I recently surveyed Genetic Lifehacks members to see what they were most interested in learning about. A top answer was long Covid and vaccine-related issues. In combing through the research on both topics, there is a lot of overlap in symptoms and possible mechanisms of action. Thus, I’ve combined the two topics into one article.
Writing this article reminded me repeatedly that research seems to happen in a silo. The specialists seem to look only at how their specialty applies. For example:
- Immunologists point to immune system abnormalities.
- Mast cell researchers claim that MCAS explains everything.
- Coagulation experts point to clotting dysregulation as the problem.
- Imaging specialists point to changes in fMRI pictures of the brain.
- And gut microbiome docs find that everything is due to the gut.
My goal is to present the research and then give you genetic links to why you may be more susceptible to certain outcomes. While many of the research silos seem separate, your genetic susceptibility may hold the key to determining what is causing the root of your health problems.
Heads up: This is an in-depth article, which is a nice way of saying it turned out to be, well, kinda long. Bookmark it, email it to yourself — you may want to read this one in pieces.
Premise: What do I mean by Long Spike?
Some people who have received the mRNA vaccines have long-term symptoms similar, in many ways, to the symptoms of long Covid (or post-acute sequelae of Covid-19, PASC).
Reported symptoms of the mRNA spike protein vaccines and/or long Covid include:
- brain fog
- heart rhythm issues
- tachycardia (heart rate of 100+ beats per minute)
- mast cell activation (allergy-like symptoms)
- small fiber neuropathy (tingling, pain, nerve issues)
- dysautonomia (sweating, heart rate anomalies, dizziness, low blood pressure, inability to stay upright)
- POTS (heart rate changes with sitting or standing)
- sensitivity to temperature
- reactivation of viruses (Epstein-Barr reactivation)
- fatigue, exercise intolerance
- tinnitus, hearing loss, hair loss
For the purposes of this article, I’m going to call this long Spike. I’ll include information both on long Covid as well as studies that drill down to the known effects of the spike protein.
- Is every symptom of long Covid due to the spike protein? Probably not.
- Is every symptom of a vaccine reaction due to the spike protein? I don’t know.
But… there is a lot of research on the spike protein, making it a likely culprit for much of what I’m going to call ‘long Spike’.
Before I go any further, I want to point out the obvious: the vast majority of the world’s population has been exposed to the SARS-CoV-2 spike protein through getting COVID-19 and/or being vaccinated. With billions exposed, it is unsurprising that a percentage of the population has persisting and varied symptoms.
Quantifying Long Covid (PASC):
Defining long Covid and determining the percentage of the population with it is a sticky problem, and the research numbers are all over the place. For this article, I’m going to call it long Covid, but a more scientific term is Post-Acute Sequelae of COVID-19 (PASC).
A meta-analysis found that long Covid symptoms are quite common. The analysis combined data from several studies and defined long Covid as still having fatigue or brain fog 12 weeks after infection with SARS-CoV-2. The study found that 32% of people still had fatigue, and 22% still had cognitive impairment.[ref].
There seems to be a spectrum of long Covid — from tiredness and brain fog to completely debilitating symptoms that keep someone homebound, on bed rest, and out of work.
Is long Covid real?
Going to the doctor for long Covid symptoms can often be frustrating — both for the patient and the doctor.
The compilation of odd, non-specific symptoms combined with a lack of treatment or tests makes diagnosing difficult. It leaves some doctors suggesting that long Covid is just anxiety or ‘all in their head’.
Research shows that long Covid causes significant, detectable biological changes. Hopefully, tests will be developed soon to quantify this and put the ‘all in their heads’ attitude to rest.
- A new study found that people with long Covid have alterations to their urinary metabolites that can readily be detected using a spectrometer, with test specificity at 98%.[ref]
- Trained dogs can sniff out long Covid patients due to specific volatile organic compounds in their sweat.[ref]
Moving on to the mRNA vaccines and spike protein…
SARS-CoV-2 Spike protein, mRNA:
The mRNA vaccines include instructions for cells to assemble a spike protein similar to that found in the original Covid-19 virus.
First, I’ll briefly explain mRNA and how the vaccine mRNA differs just a bit from our normal cellular mRNA. (Skip ahead if you know this stuff.)
Quick background on mRNA:
mRNA stands for messenger RNA, and it is an integral part of how cells in all living organisms work. Your genes in the cell nucleus are transcribed into messenger RNA (mRNA). The mRNA copies the nucleotide code (the A, C, G, and Ts) into a message that can turn into proteins. The mRNA also uses the nucleotides A, C, and G, but with one exception — mRNA uses U (uridine) instead of T (Thymine). The transcription of mRNA constantly happens in all the cells of your body: DNA is transcribed into mRNA, which exits the nucleus and is then translated into proteins in the cytosol of the cell.
The mRNA covid vaccines are designed to be injected into the deltoid muscle of the upper arm. The mRNA is then taken into muscle cells, which translate the mRNA into the spike protein. The cells then should display the spike protein to alert the immune system to the presence of this foreign protein. Cells making the spike protein should go through cell death (apoptosis), and the immune system is primed to recognize the spike protein when it sees it again.
The mRNA vaccines from Pfizer-BioNTech and Moderna both encode the S (spike) protein, sequenced from the original strain of SARS-CoV-2 (Wuhan-Hu-1 strain). The mRNA is packed in lipid nanoparticles, which can cross cell membranes into cells, where it is translated into the spike protein. One difference in the mRNA vaccines is that the spike protein has a synthetic uridine (U) known as pseudouridine. It is, so the immune system doesn’t initially recognize the mRNA as something that needs to be immediately destroyed. mRNA technology has decades of research behind it, and the researchers had figured out that pseudouridine results in the mRNA sticking around longer and being translated a greater number of times. In other words, the pseudouridine helps to prevent the spike protein mRNA instructions from being broken down quickly.[ref]
The mRNA is translated over and over into the spike protein, and the cells then display it for the immune system to recognize that it is a foreign protein that should be destroyed. The cell producing the spike protein is also marked to be destroyed — just like if it was infected with the virus. The subunits of the spike protein can also be released from the cell via exocytosis. “It is believed (but not systematically studied and formally shown) that muscle cells, fibroblasts, endothelial cells, and/or immune cells such as dendritic cells contribute to the expression of S after intramuscular vaccination.”[ref] Endothelial cells are the cells that line blood vessels.
Adverse reactions reported from the vaccine:
Anecdotal reports of vaccine after-effects include new onset of autoimmune diseases, MCAS, POTS, small fiber neuropathy, clotting problems, changes in menstruation, heart rhythm issues, and more. Here’s a list of over 1,000 publications on the topic. The VAERS database also records hundreds of thousands of possible adverse effects from the SARS-CoV-2 vaccines.
For example, research studies and case reports on vaccine reactions include neurological, cardiac, immunological, autoimmune, and gastrointestinal issues such as:
- Bells palsy or facial paralysis[ref][ref]
- Shingles[ref]
- Guillain Barre Syndrome[ref]
- Multifocal motor neuropathy[ref]
- Cervical Transverse Myelitis[ref]
- small fiber neuropathy[ref][ref]
- Clotting issues[ref]
- myocarditis and pericarditis
- hemorrhagic stroke[ref]
- menstrual irregularities[ref]
- tinnitus[ref][ref]
- sudden hearing loss[ref]
- myasthenia gravis[ref]
Some adverse side effects, such as Guillain Barre syndrome or cervical transverse myelitis, are rare (1 in a million) and can happen with other vaccines.
While other side effects, such as menstrual irregularities, are more common. Menstrual irregularities after the mRNA vaccines were reported by 40% of women in one large study of women aged 18-40.[ref]
One difference to keep in mind with this current pandemic is simply that the sheer number of adults getting vaccinated all at once will make adverse events more common. Besides occasional tetanus or flu shot, most adults aren’t getting vaccines regularly.
Are the adverse effects of the vaccine due to the spike protein?
I’m not the only one who has noticed the big overlap in symptoms of long Covid and the symptoms post-vaccination with the mRNA vaccines. Plus, the obvious commonality of the spike protein.
A study published in Cell in July 2022 explains that “we surmise that vaccination-mediated adverse effects (AEs) can be attributed to the unique characteristics of the S protein itself (antigen) either due to molecular mimicry with human proteins or as an ACE2 ligand.”[ref]
The mRNA vaccine was assumed to stay in the muscle where it is injected, but that doesn’t seem to be the case – at least not for everyone. “The anti-SARS-CoV-2 vaccine mRNA-containing LNPs are injected into the deltoid muscle and exert an effect in the muscle tissue itself, the lymphatic system, and the spleen, but can also localize in the liver and other tissues… from where the S protein or its subunits/peptide fragments may enter the circulation and distribute throughout the body.”[ref]
Does vaccination prevent long Covid – or – does vaccination make long Covid more likely?
While a provocative question, a large study shows neither seems to be the case.
A study looking at ~10,000 vaccinated people who got Covid compared the results to a similar number of unvaccinated age, weight, and sex-matched controls. The risk of “long Covid features” was reported to be the same for vaccinated and unvaccinated. Digging into the details shows a slightly nuanced difference. Table A13 in the appendix shows that the hazard ratio for hypertension and hyperlipidemia was statistically higher in the vaccinated participants. Additionally, the risk of anxiety disorders and abdominal symptoms (20% higher) was statistically elevated for study participants who had gotten covid within a couple of months of vaccination. After four months, the negative impacts of the vaccine disappeared.[ref]
Theories and research on long Spike:
Several pathways are being researched for long Covid / long Spike.
To keep this organized, I’m going to group the research into possible causes and possible effects with long Spike.
1) Possible causes:
- Persistence of the virus and/or spike protein
- Gut microbiome interactions
- Damage to organs, including the heart and endothelium
- Damage to the blood-brain barrier and activation of microglia
- Damage to the intestinal epithelial barrier
- Interaction with nerve receptors
2) Possible effects / results:
- MCAS, POTS
- Clotting (microclots, cerebral blood flow disruption)
- small fiber neuropathy
- Chronic fatigue
- Cognitive dysfunction and mood changes
- Autoimmune diseases
The terms “causes” and “effects” aren’t totally accurate here, but what I’m hoping to get across is that the various symptoms, whether grouped as dysautonomia, small fiber neuropathy, or autoimmune, are likely a result of something that the spike protein did in the body.
1) Causes of Damage:
First, let’s dig into the research studies on possible causes of damage or continued change going on after exposure to the spike protein.
