Key takeaways:
~ Low vitamin D levels are associated with an increased risk of chronic conditions, including mood disorders, cancer, and bone density issues.
~ Vitamin D regulates calcium uptake for bone health and influences the production of hundreds of enzymes, affecting overall wellness.
~ Genes play a big role in your body’s susceptibility to low vitamin D levels. Read on to learn how to check your 23andMe results for your vitamin D genes and find solutions tailored to your specific genetic variants.
Vitamin D: What does it do for you?
Vitamin D is essential to many processes in the body. It isn’t actually a vitamin at all, but a prohormone that is synthesized in the skin when exposed to UV radiation.
Low Vitamin D levels are linked to various chronic conditions, from mood disorders to cancer risk to immunity to bone density. In general, higher vitamin D levels correspond to a lower risk of getting a variety of chronic diseases.
People think of vitamin D regarding bone health because it regulates calcium uptake to keep bones strong. But there is a lot more to vitamin D and your health. It acts in your cells to regulate the production of hundreds of different enzymes, influencing wellness in a multitude of ways.
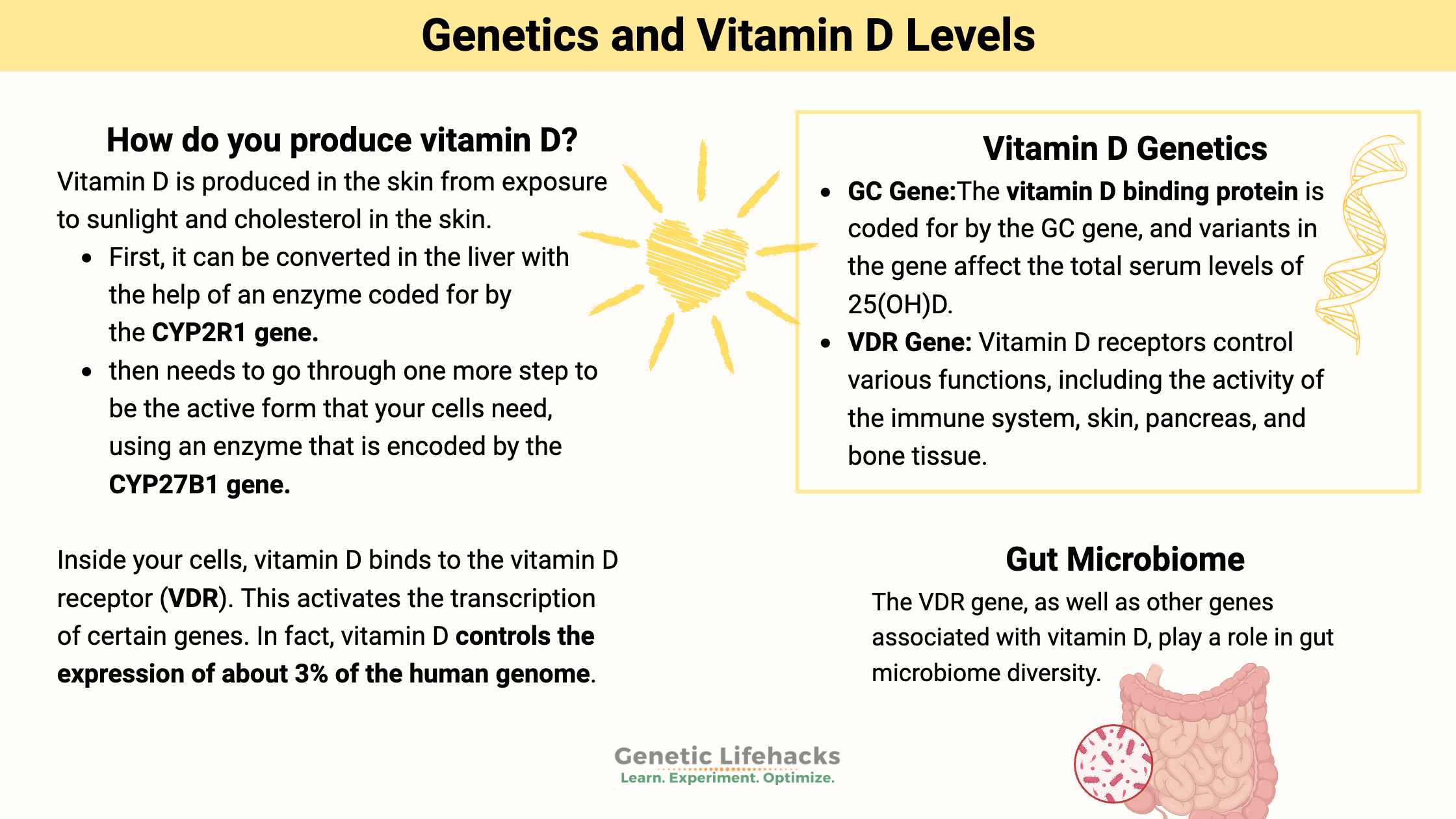
How do you produce vitamin D?
