frontal cortex to the thalamus and amygdala. It plays a role in motivation, cognition, emotion, decision-making, and impulse control.
A study of brain GABA levels using MRI found that levels in the prefrontal cortex were decreased in OCD patients.[ref]
It’s not as simple as too much glutamate and not enough GABA. Instead, the imbalances seem to be specific to different regions of the brain. For example, another study found lower glutamatergic (excitatory) gene expression in the orbitofrontal cortex and striatum in people with OCD.[ref]
Related articles: Glutatamate genes & GABA genes
Dopamine:
Dopamine modulates behavior and is involved in learning, memory, and reward. Animal studies suggest a role for the dopaminergic system in OCD-like behaviors. As a neurotransmitter, dopamine acts on dopamine receptors to send a signal from one neuron to the next.[ref]
Drugs that increase dopamine can cause OCD symptoms, such as in people taking dopaminergic drugs for Parkinson’s disease. In animal studies, dopamine receptor agonists (drugs that bind to the D2 receptor) can cause OCD-like behaviors.[ref] Overactivation of the D1 receptor has also been implicated in OCD in animals.[ref]
Serotonin:
The conventional treatment for OCD is serotonin reuptake inhibitors (antidepressants, SSRIs), suggesting either a role for serotonin in OCD or an alteration in the immune system. SSRIs increase serotonin levels in the brain and also affect the immune response in the brain. However, studies show that nearly two-thirds of people with OCD still have symptoms when treated with antidepressants.[ref][ref]
Related articles: Dopamine Synthesis & Dopamine Receptor Genes
Stress hormones and immune response:
Cortisol, a hormone released during stress, is elevated in people with OCD.[ref] Cortisol also modulates immune response, with high cortisol levels initially acting to suppress the immune system but long-term elevations leading to increased inflammation.
Related article: Cortisol and the HPA Axis
Neuroinflammation:
An autoimmune or inflammatory component is thought to underlie the onset of OCD for many people. In children, PANS (pediatric acute neuropsychiatric syndrome) is thought to be caused by strep A infection or other pathogens such as Mycoplasma pneumoniae, Borrelia burgdorferi, Borna disease virus, and Toxoplasmosis gondii.
Autoimmune causes of OCD are also possible, and covid infections are also being investigated. A study in Sweden found that people with OCD are at a 43% increased relative risk of other autoimmune disorders.[ref]
Inflammatory cytokine levels are often elevated in people with OCD. One study found that serum IL-1B and IL-6 levels were elevated compared to a control group.[ref] Another study in children found that cytokine levels (IL-1B, IL-6, and TNF-alpha) were predictive of the severity of symptoms.[ref][ref]
What triggers OCD to start?
OCD tends to start either in pre-adolescence (between the ages of 7 and 12) or in early adulthood (early 20s). However, the research on this is not completely clear because the age of diagnosis, such as in the early 20s, could include a childhood onset that is not diagnosed until early adulthood. Having routines or rituals is common and normal in children, as is collecting things and magical thinking. So determining when OCD began can be difficult, and it is often not formally diagnosed until adulthood, even if it began at an earlier age.[ref]
There are several known risk factors that precede the onset of OCD symptoms, including neuroinflammation, viral or bacterial infections, or other childhood trauma.
Infection, neuroinflammation, or trauma during childhood:[ref][ref][ref][ref]
- An autoimmune response to infection may lead to early-onset OCD. This is called pediatric autoimmune neuropsychiatric syndrome (PANS) – or PANDAS when referring specifically to a Strep A infection.
- Childhood stress is also a risk factor for OCD
- Some studies suggest a role for neuroinflammation.
- Influenza and hepatitis A vaccinations are associated with an increased risk of subsequent OCD diagnosis within the next 3-12 months.[ref][ref]
- People with OCD are more likely to have experienced childhood trauma.