Let me make it clear: When a cell is infected, whether through nanoparticles bringing in the spike protein mRNA or by the virus, the response of the immune system is to kill that cell. As one study on vaccines puts it: “In conclusion, it is essential to underline that every human cell that intakes the LNPs and translates the viral protein (in case of the mRNA vaccines), or that gets infected by the adenovirus and expresses and translates the viral protein (in case of the adenovirus-based vaccines), is inevitably recognized as a threat by the immune system and killed… There are no exceptions to this mechanism. ” [ref]
Viral persistence and/or spike protein persistence
I tend to think of viral illnesses as coming into contact with the virus, developing symptoms days later, and then returning to normal when the immune system has fought it off.
That simplified view misses the boat regarding a lot of viral illnesses. For example, you get chicken pox and then recover back to normal in a week or so. But that chicken pox virus, the varicella-zoster virus, lies dormant for decades in the nerves, only to reactivate in times of stress to cause shingles. Other viruses that can lie dormant and then reactivate include human herpesviruses, Epstein-Barr virus (mono), and adenoviruses. And then some viruses just stick around, like the herpes virus that causes cold sores or viruses that cause warts.[ref]
For people with long Covid, some research shows that the virus is still present in their system. One pre-print states: “Strikingly, we detect SARS-CoV-2 spike antigen in a majority of PASC [long Covid] patients up to 12 months post-diagnosis, suggesting the presence of an active, persistent SARS-CoV-2 viral reservoir. Furthermore, temporal antigen profiles for many patients show the presence of spike at multiple time points over several months, highlighting the potential utility of the SARS-CoV-2 full spike protein as a biomarker for PASC.”[ref]
Important to note here – the researchers claim that some of the presence of spike protein could be due to vaccinations after Covid, but they assumed that this is only for the first two weeks after vaccination. Other research studies show that the mRNA vaccine can stick around much longer. To me, this study doesn’t do enough to differentiate whether the spike protein is from SARS-CoV-2 or the vaccine. But, perhaps it doesn’t matter.
Other peer-reviewed published papers also show prolonged viral shedding is possible.
- One case study in an elderly man showed that he was shedding the virus and testing positive with PCR tests for 97 days after the onset of symptoms. Tests showed that he had a low T-cell response to the virus.[ref]
- A large study found viral shedding in nasopharyngeal tests for 28 days on average, but the results showed that about 10% of participants were still PCR-positive for the virus at 60 days (length of the study).[ref]
While a lot of the initial information about Covid described it as a respiratory disease, autopsies show that the virus infects many tissues in the body. The NIH and NIAID did a series of autopsies on Covid patients. The doctors found that the virus infected cells in the heart, lymphatic system, intestines, kidney, reproductive tissues, muscle, peripheral nerves, fat cells, skin, eyes, and brain. The spike protein RNA was also found throughout the body.[ref]
T cells specific to COVID-19 persist in people with long Covid. One study showed that long Covid participants had “between 6- and 105-fold higher frequencies of IFN-γ- and TNF-α-producing SARS-CoV-2-specific CD4+ and CD8+ T cells in peripheral blood, and elevated levels of plasma CRP and IL-6.”[ref]
Switching back to the spike mRNA vaccines:
You may wonder, as I was, whether longer-term adverse events after vaccination could also be due to the persistence of the spike protein. The answer to that seems to be a solid ‘maybe’… It really surprised me since most mRNA produced naturally in cells is broken down in minutes.[ref]
A study published in the journal Cell showed that the mRNA for the spike protein persisted in some vaccine recipients for 60 days in the lymphatic tissue. The study found that nearly everyone produced circulating spike protein for 1-2 days after vaccination, and half of the people were still producing spike protein on day 21. Intriguingly, the researchers still found mRNA in the lymphatic cells were still producing spike protein at day 60 for a minority of people.[ref] Note that the end of the study was at 60 days, so it is unknown if the mRNA persisted in anyone longer than 60 days.
Gut and Microbiome Impact and Changes:
Changes to the gut microbiome can affect the body in many ways – from the gut-brain axis changing neurotransmitters to the altered microbiome heightening overall immune response.
It has been known since very early on in the pandemic that SARS-CoV-2 could infect more than just the lungs. Using the ACE2 receptor, the virus can infect many cell types, including intestinal cells. It can replicate in the intestinal cells and cause diarrhea. While most people have respiratory symptoms with COVID-19, intestinal symptoms are predominant for some.
Even without intestinal symptoms, the SARS-CoV-2 virus can replicate in the gut.
SARS-CoV-2 can persist in fecal samples a long time after nasal swabs are negative. For most people, the persisting fecal shedding is a week or two post-nasal swab being negative. But some outliers still produce SARS-CoV-2 in their poop 25 to 40 days after getting the virus.[ref]
Is SARS-CoV-2 acting as a bacteriophage and replicating in the gut bacteria?
Viruses cannot replicate on their own. They have to hijack the host’s cellular replication mechanisms to replicate. Thus, you can’t usually grow viruses in a petri dish without host cells (e.g., human cells for SARS-CoV-2).
Bacteriophage is the term given to viruses that can infect and replicate in bacteria or archaea.
Interestingly, a microbiology study found that the SARS-CoV-2 virus can replicate in fecal bacteria samples that contain no human cells. A fecal sample used from someone positive for SARS-CoV-2 and kept in a broth that supported the bacteria also supported the continued replication of the virus. Taking a fecal sample from a person without SARS-CoV-2 (no virus found) and then crossing it with a sample from someone who was positive showed that the virus could grow in the new fecal sample as well. The researchers went one step further and tested the ability of the virus to grow in fecal samples after administering antibiotics. They tested 18 different antibiotics and found that a couple were able to stop the virus from replicating in the fecal samples. The effective antibiotics included metronidazole, vancomycin, amoxicillin, and azithromycin. (This would indicate that bacterial species that are killed by those specific vaccines are responsible for the replication of SARS-CoV-2) Microscope imaging of the bacteria shows that they are replicating SARS-CoV-2.[ref]
You may wonder if bacteria can take in the mRNA from the vaccine and generate the spike protein. It is a question I can’t find an answer to, leading me to think it cannot happen.
Bacteria can be used to produce RNA products in the lab or in bioreactors. E. coli is one bacteria that is commonly used for this purpose.[ref]. In fact, researchers found that E. coli could be used to replicate the spike protein’s receptor-binding domain (RBD). The research on this was geared towards being able to use E. coli to replicate the spike protein for a vaccine. But, to do this, researchers needed to combine the RBD with another protein’s RNA.[ref].
Microbiome and mRNA vaccines:
Gut microbiome influences antibody response:
The gut microbiome composition influenced the immune response to the covid vaccines (both the inactivated vaccine and the Pfizer mRNA vaccine). Higher levels of Bifidobacterium adolescentis were linked to higher neutralizing antibodies in people receiving the CornanaVac vaccine. For the Pfizer vaccine, higher neutralizing antibodies (e.g., a greater immune reaction to the vaccine) were found to correlate with the abundance of gut bacteria with flagella and fimbriae (e.g., Roseburia faecis). Interestingly, adverse events were lower in people with an abundance of Prevotella or Megamonas species. So what is going on here? Some gut microbiome species modulate our human immune response, and the gut microbiome also impacts other vaccine responses. B. adolescentis is also associated with CD4+ T cell response to other vaccines.[ref]
Changes in the oral microbiome:
A Japanese study involving 40 participants found changes in the oral microbiome composition after vaccination with the Covid mRNA vaccines.[ref] Perhaps this has to do with changes to the host immune system.
Changes in the intestines post-vaccination:
Inflammatory Bowel Diseases (IBD) include Crohn’s disease and ulcerative colitis. IBD patients have been studied to see how they react to mRNA vaccines, initially to see if the immunosuppressant drugs would make the vaccines less effective. If the mRNA vaccine changes anything in the gut, these IBD patients should be a canary in the coal mine.
A study involving IBD patients in Vienna found that the mRNA vaccines increased the biomarker used for monitoring intestinal inflammation (fecal calprotectin). Of the patients in remission before the vaccination, about 10% had an IBD-related adverse event after the vaccine. The trial results showed that the fecal calprotectin levels were significantly higher in IBD patients, but only after the second dose of the mRNA vaccine. The researchers concluded that the probable underlying mechanism was “a transient mRNA vaccine-induced intestinal expression of the spike protein with consecutive down-regulation of ACE2”.[ref]
Interesting to note here is that SARS-CoV-2 infection also is associated with fecal calprotectin levels.[ref]
A survey of over 3,000 IBD patients found that 51% had systemic symptoms after the first dose of the vaccine. However, only ~4% needed medical help with the systemic reactions, which is comparable to what is found in the general population.[ref]
Gut microbiome and long Covid:
A study published in the journal Gut revealed that patients with long Covid (PACS) had significant differences in their gut microbiomes six months after Covid compared to a control group. The long Covid patients had higher levels of certain bacterial species and lower levels of butyrate-producing bacteria, such as Bifidobacteria species.[ref] A follow-up letter to the editor of the journal Gut was just published for this study. The study authors kept monitoring the long Covid patients, and the gut dysbiosis continued for 14 months.[ref]
If the gut microbiome makes all the difference, can probiotics prevent getting long Covid?
One study showed just that. A small clinical trial showed that taking probiotics right after being discharged from the hospital for covid prevented long covid symptoms, such as fatigue. The study concluded, “Our results strongly suggest that in COVID-19, the administration of probiotics during hospitalization may prevent the development of chronic fatigue by impacting key metabolites involved in the utilization of glucose as well as energy pathways.”[ref]
A larger study used strains of Lactiplantibacillus plantarum in a randomized placebo-controlled trial with almost 300 covid patients. The results showed complete remission in 53% of the probiotic group compared to 28% of the placebo group. The trial lasted 30 days, and patients in the probiotic arm had significantly lower nasopharyngeal viral loads on days 15 and 30 compared to the placebo group.[ref]
What about other viruses in the gut? We talk about probiotics and gut microbes with a focus on bacteria in the gut. But the gut microbiome also contains resident viruses as well. A 2021 study found over 100,000 different viruses that live in the gut. These are mainly DNA viruses (SARS-CoV-2 is an RNA virus), and they are bacteriophages that infect bacteria or archaea.
