Key takeaways:
~BPA and its alternatives, BPS and BPF, are pervasive in daily life, found in plastics, food containers, receipts, and even dust.
~ Research shows BPA and similar bisphenols disrupt hormones, increase inflammation, and impact health conditions such as obesity, insulin resistance, and male fertility.
~ Genetic variants influence how well you detoxify BPA, leaving some people more at risk than others.
~ Reduce BPA exposure by avoiding specific sources like plastic containers and thermal receipts, while specific supplements and detox methods like sweating and probiotics may help with excretion.
BPA and BPS: Ubiquitous Exposure to Plastics
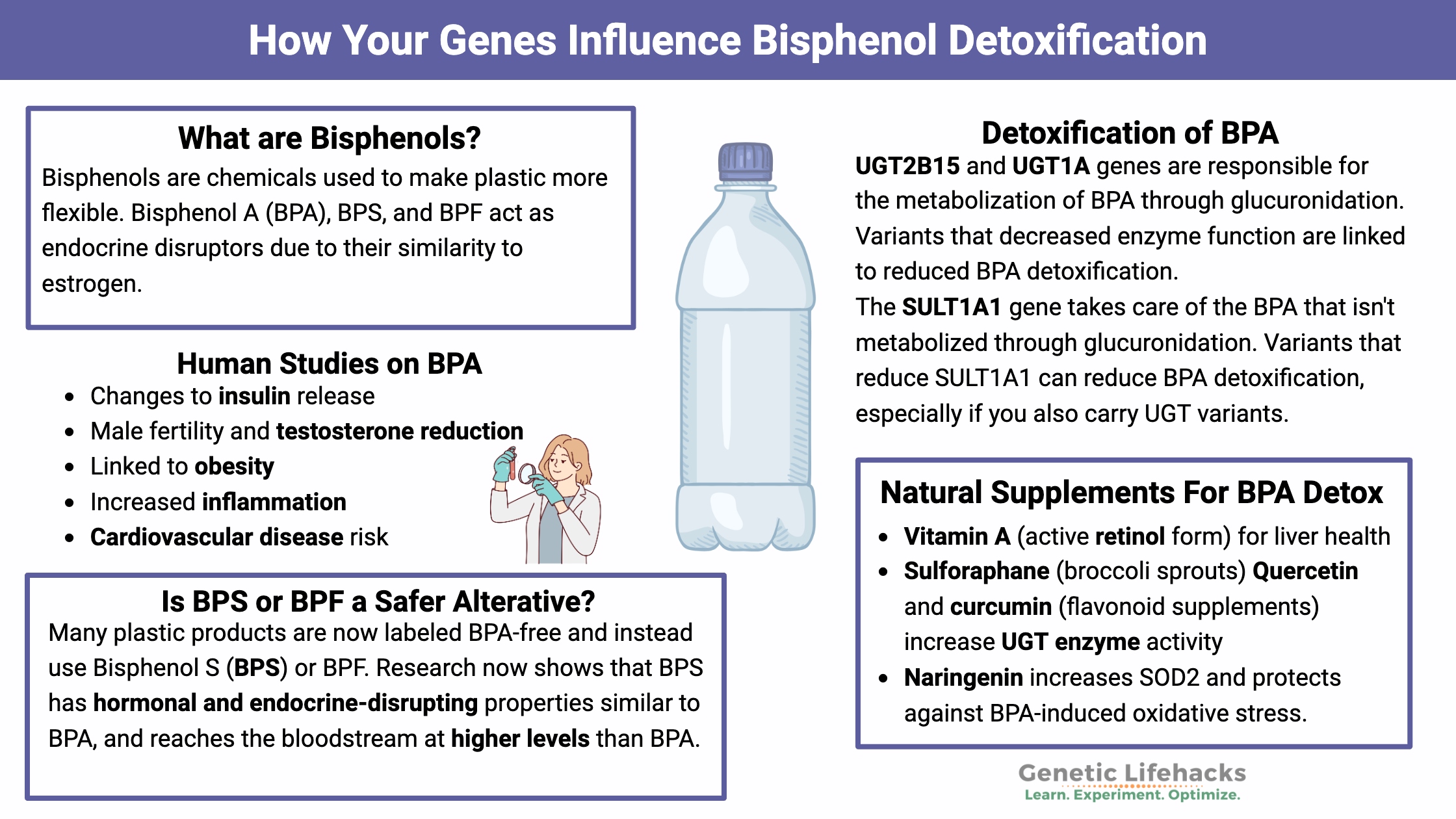
Bisphenols are chemicals used to make plastic more flexible. Bisphenol A (BPA), BPS, and BPF act as endocrine disruptors and have been linked in human studies to obesity, insulin resistance, and altered gene expression.