Vitamin D is produced in the skin from exposure to sunlight. It is produced via a reaction with UVB radiation and cholesterol in the skin.[ref]
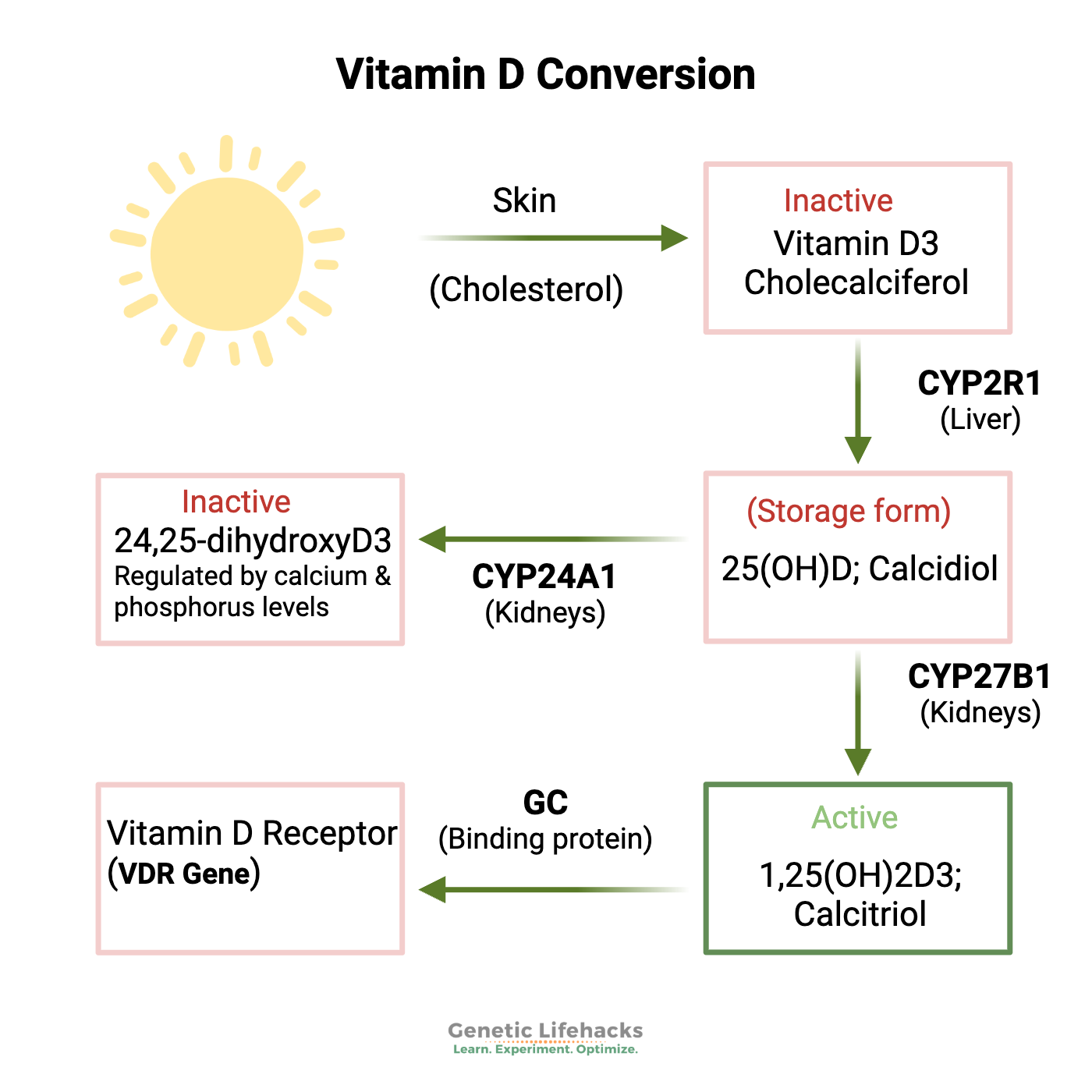
The initial form of vitamin D formed in the skin (or taken as a supplement) is the inactive form (cholecalciferol). It must go through several steps to convert into the active form.