A study on patients with Covid-19 found differences in the types of viruses found in the gut of people who got sick with Covid.[ref]
Quick aside: After all the info on SARS-CoV-2 in the gut, you may wonder if it is replicating in wastewater treatment plants. (OK, you may not be wondering that, but I was…)
The SARS-CoV-2 virus is found in wastewater treatment plants where the virus is circulating, and sampling wastewater is one way that officials determine how prevalent the virus is in an area. A study on wastewater treatment plans showed that treating the sludge with chlorination kills the virus. But in untreated sludge, the virus was present.[ref] Active chemical or UV treatment is needed to eliminate the virus in wastewater treatment plant effluence.[ref]
Damage to the endothelium:
The lining of your lymph and blood vessels is called the endothelium. Once thought just to be a layer of cells that keep your blood contained, more recently, the endothelium has been shown to have important properties, and some now consider it an organ system.[ref]
ACE2 receptors, to which the spike protein binds, are found on endothelial cells. The surface-bound ACE2 is important in how the renin-angiotensin system regulates blood pressure.
The spike protein binding to the endothelial cells in small blood vessels causes damage due to the induced immune response. Inflammation in the endothelial cells causes either cell death or cellular senescence. Studies with the spike protein alone showed increased cellular senescence also.[ref][ref] Senescent cells can no longer replicate, and they secrete inflammatory cytokines to signal to the immune system that they need to be destroyed. When there are too many senescent cells, the immune system can’t clear them all out. The senescent cells then affect surrounding cells through the secreted inflammatory cytokines.
The binding of the spike protein to ACE2 on endothelial cells also activates the NLRP3 inflammasome, exacerbating the inflammatory response and leading to cell death.[ref] Read more about the NLP3 inflammasome and check your genes.)
Damage to the heart: myocarditis
Myocarditis is a heart muscle inflammation triggered by a virus, bacteria, protozoan infection, immune reaction, an autoimmune condition, drug reaction, arsenic, or vaccination. In the acute phase of myocarditis, damage to the heart muscle causes apoptosis (cell death) and damage to tissues from the immune response.[ref][ref]
Myocarditis rates for males aged 16-40 after vaccination are reported to be somewhere between 1 in 2,700 to 1 in 5,000, depending on the country’s data used.[ref][ref]
A recent peer-reviewed study in adolescents looked at heart tests (ECG, echocardiograms, cardiac enzymes) before taking the mRNA vaccine and after. The results showed that 29% of the adolescents had cardiovascular changes, such as tachycardia or palpitations, after the vaccine. 2% of the participants had either clinical or subclinical myocarditis or pericarditis.[ref]
A recent animal study showed that the intravenous injection of the mRNA vaccine caused myocarditis much more quickly than the intramuscular injection, which took two doses of the vaccine. The myocarditis in the animals showed that the spike protein was sometimes expressed in the cardiac muscle cells but was more often found in the infiltrating immune cells. This result is similar to the Pfizer study showing that there is some (low) accumulation of the mRNA vaccine in the heart, but at lower rates than in the liver or spleen.
The researchers also note that the size of the lipid nanoparticles of the mRNA vaccines is such that they could be sucked into the T tubules in the cardiac muscle cells but not into the tiny T tubules in skeletal muscle. “Moreover, smaller mRNA-vaccine lipid-nanoparticles(100nm diameter) can be sucked into larger T tubules (diameter >200 nm) of cardiomyocytes during diastole, but not into T tubules of skeletal myocyte (diameter 20–40 nm)… Thus, the T tubule system of cardiomyocytes may concentrate mRNA-vaccine lipid-nanoparticles like a sponge.”[ref]
Viral infections, including the SARS-CoV-2 virus, can also cause myocarditis. In the case of viral infections, the virus infiltrates the heart tissue, usually from immune system cells. For SARS-CoV-2, the virus enters the heart muscle tissue via the ACE2 receptor, replicating there and causing the immune cells to kill off the heart muscle cells (apoptosis).[ref][ref]
Neuroinflammation, damage to the blood-brain barrier
A common thread among symptoms reported for long Spike is neurocognitive changes. Whether you call it brain fog, memory loss, neurocognitive deficits, or simply an inability to think… it all adds up to something going on in the brain.
Researchers looked at a group of 205 long Covid patients who were previously healthy, working younger adults. The long Covid participants underwent a comprehensive panel of tests (cardiac MRI, pulmonary CT scans, lung function, cognitive scans, CPET, and more). Essentially, these patients were tested for everything that could be relevant. The results showed that the only significant changes were in cognitive function. Everything else was fairly normal or mildly changed (a third still had slightly reduced lung function).[ref]
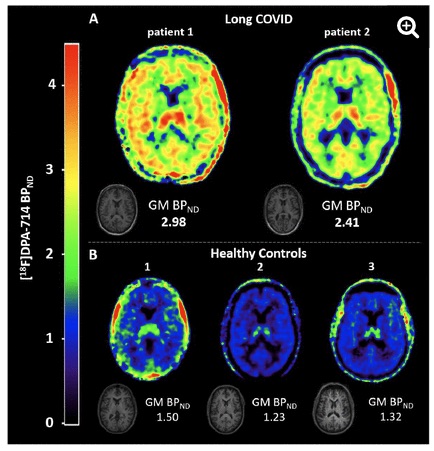
What is going on in the brain?
A small study (pre-print) looked at PET scan images of the brains of people suffering from long Covid. The results showed that the “extent of neuroinflammation was remarkable”.[ref].
Here is an MRI image showing the inflammation in the long Covid brains compared to normal controls:[ref]
Researchers published a study early on in the pandemic showing that the spike protein may be able to decrease barrier integrity in the blood-brain barrier.[ref]
Subsequent research backed that up with studies showing the spike protein could enter the brain through ACE2 endothelial cells, and that SARS-CoV-2 infection increased permeability of the blood-brain barrier.[ref][ref] Additionally, researchers found that the spike protein could bind to ACE2 in the blood vessels in the brain.[ref]
Microglia are a special type of cell in the brain that are the main form of immune defense in the central nervous system. Research shows that microglia take up the spike protein and other exosomes from SARS-CoV-2. This absorption causes hyperactivation of the microglia.[ref]
Interestingly, HSP90 (heat shock protein 90) inhibitors may block and repair spike protein-induced endothelial barrier dysfunction.[ref]. EGCG (the major catechin in tea) is a natural HSP90 inhibitor.[ref]
Interaction with specific nerve receptors (theoretical)
Very early on in 2020, it was noticed that being a smoker significantly reduced the risk of getting SARS-CoV-2. This flies in the face of what you would think would happen to smokers with a respiratory disease. But multiple epidemiological studies clearly showed that moderate or heavy smoking was protective.[ref]
This significant decrease in risk for smokers led researchers to figure out why nicotine was protective against SARS-CoV-2. Nicotine binds to nicotinic acetylcholine receptors (nAChRs) in the brain and throughout the body. When nicotine binds to the nAChRs, it blocks other substances, such as acetylcholine, from binding to it.
Acetylcholine is a neurotransmitter, and its actions are completed through binding to various types of acetylcholine receptors. For example, acetylcholine binding to nicotinic acetycholine receptors is involved in muscle movement. The nAChRs are also found in the peripheral and central nervous systems (e.g. in the brain).
One more place that nicotinic acetylcholine receptors are found is in the immune system in B cells, T cells, and macrophages. A specific subtype of nAChR, called the α7-nicotinic acetylcholine receptor, is involved in the regulation of the inflammatory response via the vagus nerve and immune cells. Alpha 7 nAChRs are also expressed in endothelial cells lining the blood vessels as well as bronchial epithelial cells lining the lungs. Additionally, α7-nAChRs affect mast cells and dendritic cells. For example, nicotine binding to nAChRs on mast cells causes mast cell degranulation.[ref]
I mentioned above that nicotine binds to the nAChRs, but other substances, such as nerve gas and toxins, can also bind to the receptors and block them. For example, the toxin produced by the poison dart frog binds to nAChRs and causes muscle paralysis.
Researchers have found that a receptor-binding domain on the spike protein in SARS-CoV-2 has a toxin-like sequence that could bind to the nAChRs. Binding to the α7 nAChR would cause disruption of the regulation of the immune response (such as is seen in severe Covid). [ref]
More recent research shows that the spike protein is an antagonist of the α7 nAChR.[ref] Studies in monkeys show that an agonist of α7 nAChR reduces SARS-CoV-2 infectivity and disease progression. An agonist binding to the acetylcholine receptor stabilizes it and desensitizes it. An antagonist, such as a toxin-like substance, blocks acetylcholine from binding to α7-nAChR.
While all of this research on the spike protein binding to the α7-nAChR as an antagonist is interesting and theoretically ties together mast cells, nerve issues, immune dysfunction, and endothelial problems, a lot more research is needed to really know if this is what is happening in the body on a large scale.
2) Effects of the Spike Protein:
Moving into the persisting effects of the spike protein…
Mast Cell Activation Syndrome and Long Spike:
Mast cells are part of the immune system. They are located in the skin, the lung, nose, and intestinal mucosa, along nerves, and generally in areas where allergens or pathogens can be present. Mast cells are traditionally thought of in terms of allergic reactions since they degranulate and dump out a lot of histamine and inflammatory substances when activated in an allergic reaction.
A recent study showed that the spike protein could bind to the ACE2 receptor on mast cells and cause degranulation.[ref]
Another study shows that histamine potentiates the interaction with the spike protein and the ACE2 receptor in epithelial cells (cells that line the blood vessels).[ref]
Mast cell activation syndrome (MCAS) is a chronic multisystem disorder with chronic activation of mast cells. Symptoms can include hives, itching, anaphylaxis, low blood pressure, rapid heart rate, headache, brain fog, fatigue, abdominal pain, diarrhea, and more. Symptoms of MCAS are very common in long Covid patients.[ref]
Interestingly, hospitals very early in the pandemic noticed that an antihistamine (H2 blocker, famotidine) was linked to better patient outcomes.[ref]
Animal studies also showed that antihistamines, along with antiviral drugs, work as a therapy for Covid-19.[ref]
In a study in mice, researchers found that retroviruses in the intestines can trigger mast cell activation for degranulation. It then activated other cell types that inhibited CD8+ T cells and natural killer cells, thus allowing for continued viral replication in the intestines.[ref]
Another recent study showed the gut microbiome to be very important in histamine/mast cell problems. The study found that histamine produced by the gut microbiome becomes systemic and can cause visceral hypersensitivity (e.g., pain) due to activating histamine receptors. Additionally, mast cells accumulate in the colon.[ref] While not specific to long Spike, the study raises a possible mechanism when combined with the changes to the gut microbiome.
Additionally, mast cells are located in areas surrounding the neurons. Activation of mast cells is thought to be a part of neurodegenerative disorders.[ref]
Blocking histamine receptors:
A study on long Covid patients found they had reduced CD4+ and CD8+ effector memory cells. The study found that 72% of patients who received H1/H2 combined antihistamine therapy had clinical improvements after four weeks.[ref] H1 antihistamines include loratadine 10 mg twice a day or fexofenadine 180 mg two times per day. H2 antihistamines include famotidine 40 mg once daily or nizatidine (prescription) 300 mg once a day.[ref]
Positive role of mast cells:
It is important to point out that mast cells are activated for a reason, and there must be a positive benefit here. The key may be in the response of mast cells to thrombin, which is the enzyme that helps blood clots form by converting fibrinogen to fibrin.