BPA is everywhere in our food supply. In fact, a CDC report showed that 93% of people have BPA in their urine.[ref] This article explains the peer-reviewed research and the links to genetic variants involved in getting rid of BPA.
What is BPA?
- Bisphenol-A is a component of some types of plastic.
- It is considered to be an endocrine disruptor because of the similarity of the molecules to estrogen.
- It is now ubiquitous in the environment, and >90% of people have detectable levels in their blood.
What is BPS? BPF?
With scary headlines about BPA, many companies have opted to make BPA-free plastics using Bisphenol S (BPS) or Bisphenol F (BPF). Some countries have banned BPA in food contact wrappers and baby products, but BPS or other bisphenol alternatives are allowed.
Research now shows that BPS and BPF have hormonal and endocrine-disrupting properties similar to BPA.[ref]
Recent animal studies show that BPS is actually absorbed better and reaches the bloodstream at higher levels than BPA. The oral bioavailability of BPS is about 50% higher than BPA, and it persists for a longer time in the body. Studies on BPF, another bisphenol alternative, show that it alters insulin response and has an obesogenic effect.[ref]
Bisphenol AF (BPAF) is a fluorinated analog of BPA. It is increasingly being used in food wrappers and thermal receipt paper as an alternative to BPA, since it does not have the same endocrine hormone-mimicking effects.[ref] However, BPAF has been shown in studies to cause chromosomal damage.[ref]
How are we exposed to BPA, BPS, and other bisphenols:
While we often think of BPA as something to avoid in plastic water bottles, our routes of exposure are much greater than just in plastic containers.
For example, BPA and bisphenols can be found in:[ref]
| Source Type | Examples/Details |
|---|---|
| Plastics | Bottles, food containers, utensils, kitchenware[ref] |
| Food Packaging | Can linings, wrappers, paper plates, cardboard boxes[ref][ref] |
| Receipts | Thermal printed receipts (BPA, BPS, BPAF)[ref][ref], |
| Clothing/Fabrics | Pantyhose, polyester fabrics, infant clothing, socks[ref] |
| Dental Materials | Composite resins, sealants, braces bonding brackets[ref][ref] |
| Household Dust | From breakdown of plastics, polyester, furniture |
| Beverages | Hot drinks in to-go cups lined with plastic[ref] |
| Miscellaneous | Microplastics, soil contamination[ref][ref][ref] |
How much?
A recent study examined reference levels, animal studies, and autoimmune studies. The results showed that the majority of people are exposed to BPA in food at a level that is more than two orders of magnitude over the European tolerable daily intake (TDI).[ref]
Exposure starts before birth:
Another recent study looked at BPA and PFOAs in over 6,000 newborns to determine if there was an effect on birth size. Researchers found that over 90% of the infants had detectable levels of BPA in their blood, and over 99% had detectable PFOA and PFOS. The study did find that average BPA levels were higher in twins born with lower birth weight, possibly because higher BPA levels also correlated with a greater number being born before 37 weeks of age.[ref]
As BPA has been replaced by BPS and BPF (so that manufacturers can slap a BPA-free label on), a 2022 study showed that 80-90% of children had BPS in their bodies.
What do human studies show about Bisphenols?
Animal studies clearly show that BPA can cause weight gain, alter hormone levels, disrupt reproduction, affect offspring, etc.[ref] Importantly, animal studies clearly show that low-level exposure, similar to what most of us encounter daily, is what drives the negative metabolic impacts. Exposure to high levels of BPA is actually less harmful than chronic, low-level exposure.[ref]
With more BPS and BPF replacing BPA in products, research now shows that these replacements have similar (or stronger) health effects including acting as an endocrine disruptor and promoting fat accumulation in adipocytes.[ref]
While animal studies are important, I’m going to focus here on recent human studies that take into account current human levels of exposure.