- First, it can be converted in the liver into 25-hydroxy vitamin D – 25(OH)D – with the help of an enzyme coded for by the CYP2R1 gene.
- That 25(OH)D then needs to go through one more step to be the active form that your cells need. To convert the 25(OH)D into the active form – 1,25(OH)2D3 or calcitriol, cells use an enzyme that is encoded by the CYP27B1 gene.
Your body’s 25(OH)D levels depend on how much you take in from food and sunlight.
The 1,25(OH)2D3 (calcitriol) levels are more tightly regulated, and the active form is converted when and where it is needed within the cells.
What exactly does vitamin D do?
In a nutshell, vitamin D can cause cells to turn on genes, making certain proteins needed in a cell.
To get a little more specific…
Inside your cells, vitamin D binds to the vitamin D receptor (VDR). This then causes VDR to get together with a couple of other proteins (one is a vitamin A-related receptor) and bind to different spots on the nuclear DNA. This activates the transcription of certain genes. In fact, vitamin D controls the expression of about 3% of the human genome. So, yeah, it’s pretty important.
Additionally, vitamin D can act as a hormone within cells to immediately cause non-DNA-related actions to take place – such as opening ion channels or causing the secretion of insulin.
The term pleiotropy gets used a lot in research papers about vitamin D. Pleiotropy just means that one gene (or, in this case, one product of a gene, calcitriol) can cause more than one completely different action or trait to occur. In other words, vitamin D does a lot of stuff in the body that is seemingly unrelated. For example, Vitamin D is essential for calcium regulation and strong bones — and vitamin D is also essential for immune response. It is also important in cancer prevention, hypertension, atrial fibrillation, blood clots, inflammatory bowel disease, and autoimmune disease. [ref]
For Vitamin D to be used in the nucleus of cells, it needs to be transported there by a binding protein coded for by the GC gene, and then it needs to bind to the vitamin D receptor, which is coded for by the VDR gene.
Does supplementing with vitamin D actually do anything?
While low levels of vitamin D have been associated with a higher risk of a bunch of chronic conditions, supplementing with vitamin D doesn’t always give impressive results in placebo-controlled studies. For example, a recent clinical trial found little benefit for postmenopausal women when looking at bone mineral density. On the other hand, the amount of vitamin D used in the trial may have been too small to get a result.[ref]
One reason that some of the research studies and clinical trials of vitamin D supplementation showed no positive results is that the doses used may have been too low.
A study came out a couple of years ago claiming there was a statistical error in the calculation for the recommended daily vitamin D intake.[ref] This error changed the supplemental doses needed by a factor of 10. Instead of 600 IU, some people may need 6,000IU+ per day. Other recent studies have backed this up, showing also that a person’s weight plays a big role in the amount of vitamin D needed for sufficiency.
A recent meta-analysis combining data from 52 different trials found that vitamin D supplementation did not impact overall mortality rates, but it did decrease the risk of death from cancer.
Vitamin D Genotype Report:
Genetics can play a role in vitamin D levels in several ways, which makes sense when looking at the different steps involved in converting it to the active form, which then acts on the vitamin D receptors in a cell.
Below are genetic variants that have been shown in multiple research studies to impact vitamin D levels.
Lifehacks:
Circadian Rhythm, Melatonin, and preventing damage from sun exposure:
Our skin naturally makes vitamin D through exposure to the sun. However, sun exposure seems to be a double-edged sword these days, with UV light giving us vitamin D as well as increasing our risk for cancer. It makes you wonder why all of our ancestors didn’t end up with skin cancer without a handy bottle of sunscreen available.
Turns out that our modern lifestyle with light at night (TVs, tablets, phones, and LED light bulbs) has decreased our melatonin production. Melatonin at the right time plays a big role in both our circadian rhythm and our skin’s natural ability to withstand UV rays without creating skin cancer. Blocking blue light wavelengths at night increases melatonin production and should increase our skin’s ability to utilize UV rays for vitamin D production without harmful effects.[ref] Read more about melatonin production, genetics, and blue light.
