Key takeaways:
~ Nootropics are supplements used to boost cognition and memory. In other words, smart drugs.
~ Genetic variants may alter your reactions to different supplements and nootropics.
Personalizing Your Nootropic Information:
This article covers published research studies on several popular nootropics. I’ll explain the research on how the substance works and the genes connected to the mechanism of action.
Let me be upfront…
Research directly connecting genetic variants to whether a smart drug will work for you is slim. Instead, I’m connecting some dots and giving you the background information to start your research and experimenting.
Please talk with your doctor or pharmacist if you have any questions about a supplement – especially if you are currently on prescription medication.
Noopept (cognitive function, memory)
Noopept is a dipeptide that the Russians discovered in the 1960s. The Russian government had a program to develop cognitive-enhancing drugs, and noopept now has decades of research on it with both human and animal studies.
Noopept may enhance memory and cognitive function in a couple of ways:
- Noopept can increase HIF-1 activity. HIF-1 (hypoxia factor 1) is important in low oxygen states.[ref] In turn, HIF-1 activates other genes that help cells respond to lower oxygen levels. In the brain, this increases energy metabolism in the mitochondria and activates proteins responsible for controlling GABA receptors.[ref]
- Noopept also enhances BDNF (brain-derived neurotropic fact) and NGF (nerve growth factor) expression.[ref][ref] Both BDNF and NGF are important in cognitive function and brain plasticity.
- The noopept metabolite, cyclopropyl glycine, binds to AMPA receptors in the brain.[ref] AMPA receptors are glutamate receptors essential to brain plasticity and neuronal transmission.[ref]
Research on Noopept and the brain
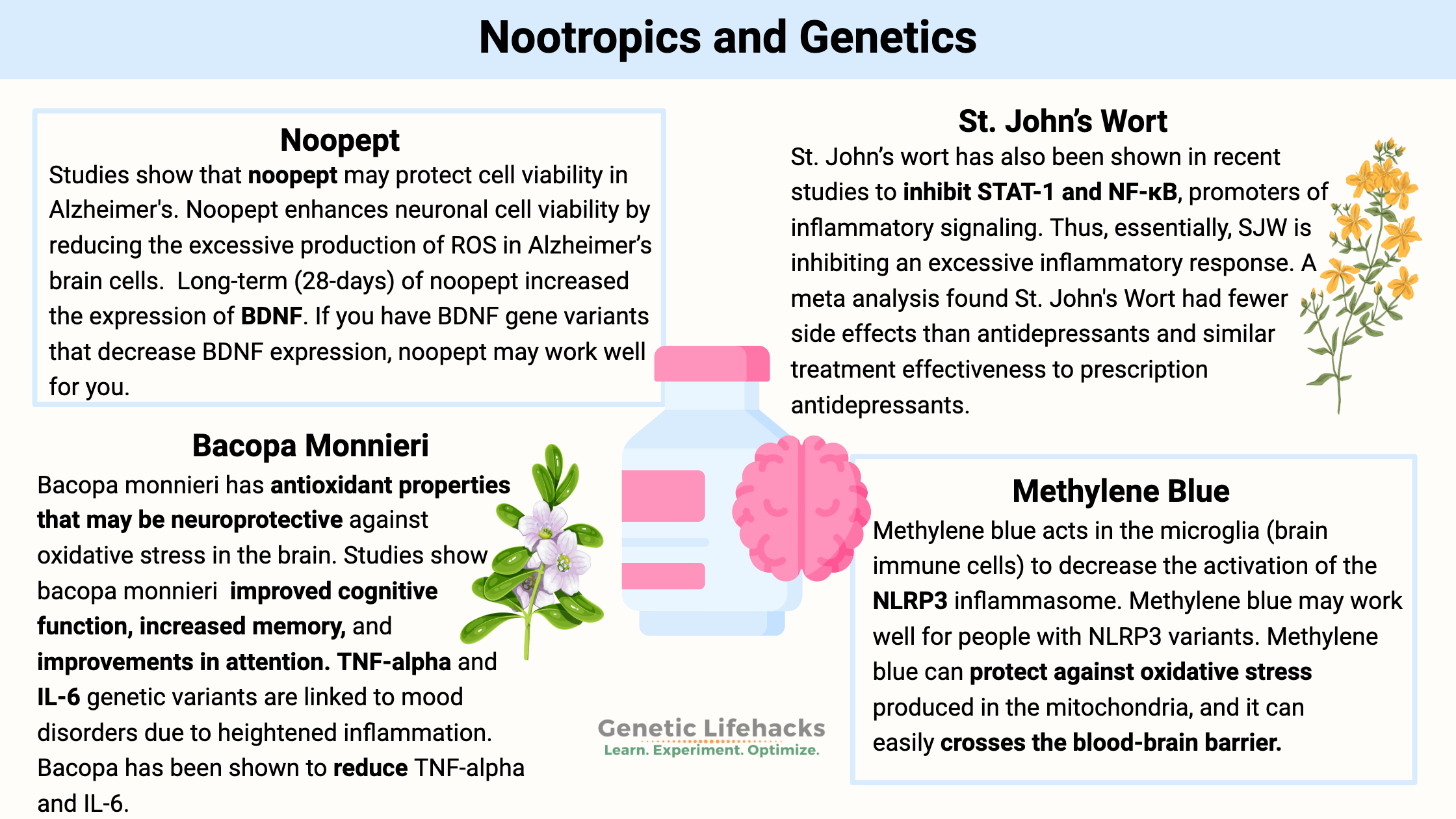
Recently, research has focused on using neuropeptides such as noopept for Alzheimer’s disease. Phase III and other clinical trials have been done in Russia. Unfortunately for me, much of the research is published in Russian. A recent cell study showed that noopept enhances neuronal cell viability by reducing the excessive production of ROS in Alzheimer’s brain cells. This protects against amyloid-beta toxicity.[ref]
Cell studies show that noopept may protect cell viability in an Alzheimer’s model.[ref]
Animal studies on noopept show that it can eliminate the symptoms of learned helplessness.[ref]
A clinical trial in Russia investigated using Noopept for cognitive dysfunction in concussion patients. Oddly, the other arm of the trial used piracetam instead of a placebo. Both noopept and piracetam (a similar drug) showed similar efficacy. Of interest here is that there were fewer linked side effects with noopept than piracetam.[ref]