| Health Effect | Bisphenol(s) Involved | Study Highlights/Notes |
|---|---|---|
| Hormone Disruption | BPA, BPS, BPF | Endocrine disruptors, estrogen-mimicking |
| Obesity/Weight Gain | BPA, BPS, BPF | Increased risk, especially in children/teens |
| Insulin Resistance/Diabetes | BPA, BPS, BPF | Increased risk, altered insulin response |
| Male Fertility | BPA | Reduced sperm motility, lower testosterone |
| Inflammation | BPA, BPS, BPF | Chronic low-level inflammation, increased cytokines |
| Cardiovascular Disease | BPA | Increased risk via NPY activation, myocarditis |
| DNA/Chromosomal Damage | BPAF | Chromosomal breaks in cell lines |
| Altered Lipid Profile | BPA, BPS, BPF | In newborns from exposed mothers |
| Gene Expression Changes | BPA, BPS, BPF | Altered miRNA, changes linked to blood pressure |
Metabolic changes and insulin resistance:
A study published in the Journal of the Endocrine Society looked at the effect of BPA on insulin secretion and glucose levels. The researchers gave an oral dose of BPA at 50 ug/kg body weight, which is the daily limit set by the EPA as being safe daily exposure over a lifetime. They found that this BPA dose increased initial insulin release (oral glucose tolerance) but then showed no statistical difference with the later phase blood glucose response. This is an important study because they used the EPA guidelines for an amount of BPA that was not supposed to elicit a response.[ref] I found it interesting that there was a large variation between individuals in their BPA levels over time after ingestion — individual rates of BPA metabolism varied a lot!
Related article: Genetic risk factors for insulin resistance
BPS and BPF are also strongly associated with an increased risk of diabetes. For example, a French study followed 775 non-diabetic adults for nine years while measuring BPS levels. At year three, the group with the top 50% of BPS urinary levels had double the rate of diabetes.[ref] Korean and Chinese studies show similar results for BPS and BPF exposure and the risk of type 2 diabetes.[ref]
Related article: Genetic risk factors for type 2 diabetes
Bisphenols are strongly linked to weight gain:
A study published in 2018 found that children and teens with higher BPA exposure (the top third of the group) had a 12-fold increased risk of obesity.[ref] This is just one example from a long line of human studies that showed that higher BPA and BPS exposure increases weight and waist circumference.[ref][ref][ref][ref][ref][ref][ref][ref]
In addition to the effect on testosterone and abdominal weight gain, BPA stimulates the overexpression of GPR30 in fat cells, which prevents the burning of the fat for energy.[ref]
Male fertility and testosterone reduction:
BPA was shown in a recent study (and several previous studies) to reduce sperm motility in men.[ref] Previous studies also showed decreased testosterone levels in male teenagers with higher levels of BPA.[ref] Other research shows that BPA disrupts the activation of androgens, leading to reduced testosterone and increased belly fat.[ref]
Related article: Male infertility genetic variants
Chronic, low-level inflammation:
A study from August 2018 found that BPA at normal exposure levels alters insulin response in a way that is independent of adipogenesis (fat creation). The study found that BPA causes a low-level inflammatory response.[ref] This is in line with previous epidemiological studies that tie higher BPA levels to insulin resistance in men, women, and children.[ref][ref][ref] Animal studies on BPS and BPF also show increased inflammatory cytokine levels, including TNF-alpha.[ref]
Related article: TNF-alpha, chronic inflammation
Myocarditis and cardiovascular disease:
Estrogen receptors are located in mast cells and cardiac muscle cells in the heart. A 2019 study in mice found that exposure to BPA in their drinking water increased their susceptibility to viral myocarditis and pericarditis. The higher BPA levels also activate mast cells in the heart.[ref] Additionally, activation of neuropeptide Y (NPY) by BPA not only increases obesity but also contributes to the pathogenesis of heart disease.[ref]
Altered lipid profile in babies:
A study of maternal BPA, BPS, and BPF levels showed that babies born to mothers with higher bisphenol levels had altered fatty acid profiles.[ref]
Chromosomal / DNA breaks with BPAF:
A recent study showed that bisphenol AF (BPAF), which is a fluorinated BPA, can cause chromosomal or DNA breaks in human cell lines. This is concerning because DNA breaks cause mutations that can lead to cancer. The study was in cell lines (not in living humans) and showed that at certain concentrations, BPAF and possibly BPA/BPS can cause chromosomal damage.[ref] BPAF is a newer bisphenol that was developed for food wrappers and can linings because it doesn’t have the same hormonal effects.
Bisphenols alter gene expression:
Recent research shows that exposure to low levels of bisphenols alters microRNA expression. MicroRNAs (miRNAs) are short RNA strands that can block genes from being translated into their protein. There are a few thousand miRNAs that each can control the expression of multiple genes.
