Key takeaways:
~ Vitamin B6 is an important co-factor in hundreds of different enzymatic reactions.
~ Low levels of B6 are linked to an increased risk of diabetes, cardiovascular disease, neurodegenerative diseases, and cancer.
~ Vitamin B6 is also important for reducing oxidative stress and inflammation.
~ Genetic variants in several B6-related genes can increase your need for vitamin B6.
Vitamin B6: An Essential Cofactor
Vitamin B6 is an essential micronutrient that is used in hundreds of different reactions in the body. It’s a water-soluble vitamin that isn’t synthesized by the body nor stored long-term, so we need to replenish our supply regularly by eating foods that contain B6.[ref]
Vitamin B6 comes in multiple forms: pyridoxal, pyridoxine, and pyridoxamine, as well as phosphate ester forms.[ref] The active form of B6 most often used in reactions in the body is pyridoxal 5′-phosphate, abbreviated as PLP or P5P.
This is where genetics comes into play: Converting the forms of B6 we get in our foods into the active P5P form utilizes specific genes.
This article explains how vitamin B6 is used by cells, how it is absorbed and converted, and why genetic variants impact an individual’s need for different amounts and different forms of B6.
What does vitamin B6 do in the body?
The biologically active form of vitamin B6, pyridoxal 5′-phosphate (P5P), is used as a cofactor in hundreds of different cellular reactions.[ref]
Let me hit the highlights here:
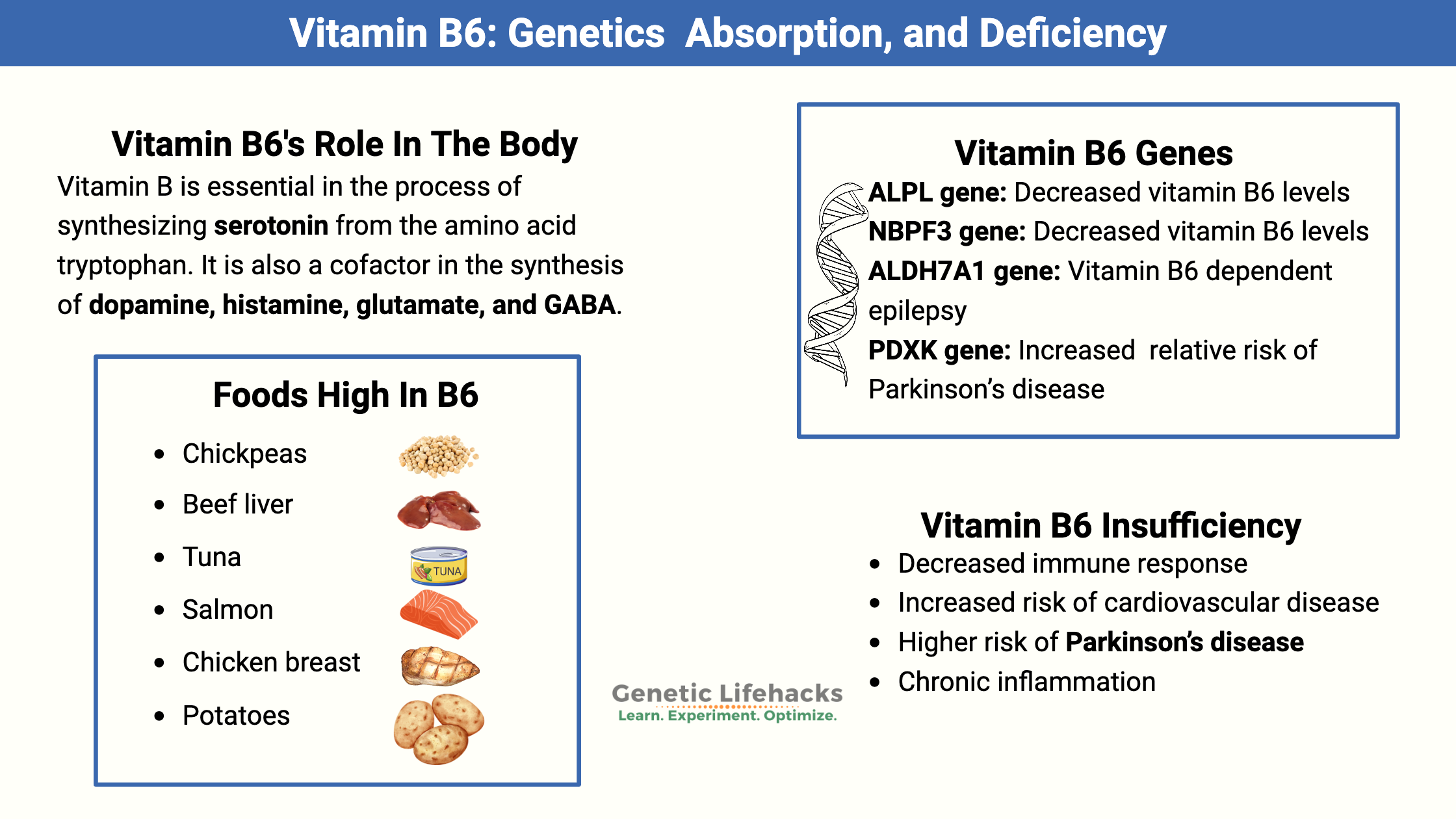
- Nervous system and neurotransmitters:
P5P is essential in the process of synthesizing serotonin from the amino acid tryptophan. It is also a cofactor in the synthesis of dopamine, histamine, glutamate, and GABA.[ref] - Hemoglobin:
P5P is needed as a coenzyme in creating heme, which is part of the body’s hemoglobin molecule to carry oxygen through the bloodstream. - Creating glucose:
P5P is a cofactor for synthesizing glucose from amino acids through the process of gluconeogenesis. This makes vitamin B6 important in brain energy and in regulating blood glucose levels. - Methylation cycle cofactor:
Vitamin B6 is a cofactor in the methylation cycle and is important for balancing homocysteine levels. It acts as a cofactor along with SHMT for the formation of methylfolate.
(Related article: Homocysteine) - Tryptophan metabolism:
Vitamin B6 is an important cofactor in the kynurenine pathway for tryptophan metabolism, resulting in the formation of niacin.
(Related article: Tryptophan, kynurenine, serotonin)
Symptoms of vitamin B6 deficiency:
Overview of how B6 deficiency affects the body:
| System/Condition | Symptom or Risk |
|---|---|