Another clinical trial in Russia found mild improvements from noopept in stroke patients. The trial (with a placebo control) used a 20 mg daily dose for two months.[ref]
Safety is essential when looking into nootropics. Let’s take a look at what research shows on noopept safety.
- Animal studies also show that Noopept does not seem to increase cell proliferation. It is important because HIF-1A is increased in cancer cells.[ref]
- Additionally, animal studies show that noopept is not genotoxic (does not cause DNA damage).[ref]
Noopept: Genotype Report
Bacopa monnieri (memory supplement)
Bacopa monnieri, also known as Brahmi, is a native plant found in the wetlands of Australia and India. It has been used in traditional Ayurvedic medicine for over 1400 years as a way to sharpen intellect and help with memory.[ref]
How does bacopa work?
- The active compounds in Bacopa include bacosides, which can cross the blood-brain barrier easily.[ref]
- Studies show that Bacopa monnieri has antioxidant properties that may be neuroprotective against oxidative stress in the brain.[ref]
- Animal studies show that it restores acetylcholine levels in aged brains to that of young animals. Additionally, Bacopa monnieri modulates neurotransmitter levels.[ref]
- Cell studies show that Bacopa monnieri inhibits the release of proinflammatory cytokines – reducing TNF-alpha and IL-6 in brain cells.[ref]
- Animal studies also show that the improvements in learning and memory with Bacopa monnieri accompany an increase in amygdala function via dendritic growth.[ref]
Research Studies on Bacopa monnieri
- A randomized controlled trial of adults aged 40-65 showed that after three months of Bacopa supplements, the study participants increased memory of new information.[ref]
- A randomized trial in medical students found that 150 mg Bacopa monnieri twice daily for six weeks improved cognitive function.[ref]
- Studies of Bacopa supplements for children and teens show that it helps to improve memory. Study participants also showed improvements in attention and a reduction in hyperactivity. [ref]
- A meta-analysis of nine studies concluded that Bacopa monnieri improves cognition and speed of attention.[ref]
Bacopa: Genotype Report
Methylene blue (mitochondria, brain energy)
Methylene blue was first developed as a textile dye but was quickly found to stain cells under a microscope. Early medical uses included using methylene blue to treat malaria. When used in higher amounts, methylene blue turns urine a blue color. Thus, it was included with psychiatric medications to see if the patient was compliant with taking the drugs. It led to the discovery that methylene blue itself had antipsychotic effects by inhibiting MAOA.[ref]
Currently, methylene blue is primarily used as a medication for methemoglobinemia and during certain heart surgeries to increase oxygenation in the blood. It is also used in periodontal health along with phototherapy.