A recent experiment involved exposing women over the age of 60 to BPA at different doses. The researchers then measured the BPA levels in their urine and blood and found that certain miRNAs were increased while others were decreased. Interestingly, the six miRNAs that were altered were related to blood pressure, which may be why BPA is associated with hypertension.[ref]
Related article: MicroRNAs
In boys with autism spectrum disorder, a study linked higher maternal BPA levels with an increased risk of autism in boys at age 2 and at age 9. The link was demonstrated to be due to impaired aromatase function due to higher methylation of the CYP19A1 gene from in utero exposure to BPA. In the study, the researchers looked at five CYP19A1 to create a ‘high’ or ‘low’ CYP19A1 score for the boys. Those with a low CYP19A1 score – combined with higher maternal BPA levels – were at a 3 to 6-fold increased risk of ASD diagnosis.[ref]
How are bisphenols eliminated from the body?
Most of the bisphenols that are absorbed from food or taken in through the skin will end up in the liver where a process called glucuronidation will modify the BPA so that it can be easily excreted. Liver health is important in detoxifying many environmental toxicants, including bisphenols.
Glucuronidation is a phase II detoxification process that adds glucuronic acid to a substance, such as bisphenols, for easy elimination.
The UGT (UDP-glucuronosyltransferase) enzymes facilitate a glucuronidation reaction. Glucuronidation involves the attachment of a glucuronic acid molecule to a toxicant or drug metabolite. Glucuronic acid is a metabolite of glucose and is abundant in the body. Variants in the UGT genes can affect the metabolism of bisphenols.
Related article: UGT genes
The glucuronidated bisphenol is then exported from the cell by efflux transporters. MDR3 (Multidrug resistance protein 3) is the primary efflux transporter for removing the bisphenol metabolites from the cell. The ABCB4 gene encodes MDR3.[ref]
The rate at which bisphenols are metabolized and eliminated from the body is important in understanding the risk of negative effects. For example, women with a UGT2B15 variant had both higher unmetabolized BPA levels and an almost 2-fold risk of PCOS.[ref]
Genotype Report: Bisphenol Detoxification
The studies show that, on average, exposure to BPA, BPS, and BPF at low levels is detrimental to metabolic health and possibly reproductive health. However, not everyone is affected by BPA and BPS in the same way. Genetic variants impact how quickly you clear it out of your body and how likely it is to be a problem for you.
This genotype report is broken up into sections:
- Variants related to oxidative stress response related to bisphenol exposure
- Variants related to the process of breaking down and eliminating bisphenols
- Variants related to the risk of cancer from the estrogen-mimic effect of bisphenols
Genetic Variants Related to BPA and Oxidative Stress:
Bisphenol exposure increases oxidative stress and mitochondrial dysfunction. A study that looked at BPA exposure in children with autism found that all children (with and without autism) had an increase in oxidative stress and mitochondrial dysfunction when exposed to BPA.[ref] Another study found increased oxidative stress biomarkers in pregnant women based on BPA exposure.[ref]
Genetic variants that decrease your response to oxidative stress have been shown to interact with BPA exposure to cause liver problems. While most people with these variants won’t have severe liver problems from bisphenol exposure, these genetic variants indicate that you could be more affected by continual bisphenol exposure – especially if combined with another toxicant that puts a strain on the liver.
Lifehacks for getting rid of bisphenols:
Getting rid of BPA and BPS involves lifestyle changes for reducing exposure as well as detoxification methods to eliminate it from the body.
Lifestyle changes:
Stopping exposure to BPA is the logical first step; it is also the hardest. Realistically, it isn’t possible to cut out all exposure.
Prioritize and choose the areas where you will get the most impact.
Avoid common sources of BPA and BPS:
- plastic bottles, plastic food containers
- teabags that contain plastic[ref]
- thermal printed receipts (now more BPS than BPA)[ref][ref], especially when combined with hand sanitizer[ref]
- composite dental resins and sealants[ref]
- brackets for bonding braces[ref]
- most food – from plastic containers or from the soil[ref][ref]
- hot beverages, such as coffee, from plastic or disposable cups[ref]
- clothing (82% of infant clothing tested had BPA)[ref];
- polyester fabrics, athletic clothing, and socks are big sources of transdermal BPA[ref]
- cans lined with BPA or other alternative bisphenols
- plastic kitchenware such as utensils, plastic cups, and plastic containers
- takeout drinks and plastic takeout containers[ref]
Make consistent changes where you can:
A study involving eating canned food vs. fresh food showed that BPA levels were more than doubled with canned food consumption. Of note, the BPA levels returned to normal after 24 hours.[ref]
Making choices to eat fresh foods instead of canned foods can have a quick impact on your BPA levels. Many makers of canned foods have moved away from using BPA in the can linings, and you’ll often see BPA-free on the label. However, the new linings may use other bisphenols, polyester, or polyvinyl chloride. Of note, tetramethyl bisphenol F (TMBPF) has been developed as an alternative for lining food cans. Studies show that it does not have the endocrine-disrupting effects of BPA and doesn’t make people fat. However, it does have a toxic effect on stem cells.[ref]
Another study looked at the bisphenol levels of people eating foods wrapped in plastic, along with some canned foods, in comparison to people eating fresh foods that weren’t plastic-wrapped. Switching to fresh foods not wrapped in plastic dropped bisphenol levels by 66% within three days.[ref]
A 3-day dietary intervention study showed that eliminating foods in plastic containers, fast foods, and delivery foods dropped BPS and BPA levels by more than 50%.[ref]
The takeaway here is that you can cut your exposure to bisphenol quickly and significantly by preparing fresh food that hasn’t been stored in plastic, including cans lined with bisphenols and cardboard containers lined with bisphenols.