Prenatal environment:
Maternal factors and the prenatal environment may also play a role in susceptibility. A recent study also showed that children with OCD or tics were more likely to have mothers with autoimmune diseases.[ref] Maternal illness during pregnancy and maternal smoking are also risk factors.[ref][ref]
Gut microbiome:
Both animal and human studies show that changes in the gut microbiome may be involved in OCD. For example, a 2020 study found that people with OCD have a reduced microbiome richness and lower abundance of butyrate-producing bacteria.[ref] Butyrate is a short-chain fatty acid that is produced by certain gut microbes and is important in the gut-brain axis. Butyrate has been shown in studies to act as an HDAC inhibitor, which is one way that gene expression is modified.[ref]
Genetics and OCD:
Researchers are looking at both common genetic variants that contribute to susceptibility to OCD, as well as rare mutations that significantly increase risk. Epigenetics and altered gene expression may also be involved.
Common variants:
Genetic variants related to glutamate, inflammation, and overall brain function have been associated with an increased relative risk of OCD. Interestingly, there is genetic overlap with comorbid conditions Tourette’s syndrome, schizophrenia, and anorexia nervosa.[ref][ref]
Rare variants:
In addition to the common variants that combine to increase risk, rare mutations have been found in some people with OCD. For example, de novo mutations in CHD8 are associated with altered synaptic transmission and neurogenesis. Again, there was genetic overlap with rare mutations and genes associated with Tourette syndrome and autism spectrum disorder. Copy number variants, which are insertions or deletions of multiple copies of nucleotide bases, are also commonly found in people with OCD.
[ref]
Protein expression:
Beyond traditional gene studies, researchers are also looking at how proteins are expressed differently in people with OCD. A study of overlapping genetic pathways found that OCD overlaps with olfactory transduction and herpes simplex virus 1 (HSV1) infection. There were also intersections with other neurological diseases, such as Huntington’s, Parkinson’s, and Alzheimer’s, with gene expression overlap related to the way mitochondria produce energy.[ref]
Genotype report for OCD
Below are common genetic variants that increase susceptibility to OCD. These variants do not cause OCD on their own but rather combine with other environmental factors.
Lifehacks:
Talk with your doctor about pharmaceutical options for OCD. Cognitive behavioral therapy, exposure response therapy, and NOCD are all options for OCD patients, and your doctor can help you navigate all of the options available.[ref][ref]
Sleep and Circadian Rhythm:
Circadian rhythm is your body’s natural 24-hour clock that controls fluctuations in hormones such as cortisol and the immune response. Melatonin is released at night in response to the absence of light, and melatonin is important both for reducing inflammation in the brain and for setting the circadian rhythm.
A study of people with obsessive-compulsive disorder showed that almost half of them had severely altered circadian rhythms with delayed melatonin onset. [ref] Another recent study also showed delayed circadian rhythm timing in people with OCD.[ref]
Avoiding electronics and light at night, especially blue light from screens, for two hours before bedtime can help get your circadian rhythm back on track. Exposure to sunlight in the morning can also help set the circadian rhythm and increase melatonin at night. [ref] While this may sound overly simplistic, the effects on the brain — cognitive function, thought patterns, mood — of circadian rhythm disruption are significant and real.
Diet and Nutrition:
The link between the gut microbiome and OCD, as well as the elevation of inflammatory cytokines, makes a healthy diet important. However, OCD symptoms may overlap with orthorexia and other eating disorders. Talk to your doctor or dietitian if you have questions about your diet.
In children and adults with Tourette syndrome or OCD, a gluten-free diet reduced symptoms in a portion of the study participants.[ref] Keep in mind that switching to a gluten-free diet often also decreases exposure to junk food and fast food.
The connection between low butyrate-producing bacteria and OCD points towards a diet higher in fiber and whole foods. However, I cannot find any research studies specifically looking at diet, the gut microbiome, and OCD. One book that may be worth reading on the role of diet and mental health is Brain Energy: A Revolutionary Breakthrough in Understanding Mental Health–and Improving Treatment for Anxiety, Depression, OCD, PTSD, and More by Chris Palmer.
Natural supplement with clinical trials for OCD:
Related articles:
HPA Axis Dysfunction: Understanding Cortisol and Genetic Interactions
Specialized Pro-resolving Mediators (SPMs): The Resolution of Inflammation