| Nervous System | Seizures, neuropathy, depression, Parkinson’s |
| Immune System | Decreased T/B cells, increased infection risk |
| Cardiovascular | Higher homocysteine, heart disease risk |
| Metabolic | Insulin resistance, higher diabetes risk |
| Inflammatory Diseases | Worsened symptoms in RA, IBD, COPD, etc. |
Insufficiency or borderline deficiency:
While full-blown deficiency is uncommon, having low levels, insufficiency, or borderline deficiency in vitamin B6 can impact your health. Traditionally, an active B6 concentration of 30 nmol/L has been used as the level of sufficiency in adults. However, more recent studies show that there are effects on cellular function, possibly starting with P5P concentrations less than 100 nmol/L, with more apparent differences seen at >50 nmol/L.[ref]
Here are several ways that low levels of vitamin B6 can impact your overall health and wellness:
- Decreased immune response:
Studies in older adults show that decreased levels of vitamin B6 have a significant impact on the immune system. Consuming a diet low in vitamin B6 for three weeks decreased T and B cells (white blood cells that fight invaders). Supplementary B6 (50 mg/day) brought immune function back to normal after four days.[ref] - Heart health:
Low vitamin B6 is also linked to an increased risk of cardiovascular disease.[ref]
Related article: Cardiovascular disease risk - Parkinson’s disease: Glutathione and dopamine
A low intake of B6 is linked to a higher risk of Parkinson’s disease.[ref] Not only is B6 important in dopamine production, but it is also important in the creation of glutathione (an antioxidant) in the brain.[ref] Parkinson’s patients on L-DOPA also often have low or deficient B6 levels.[ref]
Related article: Parkinson’s disease and genetic susceptibility - Chronic inflammation:
Inflammatory conditions, including rheumatoid arthritis, IBD, diabetes, cancer, and deep vein thrombosis, are all associated with low vitamin B6 levels.[ref] While inflammatory conditions are linked to low vitamin B6 levels, it may be (at least partly) because systemic inflammation decreases the body’s P5P levels, and dietary intake isn’t sufficient to meet the increased need.[ref]
Related article: Chronic inflammation and personalized solutions - Asthma and COPD:
A recent study showed that higher vitamin B6 intake correlates with higher FEV1 levels (lung function test) in CoPD. Similarly, vitamin B6 levels are lower in people with asthma than in healthy control groups. One connection is that low vitamin B6 interacts with IL-33, an inflammatory cytokine often involved in asthma or COPD. Another connection is that B6 is involved in the inflammatory signaling pathways in the lungs.[ref][ref][ref]