Dust your house:
Our polyester clothes, furniture, and plastic items throughout the house break down and contribute bisphenols to the household dust. One estimate showed that household dust contributed to about 10% of our daily BPA exposure.[ref] Regularly dusting with a damp cloth, vacuuming with a HEPA filter vacuum, and keeping dryer lint from lingering in the laundry area will all help make a difference.
Sauna, exposure to heat:
Related Articles and Topics:
Glutathione: Master Antioxidant, Reducing Oxidative Stress, and Detoxification
References
Alharbi, Hend F., et al. “Exposure to Bisphenol A Substitutes, Bisphenol S and Bisphenol F, and Its Association with Developing Obesity and Diabetes Mellitus: A Narrative Review.” International Journal of Environmental Research and Public Health, vol. 19, no. 23, Nov. 2022, p. 15918. PubMed Central, https://doi.org/10.3390/ijerph192315918.
Amin, Mohammad Mehdi, et al. “Association of Exposure to Bisphenol A with Obesity and Cardiometabolic Risk Factors in Children and Adolescents.” International Journal of Environmental Health Research, vol. 29, no. 1, Feb. 2019, pp. 94–106. PubMed, https://doi.org/10.1080/09603123.2018.1515896.
Ariemma, Fabiana, et al. “Low-Dose Bisphenol-A Impairs Adipogenesis and Generates Dysfunctional 3T3-L1 Adipocytes.” PloS One, vol. 11, no. 3, 2016, p. e0150762. PubMed, https://doi.org/10.1371/journal.pone.0150762.
Bell, Erin M., et al. “Concentrations of Endocrine Disrupting Chemicals in Newborn Blood Spots and Infant Outcomes in the Upstate KIDS Study.” Environment International, vol. 121, no. Pt 1, Dec. 2018, pp. 232–39. PubMed, https://doi.org/10.1016/j.envint.2018.09.005.
Blaauwendraad, Sophia M., et al. “Associations of Maternal Bisphenol Urine Concentrations during Pregnancy with Neonatal Metabolomic Profiles.” Metabolomics, vol. 17, no. 9, 2021, p. 84. PubMed Central, https://doi.org/10.1007/s11306-021-01836-w.
Bruno, Katelyn Ann, et al. “BPA Alters Estrogen Receptor Expression in the Heart After Viral Infection Activating Cardiac Mast Cells and T Cells Leading to Perimyocarditis and Fibrosis.” Frontiers in Endocrinology, vol. 10, Sept. 2019, p. 598. PubMed Central, https://doi.org/10.3389/fendo.2019.00598.
Calafat, Antonia M., et al. “Exposure of the U.S. Population to Bisphenol A and 4-Tertiary-Octylphenol: 2003–2004.” Environmental Health Perspectives, vol. 116, no. 1, Jan. 2008, pp. 39–44. PubMed Central, https://doi.org/10.1289/ehp.10753.
De Filippis, Elena, et al. “Exposure of Adipocytes to Bisphenol-A in Vitro Interferes with Insulin Action without Enhancing Adipogenesis.” PLoS ONE, vol. 13, no. 8, Aug. 2018, p. e0201122. PubMed Central, https://doi.org/10.1371/journal.pone.0201122.
Di Bella, Giuseppa, et al. “Plasticizers and BPA Residues in Tunisian and Italian Culinary Herbs and Spices.” Journal of Food Science, vol. 83, no. 6, June 2018, pp. 1769–74. PubMed, https://doi.org/10.1111/1750-3841.14171.