In addition to light at night, the time at which you eat also influences the circadian rhythm of your genes. A recent study showed mice eating at the wrong time (equivalent to humans eating at night) had increased skin damage from UV light.[ref] Basically, eating at the wrong time shifted the phase of the circadian rhythm of skin genes to where UV damage would be less of a problem at night rather than during the day… and the sun doesn’t shine at night! So an easy ‘lifehack’ here would be to eat dinner earlier in the evening and don’t snack at night.
Food and Supplements for increasing vitamin D:
Related Articles and Topics:
Circadian Rhythms: Genes at the Core of Our Internal Clocks
Circadian rhythms are the natural biological rhythms that shape our biology. Our master ‘clock’ genes drive this. It turns out that we also have circadian cycles (peripheral clocks) in most organs, such as the liver, pancreas, and fat cells.
Melatonin: Key to Health and Longevity
More than just a sleep hormone, melatonin is at the heart of many health topics. Your genetic variants play a big role in the production of melatonin. Learn how your lifestyle and diet interact with your melatonin-related genes.
Leveraging your gut microbiome to change your gene expression
Learn how your gut microbiome influences the expression of your core circadian rhythm genes.
References:
Ahn, Jiyoung, Kai Yu, et al. “Genome-Wide Association Study of Circulating Vitamin D Levels.” Human Molecular Genetics, vol. 19, no. 13, July 2010, pp. 2739–45. PubMed Central, https://doi.org/10.1093/hmg/ddq155.
Ahn, Jiyoung, Demetrius Albanes, et al. “Vitamin D-Related Genes, Serum Vitamin D Concentrations and Prostate Cancer Risk.” Carcinogenesis, vol. 30, no. 5, May 2009, pp. 769–76. PubMed Central, https://doi.org/10.1093/carcin/bgp055.
Alagarasu, K., et al. “Association of Vitamin D Receptor Gene Polymorphisms with Clinical Outcomes of Dengue Virus Infection.” Human Immunology, vol. 73, no. 11, Nov. 2012, pp. 1194–99. PubMed, https://doi.org/10.1016/j.humimm.2012.08.007.
Atoum, Manar Fayiz, and Melya Nizar Tchoporyan. “Association between Circulating Vitamin D, the Taq1 Vitamin D Receptor Gene Polymorphism and Colorectal Cancer Risk among Jordanians.” Asian Pacific Journal of Cancer Prevention: APJCP, vol. 15, no. 17, 2014, pp. 7337–41. PubMed, https://doi.org/10.7314/apjcp.2014.15.17.7337.
Bouillon, Roger, et al. “Vitamin D and Human Health: Lessons from Vitamin D Receptor Null Mice.” Endocrine Reviews, vol. 29, no. 6, Oct. 2008, pp. 726–76. PubMed, https://doi.org/10.1210/er.2008-0004.
Desotelle, Joshua A., et al. “The Circadian Control of Skin and Cutaneous Photodamage.” Photochemistry and Photobiology, vol. 88, no. 5, Sept. 2012, pp. 1037–47. PubMed Central, https://doi.org/10.1111/j.1751-1097.2012.01099.x.
Gaffney-Stomberg, Erin, et al. “Association Between Single Gene Polymorphisms and Bone Biomarkers and Response to Calcium and Vitamin D Supplementation in Young Adults Undergoing Military Training.” Journal of Bone and Mineral Research: The Official Journal of the American Society for Bone and Mineral Research, vol. 32, no. 3, Mar. 2017, pp. 498–507. PubMed, https://doi.org/10.1002/jbmr.3008.
Ganz, Ariel B., et al. “Vitamin D Binding Protein Rs7041 Genotype Alters Vitamin D Metabolism in Pregnant Women.” FASEB Journal: Official Publication of the Federation of American Societies for Experimental Biology, vol. 32, no. 4, Apr. 2018, pp. 2012–20. PubMed, https://doi.org/10.1096/fj.201700992R.
Grant, William B., et al. “Evidence That Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths.” Nutrients, vol. 12, no. 4, Apr. 2020, p. 988. PubMed Central, https://doi.org/10.3390/nu12040988.
Hansen, Karen E., et al. “Treatment of Vitamin D Insufficiency in Postmenopausal Women: A Randomized Clinical Trial.” JAMA Internal Medicine, vol. 175, no. 10, Oct. 2015, pp. 1612–21. PubMed, https://doi.org/10.1001/jamainternmed.2015.3874.