Related article: Asthma, genetic variants, and IL33 inflammation
Who is at risk of B6 deficiency?
A severe dietary deficiency of vitamin B6 is uncommon because B6 is found in many foods; most people get enough of it to meet their needs. However, diseases that cause decreased absorption of vitamins can also cause B6 deficiency.
- Alcoholics are at a higher risk of B vitamin deficiencies
- People on dialysis could also be at a higher risk.[ref]
- Celiac disease can also cause decreased absorption of vitamin B6.
Genetics:
Genetic variants in the genes involved in vitamin B6 absorption and conversion can also increase susceptibility to having low vitamin B6 levels.
Severe deficiency is a cause of epilepsy:
In the 1950s, an unintended experiment showed that when B6 was accidentally left out of infant formula, the babies had seizures. Severe, rare mutations that cause a genetic deficiency of the active form of vitamin B6 also cause epileptic seizures.[ref]
Essential for neurotransmitter synthesis, hemoglobin production, glucose metabolism, and methylation.
Deficiency or low levels are linked to immune dysfunction, cardiovascular risk, neurological issues, and inflammation.
Genetics can increase your need for B6 or affect how your body uses it.
Converting B6 from food to the active form, P5P:
Vitamin B6 is the generic name for six different compounds, including inactive forms from foods, the type made by bacteria, and the converted forms used in cellular reactions.
The conversion to the active form is where genetic variants are very important, so stick with me here and let’s dig into this in more detail…
Forms found in nature:
We get vitamin B6 from foods in the pyridoxamine (meats) and pyridoxine (fruits, vegetables, grains) forms. These forms of vitamin B6 are absorbed in the jejunum, which is the second part of the small intestine after the duodenum.[ref]
Absorption:
In the small intestines, vitamin B6 is absorbed mainly by transporter proteins (SLC19A2 or SLC19A3, which also transport thiamine). The transporters are dependent on the pH in the intestines. At higher levels of pyridoxine, the transporters are saturated and no longer transport pyridoxine.[ref] This naturally limits the amount of vitamin B6 you can absorb at one time.
Conversion:
The liver then converts these inactive forms of B6 into the active form, P5P (pyridoxal 5′-phosphate). The P5P form is what is used in cellular reactions, and 70-90% of the vitamin B6 circulating in plasma is this active form.[ref]
- The first step of the B6 conversion process in the liver involves pyridoxal kinase (PDKX gene).
