Key takeaways:
~ Phase I and phase II detoxification are the primary ways your body eliminates toxins.
~ Genetic variants in these pathways affect how well you detoxify certain substances.
Detoxification and Genetic Pathways:
Your body is remarkably capable of ridding itself of harmful substances through complex detoxification pathways. In today’s world, we are all exposed to various toxicants (manufactured toxins) through pesticide residue, air pollution, skin care products, and medications. Additionally, our bodies break down and eliminate substances made and used within ourselves, as well as natural plant compounds. All of these processes rely on intricate systems in our bodies that metabolize and eliminate toxins.
Many people have genetic variants that impact how medications and toxicants are broken down and eliminated. Our genes make us unique, and one difference between people is seen in the differences in the phase I and phase II detoxification pathway genes.
Understanding where you have a genetic sensitivity — and then optimizing to avoid specific toxicants or drugs — is the key here.
To better understand this process, let’s first explore how phase I and phase II detoxification work. Then I’ll link to the full articles on significant genetic variants in these pathways, along with genotype reports where members will see their genes.
My hope is that by understanding how your body eliminates specific substances, such as prescription drugs and pesticide residue, you can make informed decisions about your health.
What are detoxification pathways?
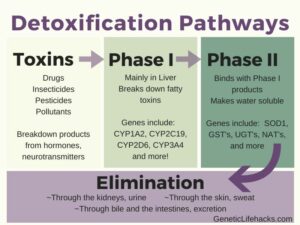
Detoxification pathways are the body’s way of metabolizing (breaking down) foreign substances and then eliminating them. This is usually a two- or three-stage process.
In a nutshell, substances need to be water soluble to be eliminated via feces and urine, and the goal of ‘detox’ is to get rid of substances that your body doesn’t want.
Phase I of detoxification involves breaking apart large toxins and converting them into polar molecules. This process is called metabolism, and the resulting substances are called metabolites.
Phase II then binds something to the metabolite from Phase I, making it water soluble and easily excretable.
Some researchers include a third phase in the process – the elimination of Phase II products (urine, feces, sweat).
Working together at the same rate:
Phase I detoxification processes often make a lipophilic (lipid soluble) substance more hydrophilic for increased solubility. This step sometimes results in a substance that is even more toxic than the original — a toxic metabolite.
Phase II processes then need to come along and remove that toxic metabolite by conjugating it with another molecule that will facilitate its elimination. If phase II processes can’t handle the load of toxic metabolites, then cell damage can occur. (DNA damage is the biggest problem because it can lead to cancer-causing mutations.)
How do phase I and phase II metabolism apply to medications or drugs?
These detoxification pathways are particularly relevant when it comes to medications or drugs. Doctors often say, “try this medication and see how it works for you”. By understanding how your genes work, you can know what is more likely to work and why a specific medication gives you side effects.
The rate at which a medication is metabolized affects how your body will react to that drug:
- Too fast, and you may not get the effect you need.
- Too slow, and you may build up too much in your body when you take the next dose.
Some medications are designed so that the metabolite – the substance created after phase I metabolism – is actually the active drug. These types of medications are called prodrugs. Phase I metabolism must take place in order for the active drug to be formed.
Note: While genetic data from services like 23andMe or AncestryDNA can provide part of the picture on medication metabolism, for a better understanding of your drug metabolism issues, your doctor may recommend getting a clinical-grade test done. This type of testing is called pharmacogenetic testing and can give a prescribing doctor a clear picture of which drugs are likely not to work well for you.
Phase I Detoxification Genes: CYP450
Many toxicants – whether ingested, inhaled, or created in our bodies – are broken down by the Cytochrome P450 (CYP450) family of enzymes in phase I detoxification. This process primarily occurs in the liver, the body’s main organ for detoxification
The CYP450 enzymes have iron and oxygen in them and, through a redox reaction, can make a drug, toxin, or endogenous substance more polar. These metabolite molecules then pass through phase II detoxification to become even more hydrophilic (water-loving) so that they can easily be eliminated. The goal of these detoxification pathways is to create molecules that the body can easily get rid of (urine, feces, sweat).
CYP450 Genetic Variants:
Genetic variants in CYP450 enzymes can significantly impact how an individual metabolizes various toxicants, medications, and substances produced within the body. Read through the article and check the genotype report. Members can start with the Detoxification Topic Report to easily see which articles are important to read first.
- CYP1A1 – metabolism of estrogen, polyaromatic hydrocarbons, and more
- CYP1A2 – metabolism of caffeine, duloxetine, bupropion, aflatoxin B, and more
- CYP2A6 – metabolism of nicotine, coumarin, and more
- CYP2B6 – metabolism of ketamine, methadone, sertraline, and more
- CYP2C9 – metabolism of warfarin, rosuvastatin, celecoxib, and more
- CYP2C19 – metabolism of clopidogrel, some proton pump inhibitors, more
- CYP2D6 – metabolism of some antidepressants, antipsychotics, more
- CYP3A4 – metabolism of half of all prescription drugs
- CYP2E1 – metabolism of fatty acids, alcohol, and some anesthetics
Phase II detoxification genes: UGT, GST, Nrf2
Phase II detoxification involves taking the metabolites of phase I and modifying them to be easily excreted.
Sometimes the metabolites of phase I are carcinogenic or reactive, so having phase II detox in sync is very important. You want to have fast and efficient phase II detoxification.
The following articles explain your genetic susceptibility variants related to phase II detoxification as well as what you can do to avoid problems here.
- UGT genes – glucuronidation, most prevalent phase II
- GST genes – glutathione
- SULT genes – sulfation reaction increases the water solubility of drugs, hormones, and xenobiotics.
- NQO1 – metabolizing benzene, quinones, air pollution
- NAT1 and NAT2 – n-acetyltrasferases, cigarette smoke, hydrocarbons
- Nrf2 Signaling Pathway
Elimination: Phase III
After a toxin passes through Phase II, it needs to be excreted from the body through urine, feces, or sweat.
Bile acids are essential in the process, as is proper kidney function. Cellular transporter proteins can also come into play here.
You can promote elimination by staying hydrated (peeing it out) and by normal bowel movements (pooping regularly).
Additionally, some substances can be eliminated through sweat, and a sauna can be beneficial for elimination.
With all of these routes of elimination, getting enough water each day is important – as is having regular bowel movements.
Detoxification pathways for specific substances:
In addition to the phase I and phase II specific genes above, the following articles look at specific toxicants and their detoxification pathways:
- Mold Genes
- Arsenic Detoxification
- BPA Detoxification
- Glyphosate Detoxification
- Organophosphate Pesticides
- Caffeine Metabolism
- Phthalate Detoxification
By learning about your genetic variants and their impact on detoxification pathways, you can take proactive steps to support your body’s natural ability to eliminate harmful substances and maintain optimal health.
Related Articles and Topics:
MTHFR and Folate:
Learn how your genes impact your need for folate. The methylation cycle relies on folate, which then impacts the detoxification of certain substances.
COMT and Supplement Interactions:
In addition to the Phase I and Phase II detoxification reactions, the COMT enzyme is affected by many popular supplements. Check your COMT variants to see if there are supplements you should be careful with.