Divakaran, Karthika, et al. “Human Hepatic UGT2B15 Developmental Expression.” Toxicological Sciences, vol. 141, no. 1, Sept. 2014, pp. 292–99. PubMed Central, https://doi.org/10.1093/toxsci/kfu126.
Durcik, Martina, et al. “Last Piece in the Puzzle of Bisphenols BPA, BPS and BPF Metabolism: Kinetics of the in Vitro Sulfation Reaction.” Chemosphere, vol. 303, no. Pt 2, Sept. 2022, p. 135133. PubMed, https://doi.org/10.1016/j.chemosphere.2022.135133.
Gerona, Roy R., et al. “Direct Measurement of Bisphenol A (BPA), BPA Glucuronide and BPA Sulfate in a Diverse and Low-Income Population of Pregnant Women Reveals High Exposure, with Potential Implications for Previous Exposure Estimates: A Cross-Sectional Study.” Environmental Health, vol. 15, Apr. 2016, p. 50. PubMed Central, https://doi.org/10.1186/s12940-016-0131-2.
Gulizia, Alexandra M., et al. “Understanding Plasticiser Leaching from Polystyrene Microplastics.” Science of The Total Environment, vol. 857, Jan. 2023, p. 159099. ScienceDirect, https://doi.org/10.1016/j.scitotenv.2022.159099.
Hananeh, Wael Mahmoud, et al. “Exposure Assessment of Bisphenol A by Drinking Coffee from Plastic Cups.” Roczniki Panstwowego Zakladu Higieny, vol. 72, no. 1, 2021, pp. 49–53. PubMed, https://doi.org/10.32394/rpzh.2021.0146.
Hanioka, Nobumitsu, et al. “Effect of UDP-Glucuronosyltransferase 2B15 Polymorphism on Bisphenol A Glucuronidation.” Archives of Toxicology, vol. 85, no. 11, Nov. 2011, pp. 1373–81. Springer Link, https://doi.org/10.1007/s00204-011-0690-5.
Hoepner, Lori A., et al. “Bisphenol A and Adiposity in an Inner-City Birth Cohort.” Environmental Health Perspectives, vol. 124, no. 10, Oct. 2016, pp. 1644–50. PubMed, https://doi.org/10.1289/EHP205.
Hong, So-Hyeon, et al. “Urinary Bisphenol A Is Associated with Insulin Resistance and Obesity in Reproductive-Aged Women.” Clinical Endocrinology, vol. 86, no. 4, Apr. 2017, pp. 506–12. PubMed, https://doi.org/10.1111/cen.13270.
Kaur, Kulbir, et al. “Bisphenol A Induces Oxidative Stress and Mitochondrial Dysfunction in Lymphoblasts from Children with Autism and Unaffected Siblings.” Free Radical Biology & Medicine, vol. 76, Nov. 2014, pp. 25–33. PubMed, https://doi.org/10.1016/j.freeradbiomed.2014.07.030.
Ke, Zhang-Hong, et al. “Bisphenol A Exposure May Induce Hepatic Lipid Accumulation via Reprogramming the DNA Methylation Patterns of Genes Involved in Lipid Metabolism.” Scientific Reports, vol. 6, Aug. 2016, p. 31331. PubMed, https://doi.org/10.1038/srep31331.
Kim, Jin Hee, Yoon Hee Cho, et al. “MicroRNA Expression in Response to Bisphenol A Is Associated with High Blood Pressure.” Environment International, vol. 141, Aug. 2020, p. 105791. PubMed, https://doi.org/10.1016/j.envint.2020.105791.
Kim, Jin Hee, Mee-Ri Lee, et al. “Modification of the Association of Bisphenol A with Abnormal Liver Function by Polymorphisms of Oxidative Stress-Related Genes.” Environmental Research, vol. 147, May 2016, pp. 324–30. PubMed, https://doi.org/10.1016/j.envres.2016.02.026.
Lambré, Claude, et al. “Re‐evaluation of the Risks to Public Health Related to the Presence of Bisphenol A (BPA) in Foodstuffs.” EFSA Journal, vol. 21, no. 4, Apr. 2023, p. e06857. PubMed Central, https://doi.org/10.2903/j.efsa.2023.6857.
Li, Adela Jing, and Kurunthachalam Kannan. “Elevated Concentrations of Bisphenols, Benzophenones, and Antimicrobials in Pantyhose Collected from Six Countries.” Environmental Science & Technology, vol. 52, no. 18, Sept. 2018, pp. 10812–19. PubMed, https://doi.org/10.1021/acs.est.8b03129.