Animal studies show that mast cell activation also plays a role in modulating, or tamping down, the inflammatory response to thrombin. In animals that lack mast cells, thrombin produces a much greater inflammatory response.[ref]
While there isn’t research specifically showing this, it makes sense that mast cells would be activated by any endothelial dysfunction and increased clotting due to the spike protein.
It nicely transitions us into talking about clotting problems…
Microclots and Clotting Issues:
Researchers looked at the clotting ability in long Covid patients by investigating platelet-poor plasma. The platelets were removed from plasma because they are the normal way of creating clots.
The researchers found that in long Covid patients, an odd type of clotting was occurring. The authors state: “we discovered that fibrinogen in blood can clot into an anomalous ‘amyloid’ form of fibrin that (like other β-rich amyloids and prions) is relatively resistant to proteolysis (fibrinolysis). The result, as is strongly manifested in platelet-poor plasma (PPP) of individuals with Long COVID, is extensive fibrin amyloid microclots that can persist, can entrap other proteins, and may lead to the production of various autoantibodies.”
The researchers theorize that the symptoms of long Covid are caused by fibrin amyloid microclots blocking capillaries (small blood vessels). The blocked capillaries then limit oxygen to different tissues.[ref].
Amyloid fibrinogen clotting isn’t unique to the spike protein or SARS-CoV-2. Research from 2016 shows that fibrinogen can form an amyloid protein structure when exposed to certain substances, including lipopolysaccharides found on some bacterial pathogens.[ref]
Recently, researchers have looked at the formation of microclots in relation to COVID-19 and the spike protein.
- One study (still in pre-print) found that the spike protein causes abnormal, amyloidogenic clotting in normal blood. This clotting initiated the formation of antibodies towards fibrinogen, which persisted “long after the acute infection”.[ref]
- Another research paper explains: “Although the symptoms of Long COVID are multifarious, we here argue that the ability of these fibrin amyloid microclots (fibrinaloids) to block up capillaries, and thus to limit the passage of red blood cells and hence O2 exchange, can underpin the majority of these symptoms.” The symptoms included here are fatigue, brain fog, and muscle pain.[ref]
- A paper published in August 2022 showed that all of the long Covid patients in the study had fibrin amyloid microclots. These patients also were more likely to have comorbidities of high cholesterol, hypertension, cardiovascular disease, and type 2 diabetes.[ref]
Lp(a): An additional link to clotting post-Covid is found with lipoprotein(a). Lipoprotein(a) levels are highly genetic. Researchers theorize that “subjects with either baseline elevated Lp(a) or those who have an increase following COVID-19 infection, or both, may be at very high risk of developing thromboses. Elevated Lp(a) may also lead to acute destabilization of preexisting but quiescent atherosclerotic plaques, which might induce acute myocardial infarction and stroke.”[ref]
Another study looking at hypercoagulability in Covid-19 patients found that Lp(a) levels increased in hospitalized patients. In those patients with higher Lp(a) levels, over half experienced a venous thromboembolism (blood clot) event.[ref]
Lipoprotein(a) levels are strongly influenced by genetic variants. I’ll list a couple of the important ones in the genetics section below.
I’m not sure that microclots explain all the symptoms of long Spike. Instead, for some people with long Spike, the nervous system seems to be driving the symptoms. So let’s take a look at autonomic disorders:
Small fiber neuropathy with long Spike:
Small fiber neuropathy (SFN) is described as a structural anomaly of small nerve fibers along with degeneration of the nerve endings. It is diagnosed by a skin biopsy examining the tiniest nerve fibers. The biopsy can show fewer than normal small nerve fibers in the skin, indicating nerve damage.[ref][ref]
Symptoms of small fiber neuropathy often start with odd sensations in the feet or hands. Some people say ‘pins and needles’; others compare it to ants biting or itchiness. It can progress up the legs and arms and then throughout the body. The abnormal activation of these nerves can cause pain, diffuse sensations, and itching.
Small fiber neuropathy can also cause abnormal activation of autonomic nervous system functions like those in the heart, gastrointestinal tract, or bladder. Fatigue is common in SFN, which is thought to be due to cardiac-related issues.[ref]
Studies on SFN in Covid show:
- A study involving 23 patients who had recovered from Covid showed that 91% had changes to the cornea consistent with small fiber neuropathy. Nerves in the cornea express ACE2 receptors as well as other receptors that the SARS-CoV-2 virus can use for entry. Alteration in the corneal nerves can cause sensitivity, pain, and dry eyes.[ref]
- The Mayo Clinic published a study in April of 2021 showing that autonomic dysfunction could follow Covid infections. Among other findings, the study showed that COVID-19 exacerbated small fiber neuropathy in people who already had it.[ref]
- Mt. Sinai also published a study showing small fiber neuropathy developing in patients after COVID-19.[ref]
- Another study from Mass General showed new onset small-fiber neuropathy in patients with long Covid.[ref]
- A case study from September 2020 explained a patient who had previously dealt with Lyme disease. After COVID, the patient developed orthostatic intolerance and small fiber neuropathy, which responded to intravenous immunoglobulin therapy.[ref]
Small fiber neuropathy after Covid vaccination:
- An observational study of 23 people with neuropathic symptoms after a Covid vaccine found that >50% met the criteria for new onset SFN (biopsy, symptoms).[ref]
- A case study published in April 2021 outlines the reaction of a 57-year-old woman who developed small fiber neuropathy a week after the Pfizer mRNA vaccine. Antibody testing ruled out a prior covid infection, and she was not on any medications nor an alcoholic. Her symptoms included burning and tingling in the extremities, loss of pinprick, and cold sensations in her feet. The biopsy confirmed the small fiber neuropathy.[ref]
- An investigation published in April 2021 that looked at immune-mediated disease flare-ups after the COVID-19 vaccines showed that flare-ups affected 78% of patients with autoimmune diseases. This investigation included autoimmune diseases that cause small fiber neuropathy.[ref]
I would like to point out that SFN can be triggered by other viruses and vaccinations, also. It isn’t unique to SARS-CoV-2 or the spike protein.
POTS: Autonomic dysfunction
POTS (postural orthostatic tachycardia syndrome) is a problem with how your autonomic nervous system regulates heart rate. Many people are reporting POTS symptoms after COVID or spike protein exposure.[ref]
Doctors define POTS as:
- an increase of heart rate of 30 BPM (beats per minute) within the first 10 minutes of standing
- Or an increase of heart rate to over 120 BMP within the first 10 minutes of standing[ref]
Dysautonomia is a term you will often see when reading about POTS. Essentially, dysautonomia means a dysfunction of the autonomic nervous system. It is a catch-all term, with several chronic conditions under the umbrella of dysautonomia.[ref]
The autonomic nervous system controls involuntary bodily functions – including heart rate, blood pressure, and the motility of the digestive tract.
Researchers are now calling the onset of POTs after Covid “Post-Covid-19 Tachycardia Syndrome”. One hypothesis as to the cause is that there may be lower blood volume due to disturbances in the rein-angiotensin-aldosterone system (RAAS). It could be due to the spike protein binding to and down-regulating the ACE2 receptor, which then could cause a RAAS imbalance. Another option is that POTS could be due to an autoimmune or inflammatory system disorder.[ref]
Case studies also show that new onset of POTS can follow the mRNA vaccines.[ref][ref]
Autoimmune Diseases triggered by Covid or spike:
Autoimmune diseases are caused by the immune system mistakenly targeting normal cells. Antibodies or T cells that react with a normal ‘self’ protein are actually thought to be present in all people, but in autoimmune diseases, there is an excess that causes tissue damage. Autoimmune diseases include type 1 diabetes, Hashimoto’s, Sjorgren syndrome, rheumatoid arthritis, and multiple sclerosis.
Autoimmune diseases linked to SARS-CoV-2 include Guillain-Barre syndrome, autoimmune hemolytic anemia, immune thrombocytopenic purpura, lupus, and Kawasaki disease.[ref][ref]
Similarly, the new onset of autoimmune diseases has been associated with mRNA vaccines. For example, immune thrombotic thrombocytopenia, autoimmune liver disease, Guillain-Barré syndrome, IgA nephropathy, rheumatoid arthritis, and systemic lupus erythematosus have been associated with the vaccines.[ref][ref]
Is the onset of autoimmune diseases new to Covid or the mRNA vaccines? No. Viruses and vaccines have long been known to trigger autoimmune diseases.[ref]
Kynurenine pathway in Long Covid Brain Fog
One final pathway to go down in this long Spike journey…
Tryptophan, an amino acid found in many protein-rich foods, can be converted into serotonin or kynurenine. If tryptophan is converted into kynurenine, it can take several routes, the most common of which involves conversion to quinolinic acid.
Quinolinic acid is the precursor for the body to produce niacin, which is essential for cellular energy. But quinolinic acid is also neurotoxic, so if there is too much or it hangs around too long, there can be negative consequences to cognitive function or mood.
A recent pre-print explains a study on cognition after mild SARS-CoV-2 infection in an unvaccinated population. The study of 128 people assessed them at 2, 4, and 12 months after Covid. The results showed mild to moderate cognitive impairment, often termed ‘brain fog’, in up to a quarter of the participants. The researchers found that kynurenine pathway metabolites, including quinolinic acid, were elevated in participants with cognitive impairment. The conclusion was that the association suggested “a potential causal link thereby indicating it as a biomarker and therapeutic target”.[ref]
Know someone with long Spike? Share this article!
![]()
![]()
![]()
![]()
Genetic variants possibly related to long Spike:
This section is usually where I would list lots of genetic variants that researchers have definitively tied to the topic of an article. However, there isn’t a lot of solid research on genetics and long Covid or vaccine-related side effects.
Instead, I will include the genetic overviews from articles related to the above causes and effects.
One theory of mine – and I could be totally wrong – is that genetic susceptibility to certain symptoms drives the varied results of long Spike.
For example, someone with the genetic risk factors for small fiber neuropathy may go down that path when exposed to the spike protein. Another person with the genetic risk factors for histamine intolerance or mast cell activation may end up with problems related to mast cell activation syndrome. A person with either existing vascular issues or is genetically prone to clotting may have clot-related problems. Someone prone to autoimmune diseases may end up with new-onset autoimmune issues.