What else does methylene blue do? Methylene blue acts as a redox recycler, moving electrons.
In the mitochondria, methylene blue can act in complex I and complex IV as an alternative electron transporter. It can protect against oxidative stress produced in the mitochondria.[ref]
Methylene blue easily crosses the blood-brain barrier. The brain uses a lot of energy, produced in mitochondria, of course. A decrease in mitochondrial function in the brain is thought to be at the root of neurodegenerative diseases.
Methylene blue clinical trials:
- A double-blind crossover study using 15 mg methylene blue in bipolar patients showed that it improved depression symptoms.[ref]
- In COVID-19 patients, methylene blue improved blood oxygen levels, decreased hospitalization days, and decreased mortality.[ref]
- Clinical trials in Alzheimer’s patients showed that higher doses of methylene blue didn’t have a benefit compared to the placebo. But the placebo group was also taking a lower dose of methylene blue to turn their urine blue. Re-analysis of the data shows that methylene blue (or derivative, patentable molecules) may be helpful in Alzheimer’s at low doses.[ref][ref]
- An fMRI study found that methylene blue alters cerebral blood flow. The randomized-controlled trial found that methylene blue enhances resting-state functional connectivity in the areas of the brain related to perception and memory.[ref]
As a nootropic, methylene blue is used in very low doses (microdoses) to enhance cognitive function.
How does methylene blue work as a nootropic?
There are several ways that methylene blue acts in the body.
- One mechanism of action is that it is an MAOA inhibitor, which should cause a slight increase in neurotransmitter levels.
- Another way that methylene blue works is to increase mitochondrial function in the brain.[ref]
- Research also shows that methylene blue decreases the activation of the NLRP3 inflammasome in the microglia (reduces inflammation in the brain).[ref]
- Methylene blue acts as an antioxidant by upregulating the Nrf2 antioxidant response pathway.[ref]
Related article: MAO-A and MAO-B: Neurotransmitter levels, genetics, and studies
Methylene Blue: Genotype Report
St. John’s Wort (mood)
Saint John’s Wort (SJW) is an herbal supplement that has been used for centuries to improve mood. With thousands of studies, St. John’s wort is one of the most well-studied herbal remedies for depression.[ref]
How does it work?
St. John’s wort has also been shown in recent studies to inhibit STAT-1 and NF-κB, promoters of inflammatory signaling. Thus, essentially, SJW is inhibiting an excessive inflammatory response. This inhibition has been shown in people with diabetes.[ref]
Cell studies show that SJW protects microglia in the brain from oxidative stress. The study also shows that it has anti-inflammatory properties in the brain as well.[ref]
Hyperforin is one of the main active components of St. John’s wort.
- Stress response: A recent study showed that hyperforin could reverse stress-induced increases in FKBP5.[ref] Why is this important? FKBP5 interacts with the glucocorticoid receptor in response to stress.
- Mitochondria: In a cell study looking at amyloid-beta plaque, researchers found that hyperforin acts upon FIS1, a mitochondrial protein important in fission-fusion events.[ref] Mitochondrial function, especially in the brain, is important in the prevention of neurodegeneration as well as mood disorders. (Read more about mitochondria and MDD)
Hyperforin has also been shown in cell studies to activate TRPC6 channels. This channel is important in moving zinc and calcium across the mitochondrial membrane.[ref] Animal studies point to TRPC6 as being important in brain plasticity.
Research studies on St. John’s Wort
There are many studies on SJW for depression, and the results vary quite a bit.
Negative clinical trials:
- Neither sertraline nor SJW differed from placebo in MDD.[ref]
- Again, neither SJW nor sertraline differed from placebo in depression.[ref]
- SJW did no better than placebo with OCD.[ref]
Positive clinical trials:
- A meta-analysis found that SJW had fewer side effects than antidepressants and similar treatment effectiveness to prescription antidepressants.[ref]
- Another meta-analysis found that St. John’s wort works better than placebo in treating depression.[ref]
- Another trial in MDD found that SJW was more effective than fluoxetine in depression.[ref]
Stack with Zinc (if deficient): The mitochondrial impact of hyperforin includes its TRPC6 channel activation, moving zinc in the mitochondria. Studies on depression show that zinc supplementation augments antidepressant treatment even in treatment-resistant patients.[ref][ref]
St. John’s Wort: Genotype Report
Related Articles and Topics:
MAO-A and MAO-B: Neurotransmitter levels, genetics, and warrior gene studies
References:
Aguiar, Sebastian, and Thomas Borowski. “Neuropharmacological Review of the Nootropic Herb Bacopa Monnieri.” Rejuvenation Research, vol. 16, no. 4, Aug. 2013, pp. 313–26. PubMed Central, https://doi.org/10.1089/rej.2013.1431.