Luo, Yunyao, et al. “The Correlation between UDP-Glucuronosyltransferase Polymorphisms and Environmental Endocrine Disruptors Levels in Polycystic Ovary Syndrome Patients.” Medicine, vol. 99, no. 11, Mar. 2020, p. e19444. PubMed Central, https://doi.org/10.1097/MD.0000000000019444.
Martínez, M. Á., et al. “Bisphenol A Analogues (BPS and BPF) Present a Greater Obesogenic Capacity in 3T3-L1 Cell Line.” Food and Chemical Toxicology: An International Journal Published for the British Industrial Biological Research Association, vol. 140, June 2020, p. 111298. PubMed, https://doi.org/10.1016/j.fct.2020.111298.
Maserejian, Nancy N., et al. “Dental Sealants and Flowable Composite Restorations and Psychosocial, Neuropsychological, and Physical Development in Children.” Pediatric Dentistry, vol. 36, no. 1, 2014, pp. 68–75.
Menale, Ciro, et al. “Bisphenol A Is Associated with Insulin Resistance and Modulates Adiponectin and Resistin Gene Expression in Obese Children.” Pediatric Obesity, vol. 12, no. 5, Oct. 2017, pp. 380–87. PubMed, https://doi.org/10.1111/ijpo.12154.
Moon, Hi Gyu, et al. “Assessment of Potential Environmental and Human Risks for Bisphenol AF Contaminant.” Ecotoxicology and Environmental Safety, vol. 281, Aug. 2024, p. 116598. ScienceDirect, https://doi.org/10.1016/j.ecoenv.2024.116598.
Naomi, Ruth, et al. “Bisphenol A (BPA) Leading to Obesity and Cardiovascular Complications: A Compilation of Current In Vivo Study.” International Journal of Molecular Sciences, vol. 23, no. 6, Mar. 2022, p. 2969. PubMed Central, https://doi.org/10.3390/ijms23062969.
Noonan, Gregory O., et al. “Concentration of Bisphenol A in Highly Consumed Canned Foods on the U.S. Market.” Journal of Agricultural and Food Chemistry, vol. 59, no. 13, July 2011, pp. 7178–85. PubMed, https://doi.org/10.1021/jf201076f.
Novo, M., et al. “Endocrine Disruptors in Soil: Effects of Bisphenol A on Gene Expression of the Earthworm Eisenia Fetida.” Ecotoxicology and Environmental Safety, vol. 150, Apr. 2018, pp. 159–67. PubMed, https://doi.org/10.1016/j.ecoenv.2017.12.030.
Oliviero, Fabiana, et al. “Are BPA Substitutes as Obesogenic as BPA?” International Journal of Molecular Sciences, vol. 23, no. 8, Apr. 2022, p. 4238. PubMed Central, https://doi.org/10.3390/ijms23084238.
Rancière, Fanny, et al. “Exposure to Bisphenol A and Bisphenol S and Incident Type 2 Diabetes: A Case–Cohort Study in the French Cohort D.E.S.I.R.” Environmental Health Perspectives, vol. 127, no. 10, Oct. 2019, p. 107013. PubMed Central, https://doi.org/10.1289/EHP5159.
Rubin, Beverly S., et al. “Perinatal BPA Exposure Alters Body Weight and Composition in a Dose Specific and Sex Specific Manner: The Addition of Peripubertal Exposure Exacerbates Adverse Effects in Female Mice.” Reproductive Toxicology (Elmsford, N.Y.), vol. 68, Mar. 2017, pp. 130–44. PubMed Central, https://doi.org/10.1016/j.reprotox.2016.07.020.
—. “Perinatal BPA Exposure Alters Body Weight and Composition in a Dose Specific and Sex Specific Manner: The Addition of Peripubertal Exposure Exacerbates Adverse Effects in Female Mice.” Reproductive Toxicology (Elmsford, N.Y.), vol. 68, Mar. 2017, pp. 130–44. PubMed, https://doi.org/10.1016/j.reprotox.2016.07.020.
Savastano, Silvia, et al. “Bisphenol-A Plasma Levels Are Related to Inflammatory Markers, Visceral Obesity and Insulin-Resistance: A Cross-Sectional Study on Adult Male Population.” Journal of Translational Medicine, vol. 13, May 2015, p. 169. PubMed, https://doi.org/10.1186/s12967-015-0532-y.
Semerjian, Lucy, et al. “Detection of Bisphenol A in Thermal Paper Receipts and Assessment of Human Exposure: A Case Study from Sharjah, United Arab Emirates.” PLOS ONE, vol. 18, no. 3, Mar. 2023, p. e0283675. PubMed Central, https://doi.org/10.1371/journal.pone.0283675.