- Then, a second step of conversion utilizes the pyridoxine phosphate (PNPO) oxidase enzyme. [ref]
Here’s an image to show you what is happening:
![Diagram of the conversion of dietary B6 to the active P5P pyridoxal 5 phosphate. P. Adapted from:[ref][ref]](https://www.geneticlifehacks.com/wp-content/uploads/2020/08/B6-Metabolism.png)
Epilepsy and movement disorders:
A severe deficiency caused by rare mutations in the PNPO enzyme can result in encephalopathy, epilepsy, and movement disorders from infancy. PNPO mutations are treated with high doses of P5P (active form), thus providing the active form of B6 without the need for conversion. In addition, mutations in ALDH7A1 in the lysine degradation pathway can also cause epilepsy that responds to P5P supplementation.[ref]
Regulation of active B6:
The cellular levels of P5P are fairly tightly regulated in the body with feedback loops and mechanisms in place. For example, high levels of P5P can be converted back to pyridoxal.[ref]
The ALPL gene encodes tissue-specific alkaline phosphatase, which plays a role in how P5P (active B6) is transported across membranes, including in the kidneys. Genetic variants in ALPL that increase the clearance of P5P through the kidneys result in lower vitamin B6 levels in the body. Conversely, rare non-functioning mutations in ALPL cause a genetic condition called hypophosphatasia, which in addition to high levels of pyrophosphate, causes high levels of P5P.[ref]
Peripheral Neuropathy and Vitamin B6:
Vitamin B6 deficiency is one of the more common causes of peripheral neuropathy.[ref][ref] On the other hand, excess consumption of vitamin B6 supplements for longer periods (months to years) has caused neuropathy or movement disorders in a few individuals. Some people report that high doses of B6 cause tingling and numbness.
How does vitamin B6 deficiency cause peripheral neuropathy – and- vitamin B6 supplements also cause neuropathy? It may come down to the type of vitamin B6 used as a supplement, along with the individual’s genetic variants.
There are two forms of B6 available as supplements: Pyridoxine HCL and P5P. Pyridoxine HCL is the more common type and is usually found in cheaper supplements. Recent research shows that supplementing with the pyridoxine form of B6 at higher doses can paradoxically inhibit the creation of P5P.[ref]
Researchers think that excess pyridoxine from high-dose supplements leads to the inhibition of PDXK, the enzyme that converts pyridoxine to P5P. This, in turn, leads to a decrease in the active form of B6 and likely affects GABA biosynthesis. GABA is an inhibitory neurotransmitter that relies on vitamin B6 as a cofactor for biosynthesis.[ref]
Genetic mutations in the PDXK gene, which converts pyridoxine from food into the active P5P form, can cause peripheral polyneuropathy.[ref]
Thus, a safer option for someone with peripheral neuropathy may be to supplement with the active P5P form of vitamin B6.
Enough background science. Let’s take a look at how your genetic variants interact with vitamin B6.
Genotype Report: How Genes Affect Your Vitamin B6 Needs
Overview of Gene Functions:
| Gene | Function in B6 Metabolism | Variant Effect | Impact/Notes |
|---|---|---|---|
| ALPL | Important in B6 excretion | Increased activity leads to more B6 being excreted by the kidneys | Low P5P |
| PDXK | Converts pyridoxine to P5P | Reduced activity impairs conversion to P5P | Peripheral neuropathy, low P5P |
| PNPO | Final step to active P5P | Severe deficiency is possible with rare mutations | Epilepsy, movement disorders |
| ALDH7A1 | Lysine degradation, B6-dependent | Disrupts recycling, Pyridoxine-dependent epilepsy | Responds to P5P supplementation |
Lifehacks: What can you do if you have a B6-related genetic variant?
Let’s take a look at:
- How much vitamin B6 is needed
- Two forms of vitamin B6 are available as supplements
- Clinical trials involving B6 and the doses used
- Food sources of B6
- Safety concerns
- How oral contraceptives impact B6 levels
How much vitamin B6?
The US RDA for vitamin B6 is 1.3 to 1.7 mg/day for adults. Adults over 50 may need more B6 (1.7mg/day).[ref] The upper daily limit of B6 is set at 100 mg/day for adults.[ref] The RDA is set at the levels to prevent severe nutrient deficiency, so it may not be the optimal amount that you need.
Consider any genetic variants above, as they may impact whether you need more vitamin B6 than average.