Alzobaidi, Nafaa, et al. “Bioactive Compounds and Traditional Herbal Medicine: Promising Approaches for the Treatment of Dementia.” Degenerative Neurological and Neuromuscular Disease, vol. 11, Apr. 2021, pp. 1–14. PubMed Central, https://doi.org/10.2147/DNND.S299589.
Amelin, A. V., et al. “[Noopept in the treatment of mild cognitive impairment in patients with stroke].” Zhurnal Nevrologii I Psikhiatrii Imeni S.S. Korsakova, vol. 111, no. 10 Pt 1, 2011, pp. 44–46.
Boyko, S. S., et al. “[Pharmacokinetics of noopept and its active metabolite cycloprolyl glycine in rats].” Biomeditsinskaia Khimiia, vol. 64, no. 5, Sept. 2018, pp. 455–58. PubMed, https://doi.org/10.18097/PBMC20186405455.
Desrivières, S., et al. “Single Nucleotide Polymorphism in the Neuroplastin Locus Associates with Cortical Thickness and Intellectual Ability in Adolescents.” Molecular Psychiatry, vol. 20, no. 2, Feb. 2015, pp. 263–74. PubMed, https://doi.org/10.1038/mp.2013.197.
Feng, Bo, et al. “Association of Tumor Necrosis Factor α -308G/A and Interleukin-6 -174G/C Gene Polymorphism with Pneumonia-Induced Sepsis.” Journal of Critical Care, vol. 30, no. 5, Oct. 2015, pp. 920–23. PubMed, https://doi.org/10.1016/j.jcrc.2015.04.123.
Formicola, Daniela, et al. “Common Variants in the Regulative Regions of GRIA1 and GRIA3 Receptor Genes Are Associated with Migraine Susceptibility.” BMC Medical Genetics, vol. 11, June 2010, p. 103. PubMed Central, https://doi.org/10.1186/1471-2350-11-103.
Gudasheva, T. A., et al. “The Anxiolytic Effect of the Neuropeptide Cycloprolylglycine Is Mediated by AMPA and TrkB Receptors.” Doklady. Biochemistry and Biophysics, vol. 493, no. 1, July 2020, pp. 190–92. PubMed, https://doi.org/10.1134/S1607672920040067.
Guo, Jun-Cheng, et al. “Correlations of Four Genetic Single Nucleotide Polymorphisms in Brain-Derived Neurotrophic Factor with Posttraumatic Stress Disorder.” Psychiatry Investigation, vol. 15, no. 4, Apr. 2018, pp. 407–12. PubMed Central, https://doi.org/10.30773/pi.2017.06.17.1.
Kang, Min-Jung, et al. “Associations between Single Nucleotide Polymorphisms of MMP2, VEGF, and HIF1A Genes and the Risk of Developing Colorectal Cancer.” Anticancer Research, vol. 31, no. 2, Feb. 2011, pp. 575–84.
Kean, James D., et al. “A Systematic Review of the Ayurvedic Medicinal Herb Bacopa Monnieri in Child and Adolescent Populations.” Complementary Therapies in Medicine, vol. 29, Dec. 2016, pp. 56–62. PubMed, https://doi.org/10.1016/j.ctim.2016.09.002.
Konac, Ece, et al. “An Investigation of Relationships between Hypoxia-Inducible Factor-1 Alpha Gene Polymorphisms and Ovarian, Cervical and Endometrial Cancers.” Cancer Detection and Prevention, vol. 31, no. 2, 2007, pp. 102–09. PubMed, https://doi.org/10.1016/j.cdp.2007.01.001.
Kongkeaw, Chuenjid, et al. “Meta-Analysis of Randomized Controlled Trials on Cognitive Effects of Bacopa Monnieri Extract.” Journal of Ethnopharmacology, vol. 151, no. 1, 2014, pp. 528–35. PubMed, https://doi.org/10.1016/j.jep.2013.11.008.