McGrath, John J., et al. “A Systematic Review of the Association between Common Single Nucleotide Polymorphisms and 25-Hydroxyvitamin D Concentrations.” The Journal of Steroid Biochemistry and Molecular Biology, vol. 121, no. 1–2, July 2010, pp. 471–77. PubMed, https://doi.org/10.1016/j.jsbmb.2010.03.073.
Moffett, Susan P., et al. “Association of the VDR Translation Start Site Polymorphism and Fracture Risk in Older Women.” Journal of Bone and Mineral Research: The Official Journal of the American Society for Bone and Mineral Research, vol. 22, no. 5, May 2007, pp. 730–36. PubMed, https://doi.org/10.1359/jbmr.070201.
Petersen, Rikke A., et al. “Common Genetic Variants Are Associated with Lower Serum 25-Hydroxyvitamin D Concentrations across the Year among Children at Northern Latitudes.” The British Journal of Nutrition, vol. 117, no. 6, Mar. 2017, pp. 829–38. PubMed, https://doi.org/10.1017/S0007114517000538.
Robien, Kim, et al. “Genetic and Environmental Predictors of Serum 25-Hydroxyvitamin D Concentrations among Middle-Aged and Elderly Chinese in Singapore.” The British Journal of Nutrition, vol. 109, no. 3, Feb. 2013, pp. 493–502. PubMed, https://doi.org/10.1017/S0007114512001675.
Sadat-Ali, Mir, et al. “Genetic Influence on Circulating Vitamin D among Saudi Arabians.” Saudi Medical Journal, vol. 37, no. 9, Sept. 2016, pp. 996–1001. PubMed, https://doi.org/10.15537/smj.2016.9.14700.
Sollid, Stina T., et al. “Effects of Vitamin D Binding Protein Phenotypes and Vitamin D Supplementation on Serum Total 25(OH)D and Directly Measured Free 25(OH)D.” European Journal of Endocrinology, vol. 174, no. 4, Apr. 2016, pp. 445–52. PubMed Central, https://doi.org/10.1530/EJE-15-1089.
Suaini, Noor H. A., et al. “Environmental and Genetic Determinants of Vitamin D Insufficiency in 12-Month-Old Infants.” The Journal of Steroid Biochemistry and Molecular Biology, vol. 144 Pt B, Oct. 2014, pp. 445–54. PubMed, https://doi.org/10.1016/j.jsbmb.2014.08.018.
Trummer, Olivia, et al. “Genetic Components of 25-Hydroxyvitamin D Increase in Three Randomized Controlled Trials.” Journal of Clinical Medicine, vol. 9, no. 2, Feb. 2020, p. 570. PubMed Central, https://doi.org/10.3390/jcm9020570.
VCV000001661.2 – ClinVar – NCBI. https://www.ncbi.nlm.nih.gov/clinvar/variation/1661/. Accessed 4 Oct. 2022.
Veugelers, Paul J., and John Paul Ekwaru. “A Statistical Error in the Estimation of the Recommended Dietary Allowance for Vitamin D.” Nutrients, vol. 6, no. 10, Oct. 2014, pp. 4472–75. PubMed Central, https://doi.org/10.3390/nu6104472.
Vitamin D Receptor Gene FokI Polymorphism Contributes to Increasing the Risk of Tuberculosis: Evidence from a Meta-Analysis. 12 Aug. 2021, https://doi.org/10.21203/rs.3.rs-774522/v1.
Wang, Hong, et al. “Time-Restricted Feeding Shifts the Skin Circadian Clock and Alters UVB-Induced DNA Damage.” Cell Reports, vol. 20, no. 5, Aug. 2017, pp. 1061–72. PubMed Central, https://doi.org/10.1016/j.celrep.2017.07.022.
Wang, Jun, et al. “Genome-Wide Association Analysis Identifies Variation in Vitamin D Receptor and Other Host Factors Influencing the Gut Microbiota.” Nature Genetics, vol. 48, no. 11, Nov. 2016, pp. 1396–406. PubMed Central, https://doi.org/10.1038/ng.3695.
Wang, Thomas J., et al. “Common Genetic Determinants of Vitamin D Insufficiency: A Genome-Wide Association Study.” The Lancet, vol. 376, no. 9736, July 2010, pp. 180–88. DOI.org (Crossref), https://doi.org/10.1016/S0140-6736(10)60588-0.