In Summary:
Genetic variants can significantly impact your vitamin B6 metabolism and the amount and type you need. Understanding your genetic variants, diet, and health conditions can help you optimize B6 intake and wellness. Keep in mind that future research may reveal even more about personalized nutrition and B6 requirements.
Related Articles and Topics:
Rheumatoid Arthritis: Genetics, Root Causes, and Treatment Research
References:
Brown, Mary J., et al. “Vitamin B6 Deficiency.” StatPearls, StatPearls Publishing, 2022. PubMed, http://www.ncbi.nlm.nih.gov/books/NBK470579/.
Clayton, Peter T. “B6-Responsive Disorders: A Model of Vitamin Dependency.” Journal of Inherited Metabolic Disease, vol. 29, no. 2–3, June 2006, pp. 317–26. PubMed, https://doi.org/10.1007/s10545-005-0243-2.
Farhad, Khosro, et al. “Causes of Neuropathy in Patients Referred as ‘Idiopathic Neuropathy.’” Muscle & Nerve, vol. 53, no. 6, June 2016, pp. 856–61. PubMed, https://doi.org/10.1002/mus.24969.
Gregory, Jesse F. “Accounting for Differences in the Bioactivity and Bioavailability of Vitamers.” Food & Nutrition Research, vol. 56, Apr. 2012, p. 10.3402/fnr.v56i0.5809. PubMed Central, https://doi.org/10.3402/fnr.v56i0.5809.
Hazra, Aditi, et al. “Genome-Wide Significant Predictors of Metabolites in the One-Carbon Metabolism Pathway.” Human Molecular Genetics, vol. 18, no. 23, Dec. 2009, pp. 4677–87. PubMed Central, https://doi.org/10.1093/hmg/ddp428.
Hinz, Marty, et al. “The Parkinson’s Disease Death Rate: Carbidopa and Vitamin B6.” Clinical Pharmacology: Advances and Applications, vol. 6, 2014, pp. 161–69. PubMed, https://doi.org/10.2147/CPAA.S70707.
Ishihara, Junko, et al. “Intake of Folate, Vitamin B6 and Vitamin B12 and the Risk of CHD: The Japan Public Health Center-Based Prospective Study Cohort I.” Journal of the American College of Nutrition, vol. 27, no. 1, Feb. 2008, pp. 127–36. PubMed, https://doi.org/10.1080/07315724.2008.10719684.
Keene, Keith L., et al. “Genetic Associations with Plasma B12, B6, and Folate Levels in an Ischemic Stroke Population from the Vitamin Intervention for Stroke Prevention (VISP) Trial.” Frontiers in Public Health, vol. 2, Aug. 2014, p. 112. PubMed Central, https://doi.org/10.3389/fpubh.2014.00112.
Laciak, Adrian R., et al. “Structural Analysis of Pathogenic Mutations Targeting Glu427 of ALDH7A1, the Hot Spot Residue of Pyridoxine-Dependent Epilepsy.” Journal of Inherited Metabolic Disease, vol. 43, no. 3, May 2020, pp. 635–44. PubMed, https://doi.org/10.1002/jimd.12184.
Meydani, S. N., et al. “Vitamin B-6 Deficiency Impairs Interleukin 2 Production and Lymphocyte Proliferation in Elderly Adults.” The American Journal of Clinical Nutrition, vol. 53, no. 5, May 1991, pp. 1275–80. PubMed, https://doi.org/10.1093/ajcn/53.5.1275.
Modica, Joseph S., et al. “Pearls and Oy-Sters: Vitamin B6 Deficiency Presenting with New-Onset Epilepsy and Status Epilepticus in a Patient with Parkinson Disease.” Neurology, vol. 94, no. 24, June 2020, pp. e2605–07. n.neurology.org, https://doi.org/10.1212/WNL.0000000000009647.
“Nutrient Ranking Tool.” Myfooddata, https://tools.myfooddata.com/nutrient-ranking-tool. Accessed 29 July 2022.