This section is best viewed as a Genetic Lifehacks member.
Not a member? Join here. Membership lets you see your data right in each article and also gives you access to the member’s information in the Lifehacks sections.
Brain fog root causes
One of the most common symptoms reported in long Spike is brain fog or the inability to think and remember things clearly. If you have brain fog and several of the variants below, read through the full article on brain fog for more in-depth information and references.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| FGA | rs121909612 | A | -- | possibly carrier of a rare mutation related to fibrinogen amyloidosis |
| SERPINF | rs8074026 | T | -- | increase venous clotting risk, reduced breakdown of microclots |
| GPX1 | rs1050450 | A | -- | increased risk of brain fog in Long Covid patients |
| GSTM1 | rs366631 | A | -- | A/A: deletion (null) GSTM1 gene. more common genotype in people with Long Covid brain fog |
| TLR4 | rs10759931 | G | -- | G/G: common genotype, more likely to have poor cognitive outcomes from mild-Covid |
| HFE | rs1800562 | A | -- | C282Y variant, most common cause of hereditary hemochromatosis, iron buildup could cause brain fog |
| HFE | rs1799945 | G | -- | higher iron levels, more of a problem if two copies (GG) or if combined with C282Y |
Small Fiber Neuropathy Genes
Small fiber neuropathy can cause both tingling/pain nerve sensations as well as autonomic dysfunction (heart rate changes, sweating). Read the full article on small fiber neuropathy for details and references.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| SCN9A | rs6746030 | A | -- | increased risk of arthritis pain, back pain (lumbar disc), and phantom pain |
| SCN9A | rs4369876 | A | -- | More sensitive to pain, increased risk of small fiber neuropathy |
| SCN9A | rs74449889 | G | -- | Increased risk of neuropathic pain |
| SCN9A | rs80356470 | T | -- | (rare) primary erythromelalgia |
| SCN9A | rs182650126 | C | -- | (rare) increased risk of neuropathy pain |
| SCN10A | rs6795970 | A | -- | Higher pain threshhold; decreased pain in inflammatory bowel disease |
| SCN10A | rs12632942 | G | -- | GG: lower pain threshold |
| SCN10A | rs151090729 | T | -- | (rare mutation) hyperexcitable NaV1.8; increased risk of small fiber neuropathy |
| SCN11A | rs138607170 | A | -- | (rare mutation) familial episodic pain syndrome, hereditary autonomic neuropathy |
| SCN11A | rs483352921 | C | -- | (rare mutation) familial episodic pain syndrome |
| SCN11A | rs483352920 | G | -- | (rare mutation) congenital insensitivity to pain |
| SCN11A | rs141686175 | G | -- | (rare mutation) increased nerve firing, pain and neuropathy |
| TRPV1 | rs8065080 | C | -- | C/C: higher pain tolerance to pinprick pain (in Asian populations) |
MCAS Genes
People commonly report mast cell activation syndrome (MCAS) symptoms with long Spike, possibly due to the spike protein binding to and activating mast cells. Read the article on mast cell activation for details and references.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| KIT | i5007903 | T | -- | KIT D816V mutation (see article for caveats) |
| KIT | rs121913507 | T | -- | KIT D816V mutation (see article for caveats) |
| IL-13 | rs1800925 | T | -- | Increased risk of systemic mastocytosis, rhinitis, asthma |
| IL4R | rs1801275 | A | -- | better prognosis in systemic mastocytosis |
| FCER1A | rs2298805 | A | -- | Decreased risk of hives, lower IgE response |
| FCER1A | rs2251746 | C | -- | Decreased IgE response |
| FCER1A | rs2427827 | T | -- | Increased IgE, increase sinus problems, allergic reactions |
| CMA1 | rs1800875 | T | -- | Decreased IgE, lower risk of a-fib |
| PTPN22 | rs2476601 | A | -- | Increased psoriasis, arthritis, T1D, lupus, urticaria risk |
| IL33 | rs1342326 | A | -- | Increased risk asthma, hay fever |
| IL33 | rs3939286 | T | -- | Increased risk of asthma |
| IL33 | rs928413 | G | -- | Increased risk hay fever, asthma |
| ALDH2 | rs671 | A | -- | Increases mast cell activation |
| PTGS2 | rs4140564 | G | -- | Increased risk osteoarthritis |
| AOC1 | rs10156191 | T | -- | Reduced production of DAO, increased risk of migraines due to histamine |
| AOC1 | rs2052129 | T | -- | Reduced production of DAO, increased risk of migraines due to histamine |
| AOC1 | rs1049742 | T | -- | Reduced production of DAO |
| AOC1 | rs1049793 | G | -- | Reduced production of DAO |
| HNMT | rs1050891 | A | -- | Reduced breakdown of histamine compared to G/G |
| HNMT | rs11558538 | T | -- | Reduced HNMT activity, reduced breakdown of histamine |
| HNMT | i3000469 | T | -- | Reduced HNMT activity, reduced breakdown of histamine |
Histamine Intolerance
Going hand-in-hand with mast cell activation is histamine intolerance. Histamine can be released by mast cells when they are activated. Genetic variants that reduce the breakdown of histamine can result in higher overall histamine levels — and symptoms that range from hives to stomach issues to sinus drainage. Read the article on histamine intolerance for details and references.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| AOC1 | rs10156191 | T | -- | Reduced production of DAO |
| AOC1 | rs2052129 | T | -- | Reduced production of DAO |
| AOC1 | rs1049742 | T | -- | Reduced production of DAO |
| AOC1 | rs1049793 | G | -- | Reduced production of DAO |
| AOC1 | rs2071514 | A | -- | possibly slightly higher DAO |
| HMNT | rs1050891 | A | -- | Reduced breakdown of serum histamine |
| HMNT | i3000469 | T | -- | Reduced breakdown of serum histamine |
| HMNT | rs2071048 | T | -- | T/T: Reduced breakdown of serum histamine (common) |
| HMNT | rs11558538 | T | -- | Reduced breakdown of serum histamine |
| HDC | rs2073440 | G | -- | Decreased histamine production |
| HDC | rs267606861 | A | -- | rare pathogenic mutation, linked to Tourettes |
| HRH1 | rs901865 | T | -- | Increased H1 receptor, increased asthma risk |
| HRH2 | rs2067474 | A | -- | Decreased H2 receptor |
| HRH4 | rs11662595 | G | -- | decreased HRH4 activation (receptor dysfunction), increased risk of progression in non-small cell lung cancer |
| MTHFR | rs1801133 | A | -- | MTHFR C677T, decreased enzyme function, affects methylation cycle |
| MTHFR | rs1801131 | G | -- | MTHFR A1298C, slightly decreased enzyme function, slightly affects methylation cycle |
Fibrinogen: Forming blood clots
Microclots and excessive platelet activation may occur in some people when exposed to the spike protein. Fibrinogen is essential to clotting, and genetic variants in these genes can increase or decrease clot formation. Read the article on fibrinogen and clotting for details and references.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| FGA | rs6050 | C | -- | Increased risk of stroke, DVT, heart disease |
| FGA | rs2070022 | A | -- | Decreased fibrinogen, lower clot risk |
| FGB | rs1800787 | T | -- | Increased fibrinogen, incr. stroke risk |
| FGB | rs1800789 | A | -- | Increased fibrinogen, incr. stroke risk |
| FGB | rs1800790 | A | -- | Increased fibrinogen, incr. stroke risk |
| FGG | rs2066865 | A | -- | Increased fibrinogen; increased risk for DVT |
| FGG | rs2066860 | T | -- | Slightly increased risk of DVT |
Genetic variants that increase the risk of blood clots.