Shatalova, Ekaterina G., et al. “Genetic Polymorphisms in Human SULT1A1 and UGT1A1 Genes Associate with Breast Tumor Characteristics: A Case-Series Study.” Breast Cancer Research, vol. 7, no. 6, Sept. 2005, p. R909. Springer Link, https://doi.org/10.1186/bcr1318.
Sirivarasai, Jintana, et al. “Environmental Lead Exposure, Catalase Gene, and Markers of Antioxidant and Oxidative Stress Relation to Hypertension: An Analysis Based on the EGAT Study.” BioMed Research International, vol. 2015, 2015, p. 856319. PubMed Central, https://doi.org/10.1155/2015/856319.
Song, Won-Hee, et al. “Effect of Endocrine Disruptors on the Ratio of X and Y Chromosome-Bearing Live Spermatozoa.” Reproductive Toxicology (Elmsford, N.Y.), vol. 82, Dec. 2018, pp. 10–17. PubMed, https://doi.org/10.1016/j.reprotox.2018.09.002.
Stein, T. Peter. “Does Bisphenol A (BPA) Exposure Cause Human Diseases?” Biomedicines, vol. 12, no. 12, Dec. 2024, p. 2678. www.mdpi.com, https://doi.org/10.3390/biomedicines12122678.
Street, Christina M., et al. “Bisphenol-A Glucuronidation in Human Liver and Breast: Identification of UDP-Glucuronosyltransferases (UGTs) and Influence of Genetic Polymorphisms.” Xenobiotica; the Fate of Foreign Compounds in Biological Systems, vol. 47, no. 1, Jan. 2017, pp. 1–10. PubMed, https://doi.org/10.3109/00498254.2016.1156784.
—. “Bisphenol-A Glucuronidation in Human Liver and Breast: Identification of UDP-Glucuronosyltransferases (UGTs) and Influence of Genetic Polymorphisms.” Xenobiotica; the Fate of Foreign Compounds in Biological Systems, vol. 47, no. 1, Jan. 2017, pp. 1–10. PubMed Central, https://doi.org/10.3109/00498254.2016.1156784.
Tastet, Valentin, et al. “Interactions of Human Drug Transporters with Chemical Additives Present in Plastics: Potential Consequences for Toxicokinetics and Health.” Environmental Pollution, vol. 331, Aug. 2023, p. 121882. ScienceDirect, https://doi.org/10.1016/j.envpol.2023.121882.
Thoene, Michael, et al. “Bisphenol S in Food Causes Hormonal and Obesogenic Effects Comparable to or Worse than Bisphenol A: A Literature Review.” Nutrients, vol. 12, no. 2, Feb. 2020, p. 532. PubMed Central, https://doi.org/10.3390/nu12020532.
Trdan Lušin, Tina, et al. “Evaluation of Bisphenol A Glucuronidation According to UGT1A1*28 Polymorphism by a New LC-MS/MS Assay.” Toxicology, vol. 292, no. 1, Feb. 2012, pp. 33–41. PubMed, https://doi.org/10.1016/j.tox.2011.11.015.
Valentino, R., et al. “Bisphenol A Environmental Exposure and the Detrimental Effects on Human Metabolic Health: Is It Necessary to Revise the Risk Assessment in Vulnerable Population?” Journal of Endocrinological Investigation, vol. 39, no. 3, Mar. 2016, pp. 259–63. Springer Link, https://doi.org/10.1007/s40618-015-0336-1.
Yang, Zongying, et al. “Influence of Aryl Hydrocarbon Receptor and Sulfotransferase 1A1 on Bisphenol AF-Induced Clastogenesis in Human Hepatoma Cells.” Toxicology, vol. 471, Apr. 2022, p. 153175. ScienceDirect, https://doi.org/10.1016/j.tox.2022.153175.
Zhan, Lei, et al. “Prevalence of ABCB4 Polymorphisms in Gallstone Disease in Han-Chinese Population.” American Journal of Translational Research, vol. 8, no. 2, Feb. 2016, pp. 1218–27. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4846965/.
Zheng, Qiang, et al. “Association of Human Cytochrome P450 1A1 (CYP1A1) and Sulfotransferase 1A1 (SULT1A1) Polymorphisms with Differential Metabolism and Cytotoxicity of Aminoflavone.” Molecular Cancer Therapeutics, vol. 9, no. 10, Oct. 2010, pp. 2803–13. PubMed, https://doi.org/10.1158/1535-7163.MCT-10-0597.