Kumar, Navneet, et al. “Efficacy of Standardized Extract of Bacopa Monnieri (Bacognize®) on Cognitive Functions of Medical Students: A Six-Week, Randomized Placebo-Controlled Trial.” Evidence-Based Complementary and Alternative Medicine: ECAM, vol. 2016, 2016, p. 4103423. PubMed, https://doi.org/10.1155/2016/4103423.
Larruskain, Jon, et al. “Genetic Variants and Hamstring Injury in Soccer: An Association and Validation Study.” Medicine and Science in Sports and Exercise, vol. 50, no. 2, Feb. 2018, pp. 361–68. PubMed, https://doi.org/10.1249/MSS.0000000000001434.
Ma, Xian-Yong, et al. “Association between BDNF Rs6265 and Obesity in the Boston Puerto Rican Health Study.” Journal of Obesity, vol. 2012, Dec. 2012, p. e102942. www.hindawi.com, https://doi.org/10.1155/2012/102942.
Majumder, Poulami, et al. “Association of Tumor Necrosis Factor-α (TNF-α) Gene Promoter Polymorphisms with Aggressive and Chronic Periodontitis in the Eastern Indian Population.” Bioscience Reports, vol. 38, no. 4, Aug. 2018, p. BSR20171212. PubMed, https://doi.org/10.1042/BSR20171212.
Mandelman, Samuel D., and Elena L. Grigorenko. “BDNF Val66Met and Cognition: All, None, or Some? A Meta-Analysis of the Genetic Association.” Genes, Brain, and Behavior, vol. 11, no. 2, Mar. 2012, pp. 127–36. PubMed Central, https://doi.org/10.1111/j.1601-183X.2011.00738.x.
McPhee, J. S., et al. “HIF1A P582S Gene Association with Endurance Training Responses in Young Women.” European Journal of Applied Physiology, vol. 111, no. 9, Sept. 2011, pp. 2339–47. PubMed, https://doi.org/10.1007/s00421-011-1869-4.
Nagy, Geza, et al. “Association of Hypoxia Inducible Factor-1 Alpha Gene Polymorphism with Both Type 1 and Type 2 Diabetes in a Caucasian (Hungarian) Sample.” BMC Medical Genetics, vol. 10, Aug. 2009, p. 79. PubMed, https://doi.org/10.1186/1471-2350-10-79.
Nemetchek, Michelle D., et al. “The Ayurvedic Plant Bacopa Monnieri Inhibits Inflammatory Pathways in the Brain.” Journal of Ethnopharmacology, vol. 197, Feb. 2017, pp. 92–100. PubMed Central, https://doi.org/10.1016/j.jep.2016.07.073.
Ostrovskaya, R. U., S. S. Yagubova, et al. “Neuroprotective Dipeptide Noopept Prevents DNA Damage in Mice with Modeled Prediabetes.” Bulletin of Experimental Biology and Medicine, vol. 168, no. 2, Dec. 2019, pp. 233–37. PubMed, https://doi.org/10.1007/s10517-019-04681-z.
Ostrovskaya, R. U., T. A. Gudasheva, et al. “Noopept Stimulates the Expression of NGF and BDNF in Rat Hippocampus.” Bulletin of Experimental Biology and Medicine, vol. 146, no. 3, Sept. 2008, pp. 334–37. PubMed, https://doi.org/10.1007/s10517-008-0297-x.
Ostrovskaya, Rita U, et al. “Neuroprotective Effect of Novel Cognitive Enhancer Noopept on AD-Related Cellular Model Involves the Attenuation of Apoptosis and Tau Hyperphosphorylation.” Journal of Biomedical Science, vol. 21, no. 1, Aug. 2014, p. 74. PubMed Central, https://doi.org/10.1186/s12929-014-0074-2.
Ozan, Erol, et al. “The Effect of Depression, BDNF Gene Val66met Polymorphism and Gender on Serum BDNF Levels.” Brain Research Bulletin, vol. 81, no. 1, Jan. 2010, pp. 61–65. ScienceDirect, https://doi.org/10.1016/j.brainresbull.2009.06.022.
Roodenrys, Steven, et al. “Chronic Effects of Brahmi (Bacopa Monnieri) on Human Memory.” Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology, vol. 27, no. 2, Aug. 2002, pp. 279–81. PubMed, https://doi.org/10.1016/S0893-133X(01)00419-5.