While not specific to microclots and the spike protein, the following genetic variants are linked to a greater risk of deep vein thrombosis or other clot-related problems. Even if this isn’t the answer for your long Spike problems, take this information as a ‘heads up’ not to ignore the signs of a blood clot. Read the full article on blood clots if you have any of these variants.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| F2 | rs1799963 | A | -- | Increased risk of blood clots, increased risk of stroke with PFO |
| F2 | i3002432 | A | -- | Increased risk of blood clots, increased risk of stroke with PFO |
| F5 | rs6025 | T | -- | factor V Leiden; increased risk of clots, DVT |
| ITGB3 | rs5918 | C | -- | PIA1/A2 mutation, increased risk of heart disease, |
| VWF | rs1063856 | C | -- | Likely to have increased Von Willebrand factor, slightly increased risk of blood clots |
| VWF | rs1063857 | G | -- | Likely to have increased Von Willebrand factor, slightly increased risk of blood clots |
| GP6 | rs1613662 | G | -- | increased platelet stickiness |
| F11 | rs2036914 | C | -- | C/C: increased risk of venous thrombosis, thromboembolism |
Lipoprotein (a) levels and clots:
Several studies show that Covid-19 blood clots are linked to higher lipoprotein(a) levels. While Lp(a) levels tend to rise during inflammatory events, people with higher baseline Lp(a) may be at an increased risk for clotting issues. Read the full lipoprotein(a) article if you have the first two variants below.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| LPA | rs3798220 | C | -- | risk of elevated Lp(a), increased risk for heart disease (important) |
| LPA | rs10455872 | G | -- | risk of elevated Lp(a), increased risk for heart disease (important) |
| LPA | rs6919346 | T | -- | decreased Lp(a) |
| LPA | rs41272114 | T | -- | decreased Lp(a) |
| LPA | rs143431368 | C | -- | decreased Lp(a) |
| LPA | rs6415084 | T | -- | higher Lp(a) levels, increased risk of heart disease (Chinese population group); no increased risk in Iranian or European Caucasian populations |
Inflammation: Genetic variants related to chronic inflammation
Some genetic variants increase the cellular production of inflammatory cytokines. While this can be beneficial for fighting off pathogens, the chronic elevation of inflammatory cytokines is seen in patients with long Spike. Knowing where your genetic susceptibility lies may help you focus on the right ways to decrease inflammation for you. Read the article on inflammation for details and references.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| TNF | rs1800629 | A | -- | Higher TNF levels, increased risk of many chronic inflammatory conditions |
| TNF | rs361525 | A | -- | Higher TNF levels, increased risk of many chronic inflammatory conditions |
| IL8 | rs4073 | A | -- | A/A: Increased IL8; increased risk of periodontitis, gastritis, Alzheimers, diabetic nephropathy |
| IL6 | rs1800795 | C | -- | C/C: lower risk of gingivitis |
| IL1B | rs16944 | G | -- | G - Typical risk of septic shock; A/A: Increased risk of septic shock |
| IL1B | rs1143634 | A | -- | Increased risk of gingivitis |
| IL1A | rs1800587 | A | -- | Increased IL1A, increased risk of gum disease, tinnitus, acne, hearing loss |
| IL10 | rs1800896 | C | -- | CC: higher IL-10 (usually good!) |
| NLRP3 | rs35829419 | A | -- | Increased susceptibility to several chronic inflammatory diseases. |
| HMGB1 | rs1045411 | T | -- | increased sepsis risk, higher HMGB1 levels in infection; |
| INFG | rs2430561 | A | -- | increased inflammatory and sickness behavior |
| MTHFR | rs1801133 | A | -- | Decreased methyl group production, decreased detoxification of mercury and arsenic, possibly decreased melatonin production |
| GSTM1 | rs366631 | A | -- | AA: GSTM1 null, increased risk of cancer, increased negative effects of smoking |
| GSTO1 | rs4925 | A | -- | Decreased detoxification of arsenic; increased risk of PCOS |
| GSTA1 | rs3957357 | A | -- | Decreased detoxification, increased risk of depression, |
| NFE2L2 | rs6721961 | T | -- | Decreased Nrf2, increased risk of male infertility, increased risk of CVD, |
| AS3MT | rs11191439 | C | -- | Arsenic is more harmful |
| NQO1 | rs1800566 | A | -- | Increased risk of cancer from benzene and smoking, increased risk of Parkinson’s from pesticide exposure |
| SOD1 | rs1041740 | T | -- | Increased ROS, increased risk of kidney problems, heart disease |
| SOD2 | rs5746136 | T | -- | Increased ROS, increased risk of asthma, PCOS |
GST genes
The GST family of genes encodes enzymes important in detoxifying environmental toxicants and oxidative stress utilizing glutathione. One study found that long Covid patients were more likely to have brain fog with GSTM1 null combined with another glutathione-related variant.[ref] The study was small, indicating a possible connection between antioxidant enzymes and long Covid. If you have GST variants below, especially GSTM1 null, read through the full GST article on ways to boost it.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| GSTM1 | rs366631 | A | -- | AA: GSTM1 deletion |
| GSTA1 | rs3957357 | A | -- | Low (AG) or non-functioning (AA) enzyme |
| GSTP1 | rs1695 | G | -- | Somewhat reduce enzyme function |
| GSTO1 | rs4925 | A | -- | Altered enzyme function; increased risk of PCOS |
Tinnitus-related genes
Another side effect many people report with long Spike is tinnitus or ringing in the ears. Tinnitus seems to be related to inflammation or high histamine levels. Read the article on tinnitus for details and possible solutions.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| NFKB1 | rs3774937 | C | -- | Faster progression to hearing loss in Meniere's |
| NFKB1 | rs4648011 | G | -- | Faster progression to hearing loss in Meniere's |
| Inter-gen | rs4947296 | C | -- | Increased risk of Meniere's |
| KCNE1 | rs1805127 | T | -- | Increased risk of Meniere's |
| KCNE3 | rs2270676 | G | -- | Increased risk of Meniere's |
| IL1A | rs1800587 | A | -- | A: lower risk of hearing loss in Meniere's; G/G: (common) Higher risk of sudden hearing loss in Meniere's |
| ADD1 | rs4961 | T | -- | Increased risk of tinnitus |
| IL1A | rs1800587 | A | -- | Lower risk of tinnitus |
| SLC12A2 | rs10089 | T | -- | increased relative risk of tinnitus, especially with mild hearing loss |
| GRM7 | rs11928865 | A | -- | increased relative risk of tinnitus |
Alopecia areata
Hair loss is a frustrating symptom reported by some people with long Spike. Alopecia areata is sudden hair loss due to autoimmune/autoinflammatory causes. Read the article on alopecia areata for details, references, and solutions.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| CTLA4 | rs1024161 | T | -- | Increased risk of alopecia areata |
| CTLA4 | rs231775 | G | -- | Increased risk of several autoimmune diseases; increased risk of alopecia areata |
| PTPN22 | rs2476601 | A | -- | 3 to 4-fold increased risk of alopecia areata |
| HLA | rs660895 | G | -- | HLA-DRB1*0401; increased risk of alopecia areata |
| IL17F | rs763780 | C | -- | CC: increased risk of alopecia areata |
| IL17RA | rs879577 | T | -- | Decreased risk of alopecia areata |
| IL18 | rs1946518 | T | -- | T/T: lower risk of AA |
| IL2 | rs7682241 | T | -- | increased risk of alopecia areata |
| IL2RA | rs3118470 | T | -- | increased risk of alopecia areata |
| MIF | rs755622 | G | -- | Decreased risk of alopecia areata |
| TNF | rs1800629 | A | -- | Higher TNF; increased risk of alopecia areata |
Sudden hearing loss
Another frustrating and impactful symptom that some people report with long Spike is sudden sensorial hearing loss. Read the article on sudden hearing loss for details and references.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| EDN1 | rs5370 | T | -- | Increased risk of sudden sensorineural hearing loss (related to vasoconstriction) |
| F5 | rs6025 | T | -- | Factor V Leiden (clot related), increased risk of SSNHL |
| MTHFR | rs1801133 | A | -- | Increased risk of SSNHL (folate-related) |
| SOD1 | rs4998557 | A | -- | A/A only: increased relative risk of SSNHL |
| IL1R2 | rs4141134 | G | -- | Increased risk of SSNHL |
| UCP2 | rs659366 | T | -- | Increased risk of SSNHL |
| IL6 | rs1800796 | G | -- | Higher IL-6; increased risk of SSHL |
| HSP70 | rs2763979 | T | -- | Increased risk of noise-induced hearing loss |
| CYP1A1 | rs1799814 | T | -- | Increased CYP1A1 activity, increased risk of SSNHL |
Autoimmune diseases in general
The CTLA4 gene encodes an immune system checkpoint. Variants in this gene are linked to increased susceptibility to a number of different autoimmune diseases. If you have a new onset of an autoimmune disease, read through the full article on CTLA4.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| CTLA4 | rs231775 | G | -- | Increased risk of autoimmune diseases |
| CTLA4 | rs3087243 | G | -- | Increased risk of autoimmune diseases |
MTHFR and folate
The variants in the MTHFR gene cause a decrease in the ability to utilize folate. Dietary folate plays an important role in the methylation cycle, and MTHFR variants may mean that you need more folate in your diet for optimal health. How does this apply to long Spike? A very recent study showed that people with MTHFR C677T (below) are prone to endothelial dysfunction due to decreased SIRT1. The researchers found that resveratrol was able to mitigate the effects.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| MTHFR C677T | rs1801133 | A | -- | 40-70% decrease in MTHFR enzyme function (folate metabolism) |
| MTHFR A1298C | rs1801131 | G | -- | 10-20% decrease in MTHFR enzyme function (folate metabolism) |
ME/CFS: genes related to chronic fatigue syndrome
There is a lot of overlap between long Covid and Chronic Fatigue Syndrome. The genetic variants related to ME/CFS may help point you toward solutions for long Spike. Many of these variants are related to autoimmune diseases, immune function, or inflammation. Read more about ME/CFS and these genetic variants.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| PTPN22 | rs2476601 | A | -- | increased risk of autoimmune diseases, increased susceptibility to CFS/ME (in patients with infectious disease onset) |
| CTLA4 | rs3087243 | G | -- | increased risk of autoimmune conditions, decrease CTLA4 expression; increased risk of CFS/ME (patients with infectious disease onset only) |
| TNF | rs1799724 | T | -- | higher TNF-alpha levels, increased susceptibility to CFS/ME |
| INFG | rs2430561 | A | -- | decreased risk of ME/CFS |
| NLRP3 | rs35829419 | A | -- | Increased susceptibility to fatigue / pain after EBV or other viruses |
| NLRP3 | rs121908147 | A | -- | mutation linked to autoinflammatory disease in combo with other genes (rare) |
| TRPM8 | rs11563204 | A | -- | increased risk of CFS/ME (cold, menthol receptor) |
| TRPM3 | rs6560200 | C | -- | CC: common genotype, higher risk of CFS/ME (Naltrexone may work?) |
| TRPM3 | rs1891301 | T | -- | TT: higher risk of CFS/ME |
| CFB | rs4151667 | A | -- | AA: increased risk of CFS/ME |
| CFH | rs1061170 | C | -- | CC: increased risk of AMD, higher immune response; TT: increased risk of CFS/ME |
POTS: changed heart rate when standing
There are several ways that genetic variants can impact the risk of POTS. If you have variants below, read through the POTS article to understand the different mechanisms at work here.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| SLC6A2 | rs7194256 | T | -- | Increased risk of POTS |
| GNB3 | rs5443 | T | -- | Increased risk of POTS |
| NOS3 | rs2070744 | C | -- | CC: Decreased Risk of POTS |
| ADRB2 | rs1042713 | A | -- | AA: Increased norepinephrine response |
Tryptophan conversion to kynurenine or serotonin:
Genes play a role in whether you’re likely to utilize tryptophan more for kynurenine or for the serotonin pathway. Read the full tryptophan article for details and graphical explanations.
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| IDO1 | rs3808606 | A | -- | AA only: more conversion to kynurenine |
| IDO1 | rs9657182 | C | -- | probably more conversion to kynurenine |
| KMO | rs1053230 | T | -- | Increased conversion to kynurenine |
| TPH2 | rs4570625 | T | -- | generally decreased risk of depression; less aggressiveness and lower anxiety |
| TPH2 | rs11178997 | A | -- | Increased risk of depression |
| TPH2 | rs1843809 | G | -- | Decreased risk of depression |
| TPH2 | rs4290270 | T | -- | TT only: circadian disruption in people with depression |
| IDO2 | rs10109853 | T | -- | Decreased IDO2 function |
| IDO2 | rs4503083 | A | -- | Decreased IDO2 function |
| IDO1 | rs7820268 | C | -- | C/C: 1.5-fold increased relative risk of MS |
Lifehacks: Research on long Covid possible treatments
Let me reiterate: Talk with your doctor if you have any medical questions. All of this information is just a compilation of research studies, which weren’t done on you. If you are on medications, please talk with your doctor or pharmacist if you have questions on interactions with supplements.
OTC Antihistamines to target histamine/MCAS:
A study showed 72% of long Covid patients had clinically improved symptoms when taking a combination of antihistamines for four weeks. The H1 antihistamines used were either fexofenadine or loratadine, which are both readily available. One of the H2 antihistamines used, famotidine, is also available OTC.[ref]
Theoretical genetic links: This may be more likely to work for someone with histamine intolerance or MCAS variants (above).