Office of Dietary Supplements – Vitamin B6. https://ods.od.nih.gov/factsheets/VitaminB6-HealthProfessional/. Accessed 29 July 2022.
Olde Loohuis, Loes M., et al. “The Alkaline Phosphatase (ALPL) Locus Is Associated with B6 Vitamer Levels in CSF and Plasma.” Genes, vol. 10, no. 1, Dec. 2018, p. 8. PubMed Central, https://doi.org/10.3390/genes10010008.
Romagnolo, Alberto, et al. “Levodopa-Induced Neuropathy: A Systematic Review.” Movement Disorders Clinical Practice, vol. 6, no. 2, Feb. 2019, pp. 96–103. PubMed, https://doi.org/10.1002/mdc3.12688.
Scott, T. M., et al. “B-Vitamin Therapy for Kidney Transplant Recipients Lowers Homocysteine and Improves Selective Cognitive Outcomes in the Randomized FAVORIT Ancillary Cognitive Trial.” The Journal of Prevention of Alzheimer’s Disease, vol. 4, no. 3, 2017, pp. 174–82. PubMed, https://doi.org/10.14283/jpad.2017.15.
Shen, Liang. “Associations between B Vitamins and Parkinson’s Disease.” Nutrients, vol. 7, no. 9, Aug. 2015, pp. 7197–208. PubMed, https://doi.org/10.3390/nu7095333.
Tanaka, Toshiko, et al. “Genome-Wide Association Study of Vitamin B6, Vitamin B12, Folate, and Homocysteine Blood Concentrations.” American Journal of Human Genetics, vol. 84, no. 4, Apr. 2009, pp. 477–82. PubMed Central, https://doi.org/10.1016/j.ajhg.2009.02.011.
Ueland, Per Magne, et al. “Direct and Functional Biomarkers of Vitamin B6 Status.” Annual Review of Nutrition, vol. 35, 2015, pp. 33–70. PubMed Central, https://doi.org/10.1146/annurev-nutr-071714-034330.
Ulvik, Arve, et al. “Evidence for Increased Catabolism of Vitamin B-6 during Systemic Inflammation.” The American Journal of Clinical Nutrition, vol. 100, no. 1, July 2014, pp. 250–55. PubMed, https://doi.org/10.3945/ajcn.114.083196.
VCV000017995.22 – ClinVar – NCBI. https://www.ncbi.nlm.nih.gov/clinvar/variation/17995/. Accessed 29 July 2022.
Vrolijk, Misha F., et al. “The Vitamin B6 Paradox: Supplementation with High Concentrations of Pyridoxine Leads to Decreased Vitamin B6 Function.” Toxicology in Vitro: An International Journal Published in Association with BIBRA, vol. 44, Oct. 2017, pp. 206–12. PubMed, https://doi.org/10.1016/j.tiv.2017.07.009.
Wang, Junjuan, et al. “The Effects of a Single Oral Dose of Pyridoxine on Alpha-Aminoadipic Semialdehyde, Piperideine-6-Carboxylate, Pipecolic Acid, and Alpha-Aminoadipic Acid Levels in Pyridoxine-Dependent Epilepsy.” Frontiers in Pediatrics, vol. 7, Aug. 2019, p. 337. PubMed Central, https://doi.org/10.3389/fped.2019.00337.
Wei, Yao, et al. “Pyridoxine Induces Glutathione Synthesis via PKM2-Mediated Nrf2 Transactivation and Confers Neuroprotection.” Nature Communications, vol. 11, no. 1, Feb. 2020, p. 941. PubMed, https://doi.org/10.1038/s41467-020-14788-x.
Zhang, Dong-Mei, et al. “Efficacy of Vitamin B Supplementation on Cognition in Elderly Patients With Cognitive-Related Diseases.” Journal of Geriatric Psychiatry and Neurology, vol. 30, no. 1, Jan. 2017, pp. 50–59. PubMed, https://doi.org/10.1177/0891988716673466.