Simpson, Tamara, et al. “Bacopa Monnieri as an Antioxidant Therapy to Reduce Oxidative Stress in the Aging Brain.” Evidence-Based Complementary and Alternative Medicine : ECAM, vol. 2015, 2015, p. 615384. PubMed Central, https://doi.org/10.1155/2015/615384.
Tavares, M., et al. “Tumour Necrosis Factor-Alpha (-308G/A) Promoter Polymorphism Is Associated with Ulcerative Colitis in Brazilian Patients.” International Journal of Immunogenetics, vol. 43, no. 6, Dec. 2016, pp. 376–82. PubMed, https://doi.org/10.1111/iji.12289.
Uyanaev, A. A., and V. P. Fisenko. “Studies of Long-Term Noopept and Afobazol Treatment in Rats with Learned Helplessness Neurosis.” Bulletin of Experimental Biology and Medicine, vol. 142, no. 2, Aug. 2006, pp. 202–04. PubMed, https://doi.org/10.1007/s10517-006-0327-5.
Vakhitova, Y. V., et al. “Molecular Mechanism Underlying the Action of Substituted Pro-Gly Dipeptide Noopept.” Acta Naturae, vol. 8, no. 1, 2016, pp. 82–89. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4837574/.
Voineskos, Aristotle N., et al. “The Brain-Derived Neurotrophic Factor Val66Met Polymorphism and Prediction of Neural Risk for Alzheimer Disease.” Archives of General Psychiatry, vol. 68, no. 2, Feb. 2011, pp. 198–206. PubMed, https://doi.org/10.1001/archgenpsychiatry.2010.194.
Vollala, Venkata Ramana, et al. “Enhancement of Basolateral Amygdaloid Neuronal Dendritic Arborization Following Bacopa Monniera Extract Treatment in Adult Rats.” Clinics, vol. 66, no. 4, Apr. 2011, pp. 663–71. PubMed Central, https://doi.org/10.1590/S1807-59322011000400023.
Watanabe, Yuichiro, et al. “Association of the BDNF C270T Polymorphism with Schizophrenia: Updated Meta-Analysis.” Psychiatry and Clinical Neurosciences, vol. 67, no. 2, Feb. 2013, pp. 123–25. PubMed, https://doi.org/10.1111/pcn.12018.
Xu, Lianping, et al. “The Analysis of Two BDNF Polymorphisms G196A/C270T in Chinese Sporadic Amyotrophic Lateral Sclerosis.” Frontiers in Aging Neuroscience, vol. 9, May 2017, p. 135. PubMed Central, https://doi.org/10.3389/fnagi.2017.00135.
Yang, Xi, et al. “HIF-1α 1772 C/T and 1790 G/A Polymorphisms Are Significantly Associated with Higher Cancer Risk: An Updated Meta-Analysis from 34 Case-Control Studies.” PLoS ONE, vol. 8, no. 11, Nov. 2013, p. e80396. PubMed Central, https://doi.org/10.1371/journal.pone.0080396.
Zainullina, L. F., T. V. Ivanova, S. V. Sadovnikov, et al. “Cognitive Enhancer Noopept Activates Transcription Factor HIF-1.” Doklady. Biochemistry and Biophysics, vol. 494, no. 1, Sept. 2020, pp. 256–60. PubMed, https://doi.org/10.1134/S1607672920050129.
Zainullina, L. F., T. V. Ivanova, R. U. Ostrovskaya, et al. “Drug with Neuroprotective Properties Noopept Does Not Stimulate Cell Proliferation.” Bulletin of Experimental Biology and Medicine, vol. 166, no. 4, Feb. 2019, pp. 466–68. PubMed, https://doi.org/10.1007/s10517-019-04373-8.
Zaki, Nevin F. W., et al. “The Association of BDNF Gene Polymorphism with Cognitive Impairment in Insomnia Patients.” Progress in Neuro-Psychopharmacology & Biological Psychiatry, vol. 88, Jan. 2019, pp. 253–64. PubMed, https://doi.org/10.1016/j.pnpbp.2018.07.025.
Debbie Moon is the founder of Genetic Lifehacks. Fascinated by the connections between genes, diet, and health, her goal is to help you understand how to apply genetics to your diet and lifestyle decisions. Debbie has a BS in engineering from Colorado School of Mines and an MSc in biological sciences from Clemson University. Debbie combines an engineering mindset with a biological systems approach to help you understand how genetic differences impact your optimal health.