Probiotic strains to target gut microbiome:
In a clinical trial, a probiotic and prebiotic formula showed efficacy for improving long Covid symptoms over 30 days. The average age of participants was 53, and the average time of starting the probiotic was 108 days after covid. The probiotic contained 10 billion CFU of Lactobacillus plantarum (Lp90), Lactobacillus rhamnosus (LRa05), Lactobacillus bulgaricus (LB42), Lactococcus lactis (La61), and Lactobacillus paracasei (LC86) along with inulin.[ref]
The study I referenced above shows that the gut microbiome was changed in long Covid patients (tested six months after Covid) and showed a decrease in Bifidobacteria species.[ref] Another study showed that higher levels of Bifidobacterium longum were associated with a significantly decreased risk of long Covid.[ref]
Taken together, these studies may indicate that a probiotic containing Bifidobacterium could help.
Theoretical genetic links: People who don’t secrete their blood type in their saliva and intestinal mucosa are likely to have very low Bifidobacterium levels in their gut microbiome. You can check your genes to see if you are a non-secretor of your blood type.
Luteolin to target neuroinflammation:
Some researchers theorize that luteolin, a natural flavonoid that acts on neuroinflammation, can help with long Spike symptoms.[ref] A clinical trial that included luteolin and palmitoylethanolamide showed improvements in people with olfactory problems after COVID-19.[ref]
Theoretical genetic links: Luteolin for inflammation may benefit people with several chronic inflammation variants (above).
Related article: Luteolin: anti-inflammatory and neuroprotective
Melatonin for overall immune support:
More than just a sleep hormone, melatonin is also a potent intracellular antioxidant. It also enhances the immune response to viruses in the acute phase of infection. Researchers theorize that several mechanisms of action would benefit anyone with long Covid. (clinical trials are needed here)[ref] If you are considering supplemental melatonin, the timed-release formulas better mimic natural production. Additionally, you may want to start with a low dose and then increase it as you get used to it.
Theoretical genetic links: While many genes are involved in melatonin creation and use, this pathway starts with serotonin being made from tryptophan. If you have variants that promote kynurenine production over serotonin, you may find that melatonin supplementation would be worth considering.
Related article: Supplemental Melatonin: Immune System Superstar
3CL protease inhibitor for continued viral replication:
For persistent SARS-CoV-2 viral infections, a 3CL protease inhibitor may be beneficial for stopping viral replication. Tollovid is a nutraceutical produced by Todos Medical and available on their website or on Amazon (expensive…). Tolovid contains Gromwell Root (Lithospermum erythrorhizon), which is a traditional Chinese herbal medicine known for its ability to inhibit certain viruses and heal bacterial skin infections. The major bioactive component is shikonin.[ref][ref][ref]
EGCG to block spike protein binding:
EGCG, a component of green tea, inhibits spike binding to the ACE2 receptor and also blocks replication.[ref] Additionally, EGCG is a natural HSP90 inhibitor (see info above on inhibiting HSP90 to block spike protein-induced endothelial barrier dysfunction).[ref]
Related article: Heat Shock Proteins
Oxaloacetate for mitochondrial ATP production:
A metabolite in the Krebs cycle, oxaloacetate, is part of how mitochondria provide energy to cells. Supplemental oxaloacetate was given as a nutritional supplement to patients with ME/CFS or long Covid. Both groups showed a reduction in physical and mental fatigue.[ref]
Aromatherapy for fatigue?
A study using essential oils (thyme, orange, clove bud, and frankincense) found that smelling the oils improved fatigue scores in women who were still tired after Covid.[ref] I included this because it is one of the few clinical trials that has been completed and published…
Nicotinamide riboside?
A new clinical trial is starting to see if nicotinamide riboside (NR) helps with long Covid.[ref] Mechanistically, it makes sense that NR would help boost overall cellular resilience. (Read more about NR and NAD+)
Theoretical genetic links: When looking at NR or NAD+, another consideration may be the tryptophan/kynurenine pathway (genes above). Cells tend to shift tryptophan towards the kynurenine pathway when niacin/nicotinamide is low. If you have a genetic propensity toward producing more kynurenine, you may want to consider whether supplement NR – or – supplemental niacin would be worth trying.
Prescription medications:
Researchers conducted a clinical trial with 18 ‘long haul’ Covid patients. The treatment used was a combination of 300 mg/ twice a day of maraviroc and 10mg/day of pravastatin. Maraviroc is a prescription medication used in HIV infections. It is a CCR5 antagonist. Pravastatin is a statin (traditionally used as a cholesterol-lowering medication). After 6 to 12 weeks of treatment, symptoms improved enough to stop the medications in the long Covid patients.[ref]
Conclusion:
I started this article thinking it would be an easy one to write — simply explain that the spike protein causes damage to cells, which in turn causes persistent symptoms from tissue damage or immune system activation. It would apply to mRNA vaccines or SAR-CoV-2 infection.
Along the way, I found studies that made me question a lot that I thought I knew.
The study showing that the SARS-CoV-2 virus could replicate in gut bacterial cells, without needing human cells, still blows my mind.[ref] In my opinion, this line of research needs to be replicated and expanded upon.
The animal studies showing that the lipid nanoparticles alone without the mRNA can cause huge spikes in inflammatory cytokines when injected into animals that already have inflammation going on — well, that made me wonder if the combination of the lipid nanoparticles, mRNA, and chronic inflammatory conditions (autoimmune, arthritis, diabetes, heart disease) could be the crux of the issue. Maybe it isn’t the spike protein by itself?[ref] It could be the lipid nanoparticle instead.[ref]. But the title “long lipid nanoparticle inflammation” doesn’t roll off the tongue like “long Spike”.
I’m dismayed at the lack of clinical trials for treating long Covid. Along the same lines, the mainstream media articles portraying long Covid as being ‘all in their heads’ is reminiscent of how other chronic illnesses such as ME/CFS or fibromyalgia have been portrayed for decades.
For anyone reading this dealing with ‘long Spike’, I want to leave you with the encouragement that research shows that it is real. But that, realistically, treatments based on clinical trials are lacking. I don’t think this is a problem that a single pill will fix for everyone. A multi-faceted, individualized approach to restoring health is likely needed.
References:
Aird, William C. “Endothelium as an Organ System.” Critical Care Medicine, vol. 32, no. 5 Suppl, May 2004, pp. S271-279. PubMed, https://doi.org/10.1097/01.ccm.0000129669.21649.40.
Bellone, Maria Laura, et al. “Production in Escherichia Coli of Recombinant COVID-19 Spike Protein Fragments Fused to CRM197.” Biochemical and Biophysical Research Communications, vol. 558, June 2021, pp. 79–85. PubMed, https://doi.org/10.1016/j.bbrc.2021.04.056.
Briggs, Selena E., et al. “Sudden Sensorineural Hearing Loss and COVID-19 Vaccination Revisited—An Ongoing Conversation.” JAMA Otolaryngology–Head & Neck Surgery, June 2022. Silverchair, https://doi.org/10.1001/jamaoto.2022.1572.
Ceban, Felicia, et al. “Fatigue and Cognitive Impairment in Post-COVID-19 Syndrome: A Systematic Review and Meta-Analysis.” Brain, Behavior, and Immunity, vol. 101, Mar. 2022, pp. 93–135. PubMed, https://doi.org/10.1016/j.bbi.2021.12.020.
Chan, Leon Y., et al. “Non-Invasive Measurement of MRNA Decay Reveals Translation Initiation as the Major Determinant of MRNA Stability.” ELife, vol. 7, p. e32536. PubMed Central, https://doi.org/10.7554/eLife.32536. Accessed 9 Aug. 2022.
Choi, Sangjoon, et al. “Myocarditis-Induced Sudden Death after BNT162b2 MRNA COVID-19 Vaccination in Korea: Case Report Focusing on Histopathological Findings.” Journal of Korean Medical Science, vol. 36, no. 40, July 2021, p. e286. PubMed Central, https://doi.org/10.3346/jkms.2021.36.e286.
Colunga Biancatelli, Ruben M. L., et al. “The SARS-CoV-2 Spike Protein Subunit S1 Induces COVID-19-like Acute Lung Injury in Κ18-HACE2 Transgenic Mice and Barrier Dysfunction in Human Endothelial Cells.” American Journal of Physiology. Lung Cellular and Molecular Physiology, vol. 321, no. 2, Aug. 2021, pp. L477–84. PubMed, https://doi.org/10.1152/ajplung.00223.2021.
Doi, Kazuma, et al. “Cervical Transverse Myelitis Following COVID-19 Vaccination.” NMC Case Report Journal, vol. 9, 2022, pp. 145–49. PubMed, https://doi.org/10.2176/jns-nmc.2022-0045.
Dressen, Bri. 1250+ COVID Vaccine Publications and Case Reports. 9 July 2022, https://react19.org/1250-covid-vaccine-reports/.
Ellul, Pierre, et al. “Implementation and Short-Term Adverse Events of Anti-SARS-CoV-2 Vaccines in Inflammatory Bowel Disease Patients: An International Web-Based Survey.” Journal of Crohn’s & Colitis, vol. 16, no. 7, Aug. 2022, pp. 1070–78. PubMed, https://doi.org/10.1093/ecco-jcc/jjac010.
Eren, Fettah, et al. “Multifocal Motor Neuropathy after SARS-CoV-2 Vaccination: A Causal or Coincidental Association?” The Journal of International Medical Research, vol. 50, no. 7, July 2022, p. 3000605221110709. PubMed, https://doi.org/10.1177/03000605221110709.
Foladori, Paola, et al. “Coronaviruses and SARS-CoV-2 in Sewerage and Their Removal: Step by Step in Wastewater Treatment Plants.” Environmental Research, vol. 207, May 2022, p. 112204. PubMed, https://doi.org/10.1016/j.envres.2021.112204.
Germano, Francesco, et al. “COVID-19 Vaccine-Related Guillain-Barré Syndrome in the Liguria Region of Italy: A Multicenter Case Series.” Journal of the Neurological Sciences, vol. 440, June 2022, p. 120330. PubMed, https://doi.org/10.1016/j.jns.2022.120330.
González-Enríquez, José Octavio. “[Bell’s Palsy Secondary to COVID-19 Vaccine Pfizer: Case report].” Revista Medica Del Instituto Mexicano Del Seguro Social, vol. 60, no. 2, Mar. 2022, pp. 224–28.
Grandjean, Dominique, et al. Screening for SARS-CoV-2 Persistence in Long COVID Patients Using Sniffer Dogs and Scents from Axillary Sweats Samples. 12 Jan. 2022. medRxiv, https://doi.org/10.1101/2022.01.11.21268036.
Gutiérrez-Castrellón, Pedro, et al. “Probiotic Improves Symptomatic and Viral Clearance in Covid19 Outpatients: A Randomized, Quadruple-Blinded, Placebo-Controlled Trial.” Gut Microbes, vol. 14, no. 1, p. 2018899. PubMed Central, https://doi.org/10.1080/19490976.2021.2018899. Accessed 9 Aug. 2022.
Heinz, Franz X., and Karin Stiasny. “Distinguishing Features of Current COVID-19 Vaccines: Knowns and Unknowns of Antigen Presentation and Modes of Action.” NPJ Vaccines, vol. 6, Aug. 2021, p. 104. PubMed Central, https://doi.org/10.1038/s41541-021-00369-6.
Lessans, Naama, et al. “The Effect of BNT 162b2 SARS‐C o V ‐2 m RNA Vaccine on Menstrual Cycle Symptoms in Healthy Women.” International Journal of Gynecology & Obstetrics, Aug. 2022, p. ijgo.14356. DOI.org (Crossref), https://doi.org/10.1002/ijgo.14356.
Li, Can, et al. “Intravenous Injection of Coronavirus Disease 2019 (COVID-19) MRNA Vaccine Can Induce Acute Myopericarditis in Mouse Model.” Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America, vol. 74, no. 11, Aug. 2021, pp. 1933–50. PubMed Central, https://doi.org/10.1093/cid/ciab707.
Littlefield, Katherine M., et al. “SARS-CoV-2-Specific T Cells Associate with Inflammation and Reduced Lung Function in Pulmonary Post-Acute Sequalae of SARS-CoV-2.” PLOS Pathogens, vol. 18, no. 5, May 2022, p. e1010359. PLoS Journals, https://doi.org/10.1371/journal.ppat.1010359.
Liu, Qin, et al. “Gut Microbiota Dynamics in a Prospective Cohort of Patients with Post-Acute COVID-19 Syndrome.” Gut, vol. 71, no. 3, Mar. 2022, pp. 544–52. gut.bmj.com, https://doi.org/10.1136/gutjnl-2021-325989.
Long, Hui, et al. “Prolonged Viral Shedding of SARS-CoV-2 and Related Factors in Symptomatic COVID-19 Patients: A Prospective Study.” BMC Infectious Diseases, vol. 21, no. 1, Dec. 2021, p. 1282. BioMed Central, https://doi.org/10.1186/s12879-021-07002-w.
Luo, Chongliang, et al. “Comparability of Clinical Trials and Spontaneous Reporting Data Regarding COVID-19 Vaccine Safety.” Scientific Reports, vol. 12, June 2022, p. 10946. PubMed Central, https://doi.org/10.1038/s41598-022-13809-7.
Mevorach, Dror, et al. “Myocarditis after BNT162b2 MRNA Vaccine against Covid-19 in Israel.” The New England Journal of Medicine, vol. 385, no. 23, Dec. 2021, pp. 2140–49. PubMed, https://doi.org/10.1056/NEJMoa2109730.
Meyer, Keith, et al. “SARS-CoV-2 Spike Protein Induces Paracrine Senescence and Leukocyte Adhesion in Endothelial Cells.” Journal of Virology, edited by Tom Gallagher, vol. 95, no. 17, Aug. 2021, pp. e00794-21. DOI.org (Crossref), https://doi.org/10.1128/JVI.00794-21.
Ng, Siew C., et al. “Gut Microbiota Composition Is Associated with SARS-CoV-2 Vaccine Immunogenicity and Adverse Events.” Gut, vol. 71, no. 6, June 2022, pp. 1106–16. gut.bmj.com, https://doi.org/10.1136/gutjnl-2021-326563.
Parrino, Daniela, et al. “Tinnitus Following COVID-19 Vaccination: Report of Three Cases.” International Journal of Audiology, vol. 61, no. 6, June 2022, pp. 526–29. PubMed, https://doi.org/10.1080/14992027.2021.1931969.
Patone, Martina, et al. “Neurological Complications after First Dose of COVID-19 Vaccines and SARS-CoV-2 Infection.” Nature Medicine, vol. 27, no. 12, 2021, pp. 2144–53. PubMed Central, https://doi.org/10.1038/s41591-021-01556-7.
Perez, Yalile, et al. “Myocarditis Following COVID-19 MRNA Vaccine: A Case Series and Incidence Rate Determination.” Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America, Nov. 2021, p. ciab926. PubMed, https://doi.org/10.1093/cid/ciab926.
Petrillo, Mauro, et al. “Increase of SARS-CoV-2 RNA Load in Faecal Samples Prompts for Rethinking of SARS-CoV-2 Biology and COVID-19 Epidemiology.” F1000Research, vol. 10, July 2021, p. 370. PubMed Central, https://doi.org/10.12688/f1000research.52540.3.
Pokryszka, Jagoda, et al. “Course of Fecal Calprotectin after MRNA SARS-CoV-2 Vaccination in Patients with Inflammatory Bowel Diseases.” Vaccines, vol. 10, no. 5, May 2022, p. 759. PubMed Central, https://doi.org/10.3390/vaccines10050759.
Ponchon, Luc, et al. “Co-Expression of RNA–Protein Complexes in Escherichia Coli and Applications to RNA Biology.” Nucleic Acids Research, vol. 41, no. 15, Aug. 2013, p. e150. PubMed Central, https://doi.org/10.1093/nar/gkt576.
Prado, Mario B., and Karen Joy B. Adiao. “Facial Diplegia as the Sole Manifestation of Post-Vaccination Guillain-Barre Syndrome: A Case Report and Literature Review.” The Neurohospitalist, vol. 12, no. 3, July 2022, pp. 508–11. PubMed, https://doi.org/10.1177/19418744221097350.
Prakash, Shantanu, et al. “SARS-CoV-2 -RNA Persists Longer in Faecal Sample as Compared to Nasal and Throat Swab Samples of COVID-19 Patients’; an Observational Study.” Indian Journal of Medical Microbiology, vol. 39, no. 1, Jan. 2021, pp. 122–24. PubMed, https://doi.org/10.1016/j.ijmmb.2020.10.012.
Robertson, John L., et al. “Alterations in the Molecular Composition of COVID-19 Patient Urine, Detected Using Raman Spectroscopic/Computational Analysis.” PLOS ONE, vol. 17, no. 7, July 2022, p. e0270914. PLoS Journals, https://doi.org/10.1371/journal.pone.0270914.
Röltgen, Katharina, et al. “Immune Imprinting, Breadth of Variant Recognition, and Germinal Center Response in Human SARS-CoV-2 Infection and Vaccination.” Cell, vol. 185, no. 6, Mar. 2022, pp. 1025-1040.e14. www.cell.com, https://doi.org/10.1016/j.cell.2022.01.018.
Safavi, Farinaz, et al. Neuropathic Symptoms with SARS-CoV-2 Vaccination. 17 May 2022. medRxiv, https://doi.org/10.1101/2022.05.16.22274439.
Santinelli, Letizia, et al. “Oral Bacteriotherapy Reduces the Occurrence of Chronic Fatigue in COVID-19 Patients.” Frontiers in Nutrition, vol. 8, 2022. Frontiers, https://www.frontiersin.org/articles/10.3389/fnut.2021.756177.
SARS-CoV-2 Infection and Persistence throughout the Human Body and Brain. 20 Dec. 2021, https://doi.org/10.21203/rs.3.rs-1139035/v1.
Serra-Compte, Albert, et al. “Elimination of SARS-CoV-2 along Wastewater and Sludge Treatment Processes.” Water Research, vol. 202, Sept. 2021, p. 117435. PubMed Central, https://doi.org/10.1016/j.watres.2021.117435.
Su, Qi, et al. “Post-Acute COVID-19 Syndrome and Gut Dysbiosis Linger beyond 1 Year after SARS-CoV-2 Clearance.” Gut, Aug. 2022. gut.bmj.com, https://doi.org/10.1136/gutjnl-2022-328319.
Swank, Zoe, et al. Persistent Circulating SARS-CoV-2 Spike Is Associated with Post-Acute COVID-19 Sequelae. 16 June 2022. medRxiv, https://doi.org/10.1101/2022.06.14.22276401.
The Vaccine Adverse Event Reporting System (VAERS) Request. https://wonder.cdc.gov/vaers.html. Accessed 9 Aug. 2022.
Traylen, Christopher M., et al. “Virus Reactivation: A Panoramic View in Human Infections.” Future Virology, vol. 6, no. 4, Apr. 2011, pp. 451–63. PubMed Central, https://doi.org/10.2217/fvl.11.21.
Trougakos, Ioannis P., et al. “Adverse Effects of COVID-19 MRNA Vaccines: The Spike Hypothesis.” Trends in Molecular Medicine, vol. 28, no. 7, July 2022, pp. 542–54. www.cell.com, https://doi.org/10.1016/j.molmed.2022.04.007.
Turner, Jackson S., et al. “SARS-CoV-2 Viral RNA Shedding for More Than 87 Days in an Individual With an Impaired CD8+ T Cell Response.” Frontiers in Immunology, vol. 11, 2021. Frontiers, https://www.frontiersin.org/articles/10.3389/fimmu.2020.618402.
Uehara, Osamu, et al. “Alterations in the Oral Microbiome of Individuals with a Healthy Oral Environment Following COVID-19 Vaccination.” BMC Oral Health, vol. 22, no. 1, Mar. 2022, p. 50. BioMed Central, https://doi.org/10.1186/s12903-022-02093-6.
Waheed, Waqar, et al. “Post COVID‐19 Vaccine Small Fiber Neuropathy.” Muscle & Nerve, vol. 64, no. 1, July 2021, pp. E1–2. PubMed Central, https://doi.org/10.1002/mus.27251.
Wang, Jing, and Bo Han. “Dysregulated CD4+ T Cells and MicroRNAs in Myocarditis.” Frontiers in Immunology, vol. 11, Mar. 2020, p. 539. PubMed Central, https://doi.org/10.3389/fimmu.2020.00539.
Zerbato, Verena, et al. “High Fecal Calprotectin Levels Are Associated with SARS-CoV-2 Intestinal Shedding in COVID-19 Patients: A Proof-of-Concept Study.” World Journal of Gastroenterology, vol. 27, no. 22, June 2021, pp. 3130–37. PubMed, https://doi.org/10.3748/wjg.v27.i22.3130.
Zuo, Tao, et al. “Temporal Landscape of Human Gut RNA and DNA Virome in SARS-CoV-2 Infection and Severity.” Microbiome, vol. 9, Apr. 2021, p. 91. PubMed Central, https://doi.org/10.1186/s40168-021-01008-x.